They tell you that if you prepare enough, breastfeeding will work. They tell you that all you need is support, commitment, and trust in your body, and you will be successful. If only it were that simple.
What they don’t tell you is that your mammary biology can have limitations. I am that mom.
I knew I might have issues. I had breast reduction surgeryback in 2001, but had been told that using the right technique would preserve my ability to breastfeed. Nonetheless, I set out preparing to ensure I would be successful. Besides doing yoga, pilates, weight training, and exercise, I entered the midwife program and prepped diligently. I did prenatal workshops and tracked down a book on how to successfully be a breast feeding after reductionmom.
I hired a private lactation consultant for a session ahead of time. We talked about teas and tinctures, techniques, and diet to help my supply be optimal. (Note: there is no evidence that teas, tinctures, or foods increase milk supply). We talked about how I could use a supplemental nursing system if necessary. I read extensively and was convinced breastfeeding was the only way to feed my son to ensure his well-being, and I would have no problem breastfeeding because I had SUPPORT.
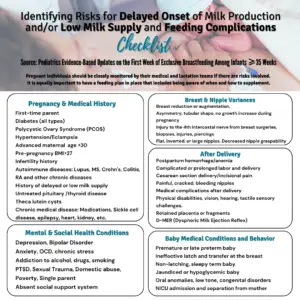
Note: Unfortunately, she was not informed of all her significant risk factors and how to supplement her baby until her milk supply was enough to feed her baby safely. Breast reduction surgery requires specific management and interventions that she did not receive.
After lengthy pre-labor, labor finally started, but my son was posterior, and we stalled at 5cm dilated for over 10 hours. Finally, 33 hours after labor started, I delivered our son vaginally. I was exhausted after being awake for 3 days straight but determined to breastfeed. We seemed to struggle with latching, and when he finally did, the pain took my breath away. I had already gone through 25 hours of labor before finally getting an epidural, but the pain during each feed was excruciating and only ended when he stopped feeding.
Within a few hours, I was concerned by the pain and by my misshapen nipples, which were already severely cracked and bleeding. I asked each nurse that I saw. All told me the latch was good and waved off my concerns about pain. My reading had told me to keep going but also mentioned it shouldn’t hurt this way. Worse yet, I often worried about how rarely he seemed satisfied with eating or would suckle to sleep. Yet we were released from the hospital with instructions to be patient and told that breastfeeding would work out.
When I pressed about my bleeding nipples, one nurse snapped at me: “What did you expect?”
My son barely urinated in the first few days, and by day 4 seemed more and more unsettled, finally crying 5 hours straightin the middle of the night. I was trying to let him feed as much as possible, but the pain persisted. The nipple shields a nurse gave me in the hospital helped my son to latch, but the pain persisted with every feed during the whole feed. My son always seemed hungry and would stay latched on for over an hour if I left him. I’d try to persist in feeding him, exhausted in bed, weeping at the pain and frustration.

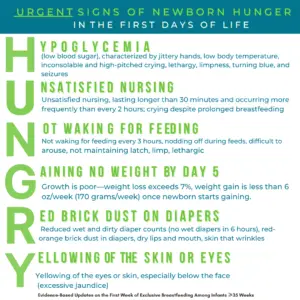
I was not informed of the newborn HUNGRY signs, knowing I had significant risk factors for low milk supply.
Our midwife team came for home visits every day. I dutifully showed our tracking charts of how long/often at each breast, his output, and they would weigh him. He was quickly dropping weight, so we tried to come up with a strategy. I kept eating oatmeal and good food like quinoa and drinking lots of water. We bought a lactating tincture, which I took religiously, and by day 4, we both went for chiropractic and osteopathic care in case that would help. I got acupuncture. (Note: no evidence exists that these suggestions increase milk supply). During this time, my wife contacted public health for another lactation consultant. I was doing all the right things, but my son was barely urinating and kept dropping weight.
The lactation consultant ‘diagnosed’ a posterior tongue tie and lip tie, which she believed was the cause of my pain and the state of my still bleeding nipples that would often be blanched white and misshapen after a feed. (Note: Lactation consultants cannot diagnose a tongue tie. They should refer to the pediatrician for any concerns they might assess. )
She thought temporary supplementation would be needed but was insistent on no artificial nipples, so we had to tube feed him with SNS or by finger. I was told not to use a soother, so he often fussed unless I let him latch onto the shield on my breast. I pleaded to get my son into a specialist quickly, and the frenectomy was performed at 7 days. Sadly, it did not help my pain. The Dr. who did the procedure would tell me after the procedure that she didn’t think the tie was serious enough to warrant the frenectomy and that the real issue was an anatomically small jaw that would have to grow.
By this point, my midwives were seriously concerned. My son had dropped over 11% of his body weight and still struggled to urinate. The minimal supplementation the LC recommended at the breast was not adequate. At the recommendation of the LC, I agreed to take domperidone. Surely, this medication would get me to exclusive breastfeeding. Formula was not the answer. My midwife explained I would need an EKG since it puts me at risk for heart arrhythmia. I have a family history of heart disease, but I was still interested. (*Please note domperidone is banned in the US.)
At that point, my wife put her foot down. “We both need you alive. He needs you more than your breast milk.”

