BY CHRISTIE DEL CASTILLO-HEGYI, M.D., Co-Founder of the FEd is Best Foundation
Every patient-healthcare provider relationship is governed by four central principles of medical ethics, which are the following:
- Beneficence – Health care providers have the duty to provide care in a way that benefits a patient, increases their safety, their immediate and long-term health, and their comfort.
- Non-maleficence – First, do no harm. This principle requires that health professionals do not intentionally harm or injure a patient either through acts of commission or omission. If an intervention causes more harm to a patient than doing nothing, you do not intervene.
- Respect for Patient Autonomy – With any health care decision, the patient has the right to full disclosure of the risks and benefits of any intervention, regardless of how rare, so that they may act in their own or their children’s best interests to get the best outcomes with the least risk involved. Patient autonomy can only be fully realized if they are given honest and complete information on any and all the risks and benefits, whether common or rare, so that they may voluntarily choose, free of coaxing or coercion, in order to optimize their own or their children’s health outcomes.
- Respect for Human Rights – In 1948, the United Nations published the Universal Declaration of Human Rights, which subsequently charged governments, doctors and health workers to protect the human rights and human dignity of all people. It provides special protection of the physical integrity of those who are unable to consent, which includes children. These human rights include the right to food and water to prevent starvation and the associated injury to the brain and vital organs.
The Baby-Friendly Hospital Initiative has violated all four of these core principles of medical ethics through its policies and has reiterated its commitment to defending its dangerous policies over their commitment to patient safety in their recent dismissive response to Landon Johnson’s accidental starvation death caused by the Baby-Friendly policies.

Landon Johnson, son of Jillian and Jarrod Johnson, developed cardiac arrest from hypernatremic dehydration 12 hours after being discharged from a Baby-Friendly Hospital despite days of crying and non-stop breastfeeding in the hospital, which she was told was normal. He died at 19 days old.
BENEFICENCE
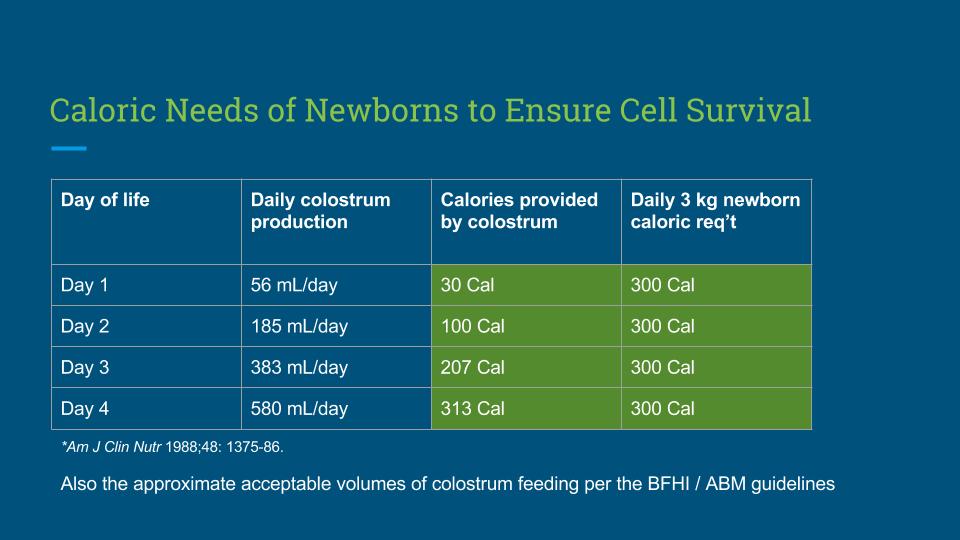
The first core principle of medicine is the duty to provide care that benefits a patient’s immediate and long-term health, their safety and comfort. The Baby-Friendly exclusive breastfeeding guidelines have made it a policy to feed newborn babies only colostrum in the first days of life while pressuring mothers to avoid supplementation when their babies are showing obvious signs of hunger and starvation. They declare that colostrum is enough despite scientific evidence that the average mother’s colostrum, the same amount that is accepted as sufficient by their policies, provides only a tenth to 2/3rds of an average newborn baby’s caloric requirement in the first 3 days before full milk production.
