Jody Segrave-Daly, RN, MS, IBCLC
Mothers are taught that it’s rare to not produce enough milk to exclusively breastfeed in nearly every breastfeeding book, mommy group and hospital breastfeeding class. The truth is, we have limited studies that provide an accurate percentage of the number of mothers who can produce enough milk for their baby for the recommended 6 months. Although actual rates of failed milk production are unknown, there are estimates that range from 5-15 percent or more.
- Dr. Marianne Neifert, Clinical Professor of Pediatrics at the University of Colorado Denver School of Medicine, who co-authored a 1990 study of 319 breastfeeding women found 15 percent of the women were unable to produce sufficient milk by three weeks after delivery.
- Data from the Infant Feeding Practices Study (IFPS) II, a study of U.S. women, showed that one in eight women experienced early, undesired weaning from disrupted lactation due to physiologic reasons. According to the study, pain, difficulty with latch and insufficient breast milk supply were the most common reasons for early weaning.
- Dr. Shannon Kelleher talks about these staggering numbers in her publication, “Biological underpinnings of breastfeeding challenges: the role of genetics, diet, and environment on lactation physiology,” where she says the prevalence of lactation insufficiency may be much higher, as 40–50% of women in the US and 60–90% of women internationally cite “not producing enough milk” or that their baby was “not satisfied with breast milk” as the primary reasons for weaning prior to 6 months.
In my extensive 30-year experience of working clinically with moms and babies in the NICU as a Registered Nurse and as an IBCLC in private practice, I have seen vast differences in colostrum and milk production within the 6 months recommended for exclusive breastfeeding. In my daily practice, I commonly see underfed babies who have been under the guidance of other lactation consultants. I believe some health care professionals and LCs are overly focused on protecting the breastfeeding relationship rather than protecting the baby. I have seen an acceptance of persistent infant hunger and poor growth in order to protect and achieve exclusive breastfeeding status among avid breastfeeding advocates. Unfortunately, I have had to refer many of these malnourished babies for admission to the hospital.
Successful breastfeeding management protects both the baby and the breastfeeding relationship while supporting maternal mental health.
Anna contacted me to help her breastfeed her second baby. Her first baby struggled to gain weight, despite seeing multiple IBCLCs and spending over $1,000 for services. He didn’t gain enough weight, was malnourished and Anna became profoundly exhausted from pumping after every nursing. Anna’s baby experienced the common occurrence of not being the priority. Anna’s mental and physical health were also not a priority.
In order for the baby to receive the full benefits of breast-milk, adequate and safe feeding must be the number one priority, every time.
With her second baby, we reviewed all of her risk factors prenatally and created a feeding plan that was flexible but would adequately feed her baby. I provided Anna with a realistic feeding and pumping schedule that would accommodate caring for a toddler while maximizing her time for rest. Her overall goal was to breastfeed while making sure her baby was well fed this time, so she could be present and enjoy the first weeks of having a newborn that she missed with her first baby.
Our contact began right after delivery and she followed the breastfeeding plan that we created. After delivery we talked multiple times a day as she needed guidance. She had delayed onset of milk at day 5 again, but wanted her baby to be supplemented the first day to avoid the unintended starvation that her first baby experienced. She continued to nurse, self-express and power-pump to maximize her milk production. The first weeks at home required multiple contacts daily and she supplemented until her full milk supply was in. She had many bumps along the way, but we quickly tweaked her feeding plan to help her cope, so she could continue breast feeding. When her full milk supply was in at almost 3 weeks, she was able to breastfeed, with occasional supplementation.

