Hopefully, my experiences will help another family avoid the psychological trauma that I endured while breastfeeding my daughter. This is what I learned:
- Sacrificing your mental health or your baby’s health (or both!) to exclusively breastfeed is not worth it.
- Some breastfeeding advocates don’t see (or don’t want to see) the risks of exclusive breastfeeding which include a baby who isn’t gaining weight sufficiently, an emotionally suffering mum, or a strained mother–baby relationship.
- Seek help from lactation professionals who are open-minded enough to suggest combo-feeding as an option and are willing to support your choice because sometimes exclusive breastfeeding is not an option.
While pregnant, when imagining myself with my new baby, I was always breastfeeding her. That image defined my new role as a mum. I was glowing with love, she was happily eating, and I felt so proud of being able to provide her with “the best.” There was no alternative in my mind. I was planning on staying at home for a whole year anyway, so it would be easy to breastfeed her for as long as I wanted. I had heard that some women didn’t exclusively breastfeed for long, but I simply wasn’t going to be one of them. I didn’t even care about what their reasons were. I always thought that if you tried enough, it would work. It was natural, so nature was going to work for me and my baby. Right? Wrong.
Breastfeeding has been one of the least natural things I have ever experienced.
I was lucky enough to be blessed with a wonderful pregnancy and a beautiful, natural birth. I was waiting for my daughter to crawl to my breast and start suckling right after, but she soon fell asleep instead. She spent the first 24 hours mostly sleeping and didn’t eat at all. We then started giving her formula and my expressed colostrum and went on to give her a bottle of formula the next day, as she was dehydrated and had lost 10 percent of her birth weight. I was still hopeful that once my milk came in, things would fall into place and she would be exclusively breastfed.
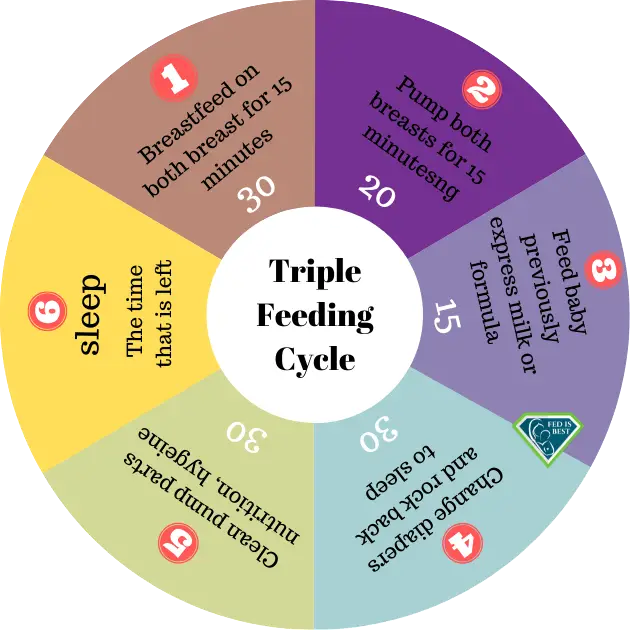
Babies cry when they are hungry, I was told. Mine didn’t. I had to wake her up and literally force her to latch. For the next few weeks, I triple fed her: I woke her up every three hours, which took several minutes; tried to breastfeed her using a nipple shield (I say try because those 15 minutes on each side were spent trying to keep her awake after an initial latch and a couple of weak sucks—she almost never activated my letdown reflex); then my husband would give her a bottle of formula or pumped milk, which she would gulp right down; then I would pump for 30 minutes. Every three hours. Needless to say, I hardly slept. Because she wouldn’t really stimulate my breasts, I got mastitis and, I realized later, a low supply. I was a wreck and could hardly utter a sentence without crying. Why was it so hard for us? Why did she prefer the bottle instead of my breast? My only duty during those first months was to feed her. I felt like I was failing as a mum already.
@keyframes spinning {
from { transform: rotate(0deg) }
to { transform: rotate(360deg) }
}
.spin {
animation-name: spinning;
animation-duration: 25s;
animation-iteration-count: infinite;
/* linear | ease | ease-in | ease-out | ease-in-out */
animation-timing-function: linear;
}
Unfortunately, triple feeding has become the default method that is recommended by medical and lactation professionals for a large number of breastfeeding challenges, with no regard to the psychological maternal complications that will eventually occur, or the likelihood of it solving the problem of low milk supply.
