Written by: Jody Segrave-Daly, MS, RN, IBCLC
Cluster feeding is a phrase that is used to describe infant feeding behavior. Generally, it’s breastfeeding or bottle feeding that is in a different pattern from your baby’s typical feeding pattern. It is described as breastfeeding sessions or bottle-feeding sessions that are much shorter and more frequent, for 3-4 hours of the day. It often happens during a baby’s fussy period of the day.
Cluster feeding is a phrase that sometimes is also called “comfort-feeding.” As parents, we react to infant cries and feeding cues, so naturally, we will assume a baby is hungry, and when we feed them, they will be satisfied. However, some babies will snack and will not take a full feeding during their cluster-feeding time; this is normal. Some babies want to suckle on a pacifier after nursing or bottle feeding. This is because their bellies are full, but they want to suckle for soothing and not for feeding milk. Some breastfeeding babies will suckle, using non-nutritive sucking patterns for soothing only. Some babies will also want to be held and snuggled, carried, or want movement while suckling too.
Cluster feeding can also happen during growth spurts, but babies generally take in more milk during this time. It can also happen during times when a baby is not feeling well, teething, or is tired or cranky. And it’s true—some babies don’t cluster feed at all. My exclusively breastfed babies never did and preferred sucking on a pacifier after nursing for comfort.
When is cluster feeding considered normal?
- It happens after a mother’s full milk supply is in, after birth.
- It is during a limited time period of 3-4 hours in 24 hours.
- The breastfeeding mother has an adequate milk supply.
- Baby is having plenty of dirty and wet diapers.
- The baby is gaining enough weight.
If you are concerned that you are not making enough breast milk or your baby isn’t transferring enough milk, you can do a simple weight check before and after nursing to see how much milk was transferred.
If your milk supply is low and/or your baby isn’t transferring enough breast milk, get immediate help to determine why your supply is low. This is very important information to know so that timely milk supplementation can occur to protect your baby from underfeeding. It’s also vital so that you won’t miss an opportunity to increase your milk supply.
Do babies “cluster feed” before the onset of copious milk production during the first few days of life? No. Breastfeeding babies nurse frequently, every 2-3 hours which is normal but different from “cluster feeding.” Bottle-feeding babies do not cluster feed during this time.
What is normal frequent breastfeeding?
This checklist will help you determine whether your baby’s feeding behavior is normal after birth and ensure your newborn receives adequate fluids and colostrum before your milk comes in.
| Normal Frequent Feeding | Abnormal Feeding Behavior Before Lactogenesis II |
| It is common:
Breastfeeding every 2-3 hours, or 10-12 times in 24 hours, with a good latch. Mother is able to hand express ample colostrum before each feeding. |
The baby is nursing more than every 2 hours or is unsettled, fussing, or crying after nursing.
Mother is not able to hand express ample colostrum before each feeding. May show signs of low blood sugar levels with hand tremors or high-pitched crying. Some babies become exhausted from excessive feeding and crying, eventually appearing fatigued and uninterested in feeding. *Review maternal medical and psychosocial history to evaluate DOL2 risk factors to provide timely supplementation. |
| Baby is nursing effectively on both breasts and is satisfied after nursing and in between feedings. | Baby continues exhibiting strong HUNGRY cues after nursing and between nursing sessions.
The mother is concerned and distraught. |
| Appropriate wet and dirty diapers | Concentrated dark urine, reduced urination (no wet diapers for 6 hours), reduced bowel movements/meconium, and urate crystals in the diaper (orangish to red staining after urination) |
| Lips, mouth, and tongue are moist.
Ample oral saliva. |
Lips may be cracked, dry, or peeling. The mucosal membranes (mouth and tongue) are pasty or dry, with scant saliva. |
| Jaundice levels (yellow skin) are stable and within normal limits. | Jaundice levels are increasing and the eyes are yellow. |
| Weight loss is less than 4.5% in the first 24 hours of life, 7% on day 2, or more than 7% at any time.
*We recommend using an online weight loss nomogram that tracks hourly weight loss for the optimal tracking Newt – Newborn Weight Loss Tool |
Weight loss is more than 4.5% in the first 24 hours of life and more than 7% on day 2.