Left, first baby, exclusively breastfed, malnourished and underweight at 1 month. Right, second baby supplemented after nursing from birth until 3 weeks, safely fed and thriving at 1 month.
What we know
Failed lactogenesis ll, known as the onset of breast milk ‘coming in’, can be from 3 reasons.
- First, there is a maternal biological reason that interferes with adequate milk production.
- Second, there are multiple reasons that can hinder effective sucking and removal of breast milk by the baby.
- Third, there can be a combination of maternal and newborn reasons, combined with improper breastfeeding management.
Fortunately, most moms do make enough milk to adequately feed their babies but for the estimated 5-15% of mothers who don’t, they are often in shock and disbelief when they realize they are not making enough milk to fully feed their babies. It breaks my heart, every time, when I have to tell a mother her baby is hungry and needs immediate supplementation after they were instructed to just keep breastfeeding. They are commonly told to avoid supplementation despite their baby displaying obvious signs of persistent hunger.
Tonya
Tonya contacted me because her 6 week old baby was very sleepy and was not waking up to feed. She was an experienced breastfeeding mom of two and thought he was just a really good baby. She thought he looked small but everyone kept telling her not to worry as he was just long. She panicked when she weighed him at home when he was a full pound under his birth weight at 6 weeks. She wanted to continue to breastfeed but needed help. She contacted me after talking with her pediatrician and we safely began to supplement, after every nursing. Her milk supply was very low and was just enough to keep her baby hydrated for the first 6 weeks.

Left, Her baby one pound below birth weight at 6 weeks. Right, gained 7 ounces in 2 days from supplementing
Supplementing an underfed baby will provide enough calories and fluids to increase alertness and the strength to nurse effectively. Why? Because babies who are being under fed will become very sleepy and sometimes lethargic as they are shutting down to conserve energy and calories. Even the smallest amounts of supplementation, will help perk up the baby to nurse more vigorously and remove milk effectively, which in turn stimulates the milk making hormone cascade optimally.
In 2 days’ time, Tonya’s baby became much more alert, demanded to be fed every 2-3 hours and gained 7 ounces! Tonya was able to include power-pumping to increase her milk supply and gradually he was able to breastfeed exclusively. He continued to gain weight and thrive.

Left at 8 Weeks and Right at 4 months of age
Supplementation when necessary will not decrease a mother’s milk supply if her breasts are stimulated with direct nursing, pumping or hand expression for each supplemental feeding. But, it is very important not to miss any breastfeeding or pumping sessions when supplementing. Once the milk volume increases, supplementing will decrease.
Krystal
Krystal was a first-time mom and her baby was born at 37 weeks by emergency c-section. Her baby was admitted to the NICU for 24 hours with respiratory support. She was able to breastfeed him several times in the NICU, but he was not satisfied and would cry and not settle after nursing. She was asked if he could be supplemented during the night as she was on another floor in the hospital and was not well enough to visit him during the night. She agreed and assumed he was being supplemented. She learned her baby was refused supplementation by the pediatrician because he insisted she be brought back up to the NICU to nurse him.
He was released from the NICU after 24 hours and for the next 24 hours he was profoundly sleepy, jaundiced and nursed poorly. He only had drops of colostrum which Krystal self-expressed. She was concerned about how ‘orange’ his skin was, but she was told he was fine because he had wet diapers.

Sleepy, lethargic and jaundiced.
When his pediatrician saw him the next morning, he was profoundly jaundiced, and lost 17 percent of his birth weight. He required immediate supplementation and ended back in the NICU for phototherapy and for full feedings. His bilirubin level was 19 which is dangerously elevated. Supplementing this baby saved his life but if he had been supplemented sooner, he would have avoided needless suffering. His parents were also saddled with debt from his second NICU admission.