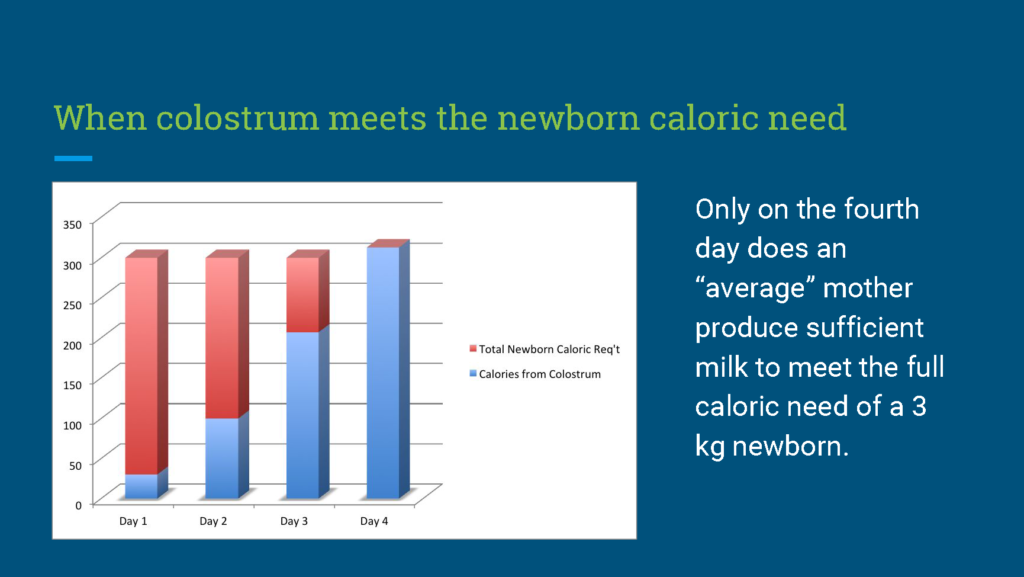
Caloric needs of newborns is 100 Cal/kg/day: Ben, X.-M. (2008). World Journal of Gastroenterology 14, 6133. Average Colostrum Production of Mothers: Neville, M.C., et al. (1988). Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am. J. Clin. Nutr. 48, 1375–1386. Caloric content of colostrum is 54 Cal/100mL: Gidrewicz, D.A., and Fenton, T.R. (2014). A systematic review and meta-analysis of the nutrient content of preterm and term breast milk. BMC Pediatrics 14, 216.
They failed to research the actual nutritional requirements of newborn babies and the actual caloric yield of a mother’s colostrum and have declared that a newborn can sustain 3 days of fasting conditions without serious harm to their vital organs and brain without any scientific evidence. They failed to provide any data on the safety of allowing newborns to fast from colostrum-only feeding and have watched baby after newborn baby cry for hours to days for milk in their mother-baby units until they developed lethargy and even brain injury from caloric and fluid deprivation. They have created non-threatening sounding names for their extreme hunger and thirst like “clusterfeeding” and “Second Night Syndrome.” They have created an alternative world where babies who are losing weight, getting a fraction of their caloric requirement and producing minimal urine are experiencing “fluid shifts” and “diuresis,” instead of the more accurate terms of “fasting” and “fluid-deprivation.” Allowing a child to go hungry for hours to days fails to protect their safety, their comfort, and their short- and long-term health outcomes.
