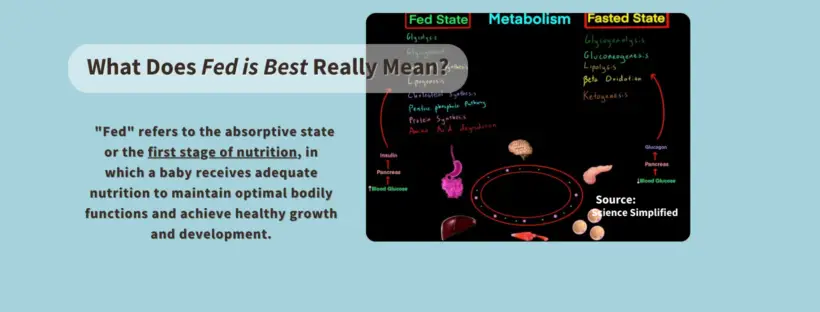
The phraseology of Fed is Best is frequently misinterpreted, and we want to clarify what it means to our readers. Nutritionally speaking, “fed” refers to the absorptive state or the first stage of nutrition, in which a baby receives adequate nutrition to maintain optimal bodily functions and achieve healthy growth and development.
Fed is best means a baby can achieve this fully fed state required to thrive from two clinically-approved sources of nutrition. One is human milk, and the other is infant formula.
Source: Science Simplified, May 13, 2020, Biology/Physiology, Video focused on details of Fed State of Metabolism.