*We recommend using an online weight loss nomogram that tracks hourly weight loss for optimal tracking Newt – Newborn Weight Loss Tool |
| Does not warrant serum blood testing. | Abnormal serum laboratory results for dehydration, hypoglycemia, or hyperbilirubinemia. |
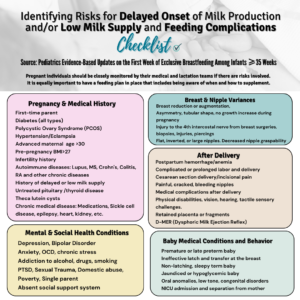
Note* A mother who is at risk for delayed onset of copious milk production requires special considerations for timely supplementation to keep her baby from experiencing hunger and thirst and preventing complications of insufficient breastfeeding.
Babies who are nursing constantly or babies who nurse and are not satisfied and cry when removed from the breast, require an immediate exam by the pediatrician and a full assessment by the mother-baby RN to be sure they are receiving enough colostrum.
The Academy of Breastfeeding Medicine defines cluster feeding as “several short feedings close together.” However, mothers are being told constant and prolonged feeding around the clock is “cluster feeding” before their milk is in (lactogenesis 2) and this is where confusion that can result and harm begins.
There is a point when frequent feeding becomes a clear sign of insufficient breast milk and/or insufficient transfer of milk and those signs must be taken seriously for the health and safety of the infant. Mothers tell us they receive conflicting information and as a result, they become very frustrated, lose confidence and want to stop breastfeeding. It is important to define what cluster feeding really is as health professionals and evaluate and intervene when an infant is in danger of insufficient feeding complications.
There is no stronger maternal drive than to feed your baby and protect him from harm. Mothers experience incredible emotional suffering when they are told their baby “was just cluster feeding,” but it turns out in hindsight they were not eating a sufficient amount, even after nursing for hours. They blame themselves rather than the health professionals who should have taken their concerns seriously.
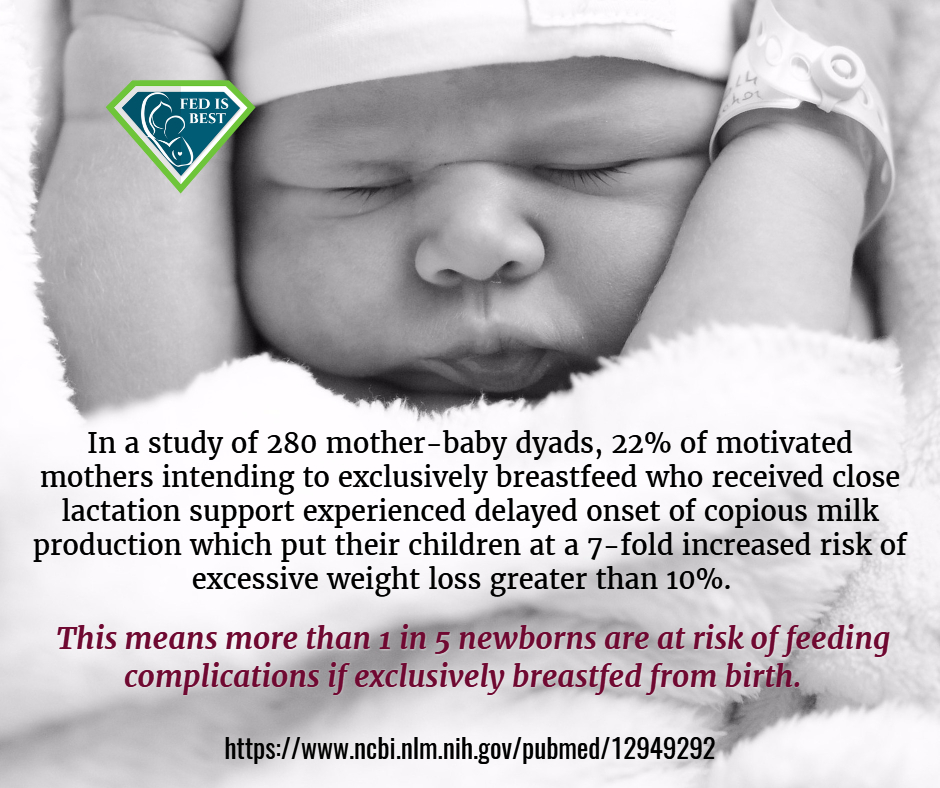
The actual rates of adequate milk production are unknown, the current estimates for lactation disruption range from 12-15% or one in eight mothers. We are learning that mothers are experiencing delayed lactogenesis II (onset of full milk supply greater than 72 hours post birth) commonly for complex biological and other unknown reasons. Delayed lactogenesis II occurs to 1 in 5 mothers, which is more common than previously reported. Some newborns need more than colostrum to be safely fed. Others simply cannot breastfeed effectively to receive the colostrum that is present.