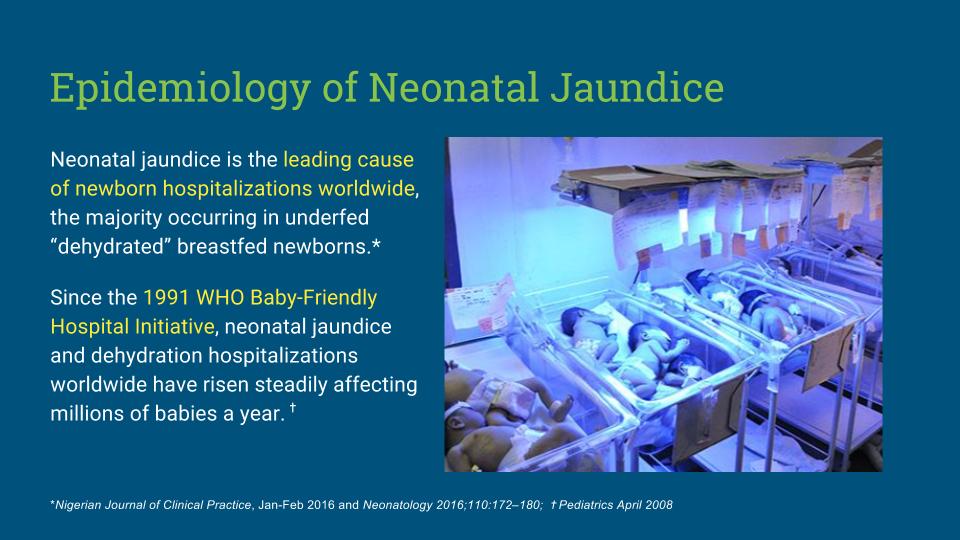
Because of the unwillingness of the Baby-Friendly Hospital Initiative to publicly admit the mistakes of their original authors or to inform the public about the common and dangerous conditions associated with their protocol, the most common causes of newborn hospitalization in the U.S. and the rest of the world are hyperbilirubinemia (excessive jaundice), “feeding problems,” and dehydration, all starvation-related conditions that would have been prevented had the mother been left alone to respond to her instincts to feed her child. Bilirubin-induced brain injury, a known complication of exclusive breastfeeding of newborns, is one of the leading causes of perinatal brain injury and disability in the world and mothers are rarely informed of these known risks. The BFHI states that their exclusive breastfeeding policies are safe without ever having provided research proving so. Meanwhile, decades of scientific evidence has documented that exclusively breastfed newborns are at greater risk of starvation-related jaundice, dehydration, hypoglycemia, brain injury and death compared to their supplemented counterparts.
NON-MALEFICENCE – DO NO HARM.
A baby left to a mother and her family to be breastfed and supplemented on pure instinct would likely be safer than a child experiencing the Baby-Friendly protocol. When a feeding policy’s primary goal is exclusive breastfeeding at discharge while the vast majority of mothers cannot produce the calories and fluid required to keep their babies from fasting, the hospital policy is causing harm. When that feeding policy tolerates a child crying for milk for hours to days as they breastfeed non-stop for survival, the hospital policy is also causing harm.
Prior to the Baby-Friendly exclusive breastfeeding protocol, in countries where breastfeeding was the primary mode of infant feeding, newborn babies were near-universally supplemented with “prelacteal feeding” in the first days of life. Despite these early supplemental feedings, the vast majority of babies were breastfed for 1-2 years without ever experiencing the fasting conditions imposed by the Baby-Friendly protocol.