Enjoying skin-to-skin time, I am desperate to increase my milk supply.
From that point on, we stopped feeding with a tube and went to supplementation with a bottle. Our lactation consultant cut off contact with me right after the frenectomy. Based on her comments, I was devastated to realize that she didn’t want to work with someone who used a bottle or a soother (something else the midwives insisted upon to give my poor nipples a chance to heal – my son wanted to be latched 24/7).
All this occurred in the first 10 days of my son’s life. I persisted in trying to combo feed for 19 weeks. Any breastfeeding session still resulted in horrible pain, with my nipples blanched white and misshapen. He hated latching without a shield, and as he grew, my supply never increased, even with continued oatmeal, tincture, water, etc. I was struggling to bond with him all those weeks later.
Even if I was the proverbial Queen of Sheba with an army of attendants and best medical care we would have still had all the problems. I still had low supply that was compounded by the chronic pain. I look back and realize that I put us through a lot of heartache for no real benefit.
I finally weaned. My depression and anxiety lifted almost immediately and I bonded with the baby. I had worked so hard to give him the best start in life. I only wished I had listened to my midwife and not my lactation consultant when she pleaded with me to understand that my son would thrive on formula, and I did everything in my biological power to make it work. Sadly, I will never get back the time lost while following all of the unproven suggestions from my lactation consultant. Today, he thrives in daycare, and I honestly can’t tell which of his friends were breastfed, combo-fed, or formula-fed. He is well-adjusted, healthy, thriving, and bonded to both of us. That is what matters.

My precious son thrives on formula and love.
HOW YOU CAN SUPPORT FED IS BEST ? JOIN US!

There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
WE ARE EXCITED TO ANNOUNCE OUR UPCOMING BOOK!
It is now available for pre-order at all major retailers! Coming June 25, 2024!
Go toFed is Best Book to pre-order today!
Video Player
HOW YOU CAN SUPPORT FED IS BEST? JOIN US!

There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Send us your stories. Share with us your successes, your struggles, and everything in between. Every story saves another child from experiencing the same and teaches another mom how to feed her baby safely. Every voice contributes to change. Contact: jody@fedisbest.org
- If you need infant feeding support, we have a private support group– Join us here.
- If you or your baby were harmed from complications of insufficient breastfeeding, please send a message to contact@fedisbest.org
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, and our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies, and 100% of your donations go toward these operational costs. All of the Foundation’s work is achieved via its supporters’ pro bono and volunteer work.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page, and by sending our FREE infant feeding educational resources to expectant families you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write to them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail it to your local obstetricians, midwives, and family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for the legal protection of newborn babies from underfeeding and for the mother’s rights to honest, informed consent on the risks of insufficient feeding of breastfed babies.
- Join us in any Fed is Best volunteer and advocacy groups. Click here to join our health Social Media Group, Legal Group, Marketing Group, Perinatal Mental Health Advocacy Group, and Fundraising Group. Please email Jody@fedisbest.org if you want to join any of our volunteer groups.
- Send us messages of support. We work daily to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
Thank you so much from the Founders of the Fed is Best Foundation!

2 thoughts on “I Had All of The Support In The World And Breastfeeding Still Didn’t Work.”