When your baby requires supplementation, donor milk from a milk bank or formula can be used. Supplementing will protect your baby from complications while waiting for your milk to come in.
Research has shown that hearing of swallows in the first days of life is not a reliable indicator of how much colostrum milk a baby is ingesting. A full clinical exam is necessary to evaluate a newborn for safe and adequate intake while breastfeeding. It’s imperative to assess each mother and baby to identify potential individual risk factors for delayed onset of lactogenesis II or low milk supply. This will help the health care team offer timely, temporary supplemental nutrition with banked donor milk or formula milk to prevent complications for identified high-risk dyads.
The physician, nurse and lactation consultant care team should be evaluating the newborn for signs of hypoglycemia, ineffective latch or transfer, weight loss percent, bilirubin levels persistent hunger cues, oral anomalies, lethargy, dehydration/hypernatremia, vital signs, presence of red urate crystals in diapers and diaper counts after copious milk production has occurred. Additionally, the health care team can identify scant or absent colostrum in a high-risk mother through instruction on manual expression; this can help inform the mother and the team that earlier supplementation may be needed for her newborn to prevent feeding complications. All of the clinical markers must be within normal limits for a baby to be considered adequately fed.
According to a review published in the Journal Of Family Practice in June 2018, “exclusive breastfeeding at discharge from the hospital is likely the single greatest risk factor for hospital readmission in newborns. Term infants who are exclusively breastfed are more likely to be hospitalized compared to formula-fed or mixed-fed infants, due to hyperbilirubinemia, dehydration, hypernatremia, and weight loss.” They estimated that for every 71 infants that are exclusively breastfed, one is hospitalized for serious feeding complications.
Five RCT studies have shown that judicious supplementation (two teaspoons) after nursing with formula or donor breast milk had no effect on long-term breastfeeding, one showing it prevented hospital readmissions.
- Limited Amount of Formula May Facilitate Breastfeeding: Randomized, Controlled Trial to Compare Standard Clinical Practice versus Limited Supplemental Feeding
- The Effect of Early Limited Formula on Breastfeeding, Readmission, and Intestinal Microbiota: A Randomized Clinical Trial
- Limited Amount of Formula May Facilitate Breastfeeding: Randomized, Controlled Trial to Compare Standard Clinical Practice versus Limited Supplemental Feeding
- Effect of Donor Milk Supplementation on Breastfeeding Outcomes in Term Newborns: A Randomized Controlled Trial
- Effect of Early Limited Formula on Breastfeeding Duration in the First Year of Life
- In-hospital formula supplementation and breastfeeding initiation in infants born to women with pregestational diabetes mellitus
How many randomized, controlled studies support Step 6 of the WHO’s Ten Steps to Successful Breastfeeding to exclusively breastfeeding from birth to 6 months and avoid supplementation to improve breastfeeding outcomes? None. Absolutely none.
For stories of mothers who supplemented their breastfeeding babies and went on to breast-feed click here.
For stories of mothers who regret not supplementing their breastfeeding babies and who suffered complications click here.
To learn how to supplement while protecting your milk supply click here.
To learn more about our safe infant feeding guidelines we have a FREE downloadable feeding plan for every family to use.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join us in any of the Fed is Best volunteer and advocacy, groups. We currently have– Health Care Professionals group, Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Maternal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org– if you are interested in joining any of our volunteer groups.
- If you need infant feeding support, we have a private support group– Join us here.
- To join our Health Care Professional private Facebook support group- Join us here. us here.
- If you or your baby were harmed from complications of insufficient breastfeeding please send a message to contact@fedisbest.org
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Sign our petition! Help us reach our policymakers, and drive change at a global level. Help us stand up for the lives of millions of infants who deserve a fighting chance. Sign the Fed is Best Petition at Change.org today, and share it with others.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educational resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write to them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop at Amazon Smile and Amazon donates to Fed Is Best Foundation.
Or simply send us a message to find out how you can help make a difference with new ideas!
For any urgent messages or questions about infant feeding, please do not leave a message on this page as it will not get to us immediately. Instead, please email christie@fedisbest.org.
Thank you and we look forward to hearing from you!