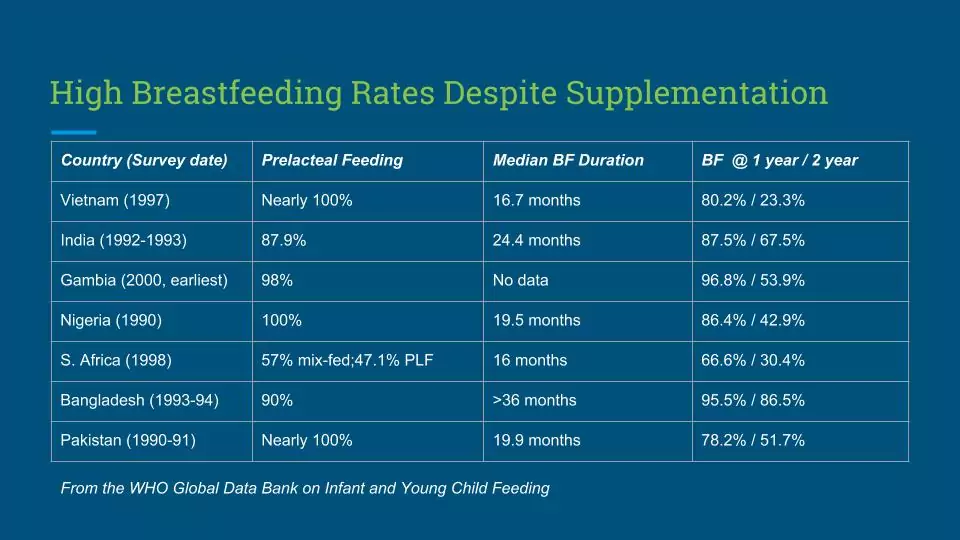
From the WHO Global Data Bank on Infant and Young Child Feeding and the Epidemiological Literature on Prelacteal Feeding (see references below)
This historical evidence shows that we actually evolved to supplement breastfeeding when the baby showed obvious signs that breast milk was not enough and that mother-led supplementation actually protected newborns from starvation-related brain-injury and death. Finding alternatives to breast milk was an advantageous human evolution, which the BFHI has successfully erased from our collective knowledge in their campaign to demonize formula. How did we feed our babies before the exclusive breastfeeding guidelines? We used our instincts and it turns out that that was far safer than following the untested thresholds for supplementation of the BFHI and Academy of Breastfeeding Medicine guidelines. According to my communications with world-renowned newborn jaundice epidemiologist, Dr. Bolajoko Olusanya, in developing countries without sufficient healthcare resources, many babies do not have the privilege of being born in the hospital nor do they get monitored as they fast from exclusive colostrum-feeding. Newborns who starve from exclusive breastfeeding either die at home or survive disabled from jaundice, which would have been prevented had their mothers been allowed to follow their own instincts to feed. According to Dr. Olusanya, 1.1 million newborns a year experience severe jaundice, and attributes it partially to the prevalence of G6PD which causes exaggerated jaundice, but mostly to starvation-related jaundice (non-hemolytic jaundice) caused by widespread early exclusive breastfeeding. 114 ,000 of these babies die each year from their severe jaundice. We did no favors to breastfeeding mothers in developing countries by “re-educating” them in the first-world’s version of breastfeeding. They were better off without our intervention.
Meanwhile, the most recent scientific research on colostrum has now proven that the calories and fluid provided by the average mother are not sufficient to keep a child from fasting for several days. Prior to the BFHI guidelines, it was widely and correctly believed that the breast milk of mothers in the first days of life was inadequate to meet the nutritional needs of the newborn child and therefore they were fed alternatives including the milk of wet nurses, sugar water and animal milk. These supplemental feedings were instinctively used by mothers to protect her child from starvation and were used by doctors to prevent the known complications of starvation including dehydration, jaundice and hypoglycemia. These supplemental feedings were discouraged by WHO and UNICEF with the incorrect and now disproven belief that a newborn child can tolerate days of fasting without permanent injury.
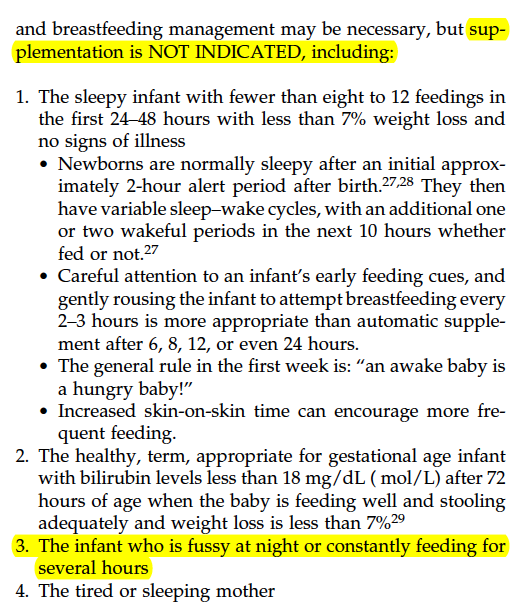
The 2009 Academy of Breastfeeding Medicine Guidelines followed by the Baby-Friendly Hospital Initiative that were in place at the time of Landon Johnson’s death. Fussing and constant feeding for several hours, both obvious signs of newborn starvation, are not indications for supplementation.