17 percent weight loss and profoundly jaundiced.
What we are learning
We are learning that mothers in western societies are experiencing delayed lactogenesis II for complex and unknown reasons.
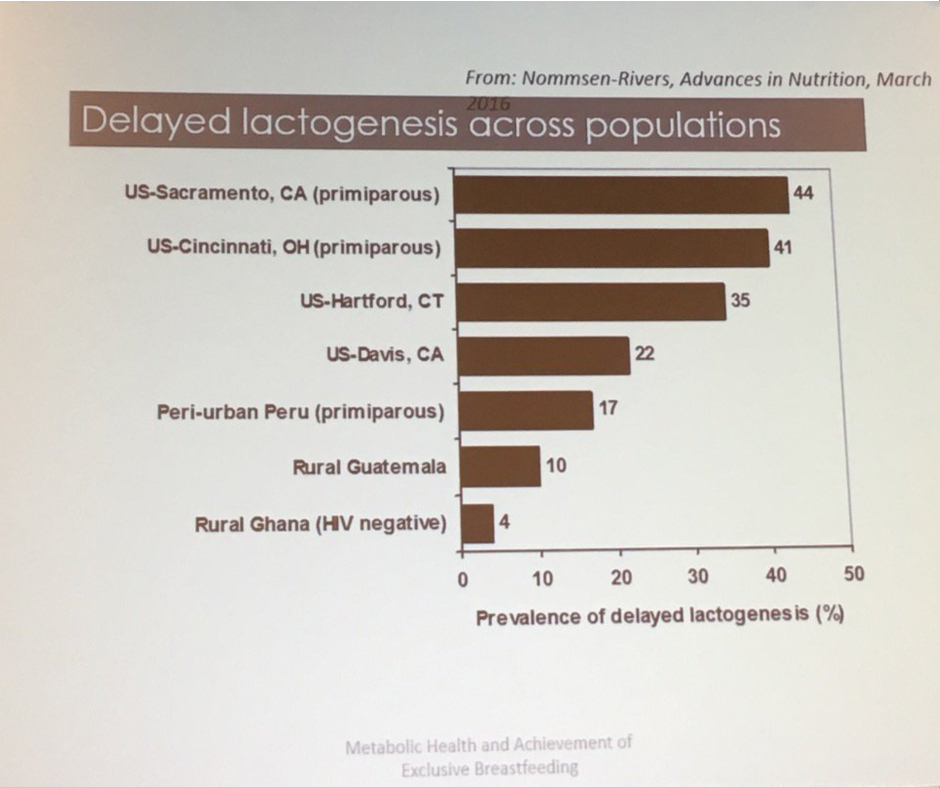
Nommsen-Rivers, Presented at 2017 ABM conference
- 22% of motivated, lactation-supported exclusively breastfeeding mothers experience delays in copious milk production that increase the risk of excessive weight loss in their newborns by 7-fold.
- 42–44% of first-time mothers have similar delays in copious milk production.
Delayed onset of full milk production does not mean a mother won’t make enough milk. It means her baby will likely need supplementation along with breastfeeding or pumping until her milk comes in.
The mothers I see are terribly distraught when they find out they were not informed of the consequences of delayed onset of milk production, how to recognize the signs of hunger or how to supplement safely.
No mother can accept that she unintentionally starved her baby.
There is a lengthy list of maternal biological risk factors for mothers who may develop delayed onset of milk production and/or chronic low milk supply. Health care professionals have the responsibility to educate mothers about the signs of inadequate milk production and the risk factors for delayed milk production at the same time they are educating mothers on breastfeeding benefits and technique. Identifying mothers who have risk factors pre- and postnatally can help health professionals prevent newborn feeding complications while providing optimal breastfeeding management, which are critical the first weeks after delivery.
Here you’ll find a variety of educational materials intended to support you in best feeding your newborn, and some materials to help your clinicians best support you in doing so. Please check back from time to time as we’re working to expand this section to include comprehensive feeding information for all types of feeding plans – breastfeeding, milk bank and formula feeding, pumping, bottle, tube, syringe, and cup feeding too.
If you need help, please contact me directly at jody@fedisbest.org
Jody Segrave-Daly’s entire 30-year nursing career has been dedicated to caring for healthy and medically fragile babies in the nursery and NICU. When she began her community-based infant feeding practice 6 years ago, she was not prepared to see the significant numbers of babies who were suffering from accidental starvation complications. The stories she heard were the same —distressed mothers were being told to never supplement their crying, sleepy, jaundiced, and dehydrated babies — or risk ruining their breastfeeding relationship and milk supply. She has comforted countless mothers all over the world who believed it was rare to under-produce breast milk and often felt betrayed by their healthcare teams, their own bodies, and the social pressure that insisted “Breast Is Best.” Now a staunch advocate for the Fed Is Best movement, Jody now works to debunk those myths while supporting mothers to breastfeed, mix-feed, pumped-milk-feed, formula-feed and tube-feed their babies. She has her own Facebook page and blog at the Momivist where she uses science and her years of clinical experience to support infant feeding. Read about her journey as a lactation consultant at Why I’m a Momivist.

Contact directly at jody@fedisbest.org