Despite people telling me that it was ok to “give up and feed her formula,” I was determined to make it work. Because again, in my mind, there was no alternative. So I made an appointment with a lactation consultant who gave us an SNS system, forbade us from using the bottle to avoid nipple confusion, and put me on a medication that promotes milk production. I would again try to nurse, then use the SNS system with my pumped milk or formula, then pump—so basically still triple feeding. My girl was still very sleepy, had a weak suck, and was not putting on a lot of weight. I could only nurse her at home because it was too complicated to use the SNS system outside. She was already two months old at this time. I was yearning to go out and meet other people. My soul was lonely. I was lonely. I wanted to be one of those smiling, calm mums who breastfeed their babies anywhere. I wanted to experience feeding her without it being a struggle every single time.
At some point and when my baby was around three months old, I was given the green light to exclusively breastfeed her by this lactation consultant.
I was pumping enough milk to supplement her feedings—a set amount which didn’t really take into account whether or not she was satisfied—so “no more pumping, no more SNS,” she said. I hardly felt ready for it, but I followed her advice nonetheless because she was the expert.
My daughter was and still is a very “easy” baby. In those early days, she hardly ever cried from hunger. I realised much later that I wasn’t interpreting her hunger cues correctly, but nobody had told me how to. After we stopped bottle-feeding her with formula, she only put on 100 g maximum per week, for weeks on end.
I kept asking the lactation consultant if this was ok, and she said that I simply had a thin baby, that the average is 150 g per week, so “a little bit less than that is fine.” But a voice inside me was telling me that it wasn’t fine. Something just didn’t feel right.
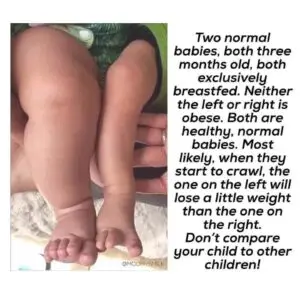
This picture clearly shows how extreme lactivism will sacrifice a baby to sustain exclusive breastfeeding even though babies are malnourished. How can anyone believe the baby on the right is not malnourished?
I started getting so worried about her eating enough that every single nursing session would almost be preceded by a panic attack and the same torturing thoughts: “Will she have enough? Is she having enough? Has she had enough?” These panic attacks got so bad that at times my letdown would literally disappear, leaving her hungry. But I still wasn’t “allowed” to give her a bottle of formula. It was obvious that despite all our efforts, things weren’t quite working out for us. Breastfeeding had become a never-ending battle.
Only my husband saw what this whole effort was doing to me. The tears before and after a nursing session, the agony of countless clogged ducts, the frustration of having to take antibiotics because of another breast infection. I was slowly reaching a point of postpartum depression when I decided to hear the voice that was telling me that my baby wasn’t getting enough. I gave her a bottle with formula and started my own version of unguided combo-feeding. I didn’t let the lactation consultant know; I felt like I would be disappointing her somehow.
I realise now how wrong that was. Nobody should have a say as to how I feed my baby except for me.
According to Fed is Best’s feeding plan, my baby and I had many of the risk factors for feeding complications. Giving her formula at the very beginning was not only not a mistake, it was necessary. She is now exclusively formula fed, and even though I am entirely sure of my choice to end our breastfeeding journey, it still hurts.
I live in a country where breastfeeding is the norm. Wherever I go, whatever I do, I see women breastfeeding their babies. Breastfeeding grief and trauma are real, and they are not about the baby. How do you get over a trauma when you’re confronted with it over and over again anyway? I am still working that one out, with the help of a therapist.
These results suggest that public responses causing a mother to feel guilty for using infant formula result in negative feelings of self-worth and dysfunctional maternal behaviors.
I wish I had discovered the Fed is Best Foundation before, or had a professional to turn to when I decided that combo-feeding was the way to go. Who knows? If the weight of “all or nothing” had been lifted earlier, if I didn’t feel like giving formula meant that I had failed, if I had been given—and given myself—permission, perhaps I would still be breastfeeding on my own terms right now.
-Jannie R.
Feeding Your Baby—When Supplementing Saves Breastfeeding and Saves Lives
Clinicians’ Guide to Supporting Parents with Guilt About Breastfeeding Challenges

One thought on “Sacrificing Your Mental Health Is Not Worth It To Exclusively Breastfeed”