The Baby-Friendly policy on supplementation, as written by the Academy of Breastfeeding Medicine, in both their 2009 version and their most recently published 2017 version, states specifically that “a baby that is fussing or nursing for hours,” also known as clusterfeeding, is NOT an indication for supplementation, which are obvious signs of hunger and starvation from insufficient breast milk intake. In their most recent version, they fail to define what “abnormal” vs. “normal” clusterfeeding is and have effectively made no changes to their policy of tolerating prolonged breastfeeding of newborns. Denying supplementation to a child who is clearly communicating their need for additional milk is by definition causing harm to that child. Landon Johnson was showing these signs of hunger for 2.5 days while in a Baby-Friendly hospital before he died of cardiac arrest from hypernatremic dehydration shortly after discharge. His mother was reassured, per policy, over and over, that he was getting enough and did not need supplementation until it was blatantly obvious that he had not received enough. Jill, his mother, was not informed of the risks of accidental starvation to her child while following their guidelines; nor have the millions of mothers who have watched their newborns cry non-stop for days until they were lethargic, needed IV fluids, glucose, phototherapy, hospitalization AND rescue supplementation. By the time their children developed lethargy, the scientific literature has uncovered that they may have already developed debilitating levels of brain injury on MRI and EEG (the diagnostic test for seizures). While most babies will survive the acute starvation once they are given enough calories and fluid, many are likely to develop long-term cognitive declines and long-term disability.
RESPECT FOR PATIENT AUTONOMY
A patient has the right to know all the risks and benefits related to health-care decisions regardless of how rare they are. In the case of starvation-related complications related to the Baby-Friendly exclusive breastfeeding guidelines, the complications are in fact the most common causes of newborn hospitalization in the world. It is the policy of the Baby-Friendly Hospital Initiative to inform mothers of the risks of formula supplementation while hiding the risks of starvation from exclusive breastfeeding including jaundice, dehydration, hypoglycemia, permanent brain injury and death.
Patient autonomy can only be fully realized if mothers are given honest and complete information on any and all the risks of their healthcare decisions so that they may voluntarily choose, free of coaxing or coercion, in order to optimize their children’s health outcomes while minimizing the risks. This ethical standard has been widely violated by the BFHI as health professionals have been trained to pressure mothers to exclusively breastfeed without informing them of the known risks of withholding supplementation from their newborn babies. Mothers have been ignored or denied supplementation for their inconsolable babies by health professionals, even when they are requesting it, as it compromises the hospital’s rates of exclusive breastfeeding at discharge, the primary goal of the BFHI. We have received reports from nurses and doctors who have been written up and disciplined for offering supplementation or for checking glucose levels on babies who showed clear signs of distress from hunger and starvation.
Pressuring patients to follow exclusive breastfeeding guidelines while hiding common brain- and life-threatening complications associated with them constitutes frank criminal medical negligence by the Baby-Friendly Hospital Initiative and the health organizations and hospitals that endorse it.
