By Tina Cartwright, Founder of Rebranding Motherhood
My journey through childbirth and early motherhood was far from easy, but it was undeniably transformative. It taught me the importance of resilience, self-compassion, and the power of community in navigating motherhood’s most profound challenges. Before reaching this undeniable truth, my birth trauma thrust me into an arduous journey as I entered motherhood.
Birth trauma is tricky because society would love to put a clean, simple definition on it. However, trauma is defined by the individual and what that experience led you to feel afterward. For me, my birth trauma started when I first held my baby. The elusive bond between mother and child didn’t materialize instantaneously for me, unlike the glossy portrayals Hollywood and social media would suggest.
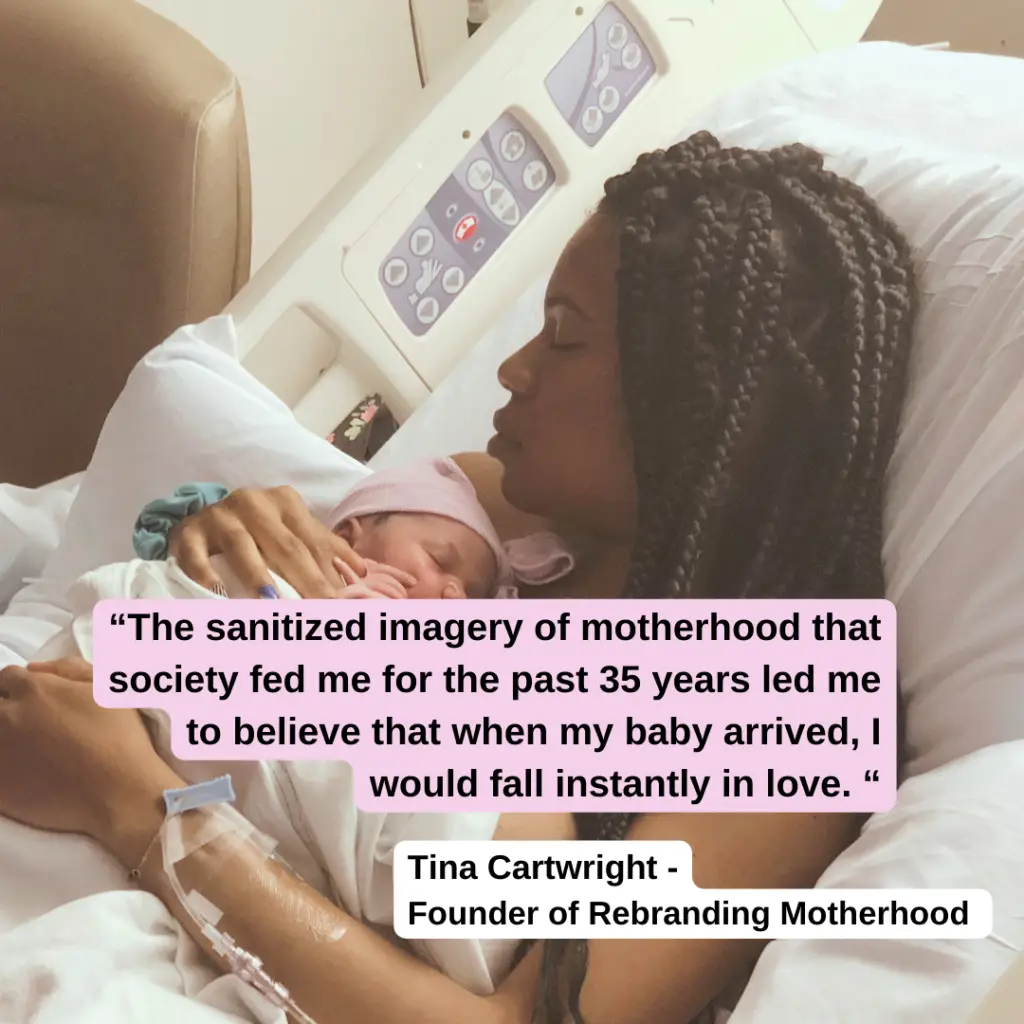
This sanitized imagery further claimed I would be overwhelmed, almost washed over with the deepest levels of instant joy and admiration for my new baby. Within seconds of this stark realization hitting me, I instantly began a silent inner panic that never quieted until I was ultimately diagnosed with PMAD (postpartum depression) and started a formal treatment plan.