RESPECT FOR HUMAN RIGHTS
The final and most important ethical standard of medicine violated by the Baby-Friendly Hospital Initiative is the duty to protect the human right of the newborn to food and water. Providing a child a fraction of their caloric and fluid requirements while watching them cry for days out of hunger and thirst is a frank violation of their human rights and would not even be allowed by the rules of the Geneva Convention for prisoners of war. For many newborns, they may receive even fewer calories than what is allotted by the BFHI and ABM guidelines as no investigation of milk supply is done until complications happen to the newborn. The mother, in addition, is coaxed and coerced to harm her own newborn by following the guidelines, all while being told incorrect and dangerous ideas about newborn physiology. Only when the harm is obvious is she told that her own actions are what led to her child’s condition. She is subsequently shamed into silence with the knowledge of accidentally starving her child and is commonly blamed for the complications as it is assumed that she was not educated enough in breastfeeding or that her insufficient milk was rare when neither is true. In fact, even if the accepted volumes of colostrum are fed to a newborn, that child can still starve because they are by definition fasting until a mother’s milk comes in.
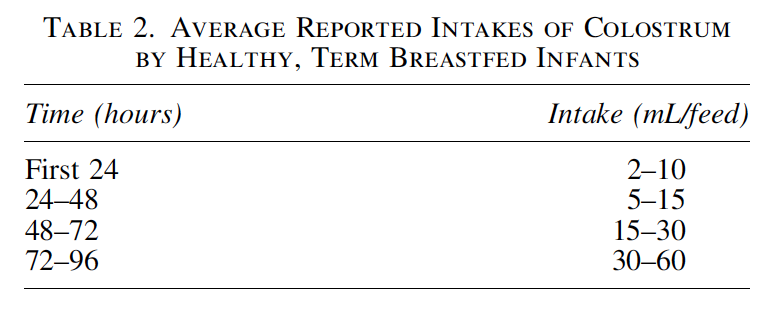
Average accepted volumes of colostrum deemed to be sufficient to meet a newborn’s nutritional needs according to the ABM and the BFHI. A volume of 2-30 mL/feed if given 12 times provides 4-65% of a 3 kg newborn’s caloric needs for the first 3 days of life. Many mothers produce even less than these volumes, which can cause worse fasting conditions for her newborn.
THE MISSION OF THE FED IS BEST FOUNDATION
It is the mission of the Fed is Best Foundation to develop safe infant feeding guidelines in order to support every family to safely feed their babies, through breastfeeding, combination feeding, formula-feeding and tube feeding. The BFHI guidelines are 25 years old, has no data on safety and decades of data showing that their policies expose exclusively breastfed newborns to unnecessary and preventable complications that can cause irreversible harm. We promote breastfeeding while making sure a child is safely fed what they need to not be harmed until a mother’s milk supply and the dyad’s breastfeeding skills are able to meet the child’s full needs. We advocate for the protection of the patient and human rights of mothers and newborns using real scientific research and the law. If you are interested in learning more and becoming part of the advocacy team to bring about national change in infant feeding, please contact us at contact@fedisbest.org
For more information on protecting your newborn from feeding complications, please read and download the Fed is Best Feeding Plan
To make a donation to the Fed is Best Foundation, go to https://fedisbest.org/donate/
References on Prelacteal feeding:
1: Hoa DP, Thanh HT, Höjer B, Persson LA. Young child feeding in a rural area in the Red River delta, Vietnam. Acta Paediatr. 1995 Sep;84(9):1045-9. PubMed PMID: 8652957.
2: Srivastava SP, Sharma VK, Kumar V. Breast feeding pattern in neonates. Indian Pediatr. 1994 Sep;31(9):1079-82. PubMed PMID: 7883365.
3: Semega-Janneh IJ, Bøhler E, Holm H, Matheson I, Holmboe-Ottesen G. Promoting breastfeeding in rural Gambia: combining traditional and modern knowledge. Health Policy Plan. 2001 Jun;16(2):199-205. PubMed PMID: 11358922.
4: Davies-Adetugbo AA. Sociocultural factors and the promotion of exclusive breastfeeding in rural Yoruba communities of Osun State, Nigeria. Soc Sci Med. 1997 Jul;45(1):113-25. PubMed PMID: 9203276.
5: Delport SD, Bergh AM, Hay IT. Breast-feeding practices in a private maternity hospital. S Afr Med J. 1988 Oct 15;74(8):396-9. PubMed PMID: 3187818.
6: Kumar S, Nath LM, Reddaiah VP. Breast feeding practices in a resettlement colony and its implications for promotional activities. Indian J Pediatr. 1989 Mar-Apr;56(2):239-42. PubMed PMID: 2807451.
7: Islam MA, Nielsen CC. Maternal and child health services: evaluating mothers’ perceptions and participation. Public Health. 1993 Jul;107(4):243-9. PubMed PMID: 8356206.
8: Ashraf RN, Jalil F, Khan SR, Zaman S, Karlberg J, Lindblad BS, Hanson LA. Early child health in Lahore, Pakistan: V. Feeding patterns. Acta Paediatr Suppl.1993 Aug;82 Suppl 390:47-61. PubMed PMID: 8219467.
9: Dashti M, Scott JA, Edwards CA, Al-Sughayer M. Determinants of breastfeeding initiation among mothers in Kuwait. Int Breastfeed J. 2010 Jul 28;5:7. doi:10.1186/1746-4358-5-7. PubMed PMID: 20667112; PubMed Central PMCID: PMC2917400.



I couldn’t agree more with this post. I am a big supporter of Fed is Best as a family doctor who does deliver babies over 25 years I am about to navigate our own hospital wanting this label. To what end? More unsafety and no boundaries on when to use “breast milk substitute” and the nurses/some docs and administrators push beyond these boundaries anyway. Not all of them do but who is following up with these babies and the issues is not always educated as to the harmful effects of insufficient breast milk. The health issues can go beyond repair and who is accountable is sometimes difficult. A new mother is trusting her caregivers who themselves are not educated in what can happen. No one wants to be the one to say “this baby needs some formula”. Denial is a big part of this as well. There are alot of posters that praise the benefits of breastmilk and none that say well this is what could happen if your baby doesn’t get any or enough.
Change must happen. I have written the administrators in the hospital and in the community and now provincially-on the Perinatal BC website under hypoglycemia they write “there is no evidence that low blood glucose concentrations among healthy bf term babies who are feeding well (no definition), are detrimental to outcome. Dated July 2003. This is on a public website with references sited from 1988 onward…..
Their defense is that underfed newborns is very uncommon, rare.(so it doesn’t need attention)
Apparently almost 300,000 subscribers think not.
My experience is that change comes about most effectively with the help of lawyers and the human rights commission.They have to listen. The best people to bring about change in feeding infants and the pressure on the mother/parents are the people whose lives have been changed by these policies. No one likes to involve lawyers I am just suggesting that those accountable will have to come out of hiding. For example, a father in British Columbia was so fed up with the province not helping with his autistic son’s education help that he sued them successfully. Now everyone with an autistic child in BC gets funding while they are in school. His work directly helped my son and many many other autistic children. Likewise the Doctors in BC would not have an inclusive maternity/paternity leave if I had not taken steps that I did. It is possible.
The Baby (Un) Friendly Initiative comes to the patient from the agencies that implement health care from the Provincial/State level down from the Federal level. Their guidelines have been unchanged or unchallenged for over a decade in our case-14 years. If these guidelines cause harm to baby or mother in their interpretation or lack of balance, and people have suffered then they have to held accountable. It will trickle up the ladder.
Thank you so much Dr. Conkin for defending mothers and babies and sharing your experience with our audience. It has got to stop. The BFHI is the most dangerous health policy that has ever been written and has hospitalized and violated the human rights of more previously healthy individuals than any health policy in the history of public health.
Breastfeeding is already very hard, at hospitals there’s actually little or no help at all even in the hospital breastfeeding friendly hospitals, where nurses who should be teaching you don’t even know themselves. I agree fed is best. But it would be very helpful to actually help moms to successfully breastfeed, and in case moms are actually unable to produce milk to get help with galactoguegues and pumping to produce more milk. I agree some moms need to supplement, it majority prefer bottle feed because is they didn’t got help to breastfeed, or because is way easier to bottle feed. Formula doesn’t have all the antibodies and benefits from breast milk. I wasn’t breastfed and was always sicker than my breastfeed brothers