Josephine contacted us after reading Dr. Christie del Castilo-Hegyi’s letter to health care professionals about the dangers of insufficient breastfeeding and the Baby-Friendly Hospital Initiative. Josephine is from Lagos, Nigeria, and wants to tell her story, because she believes every mother should know how to supplement her baby safely until her milk is flowing, no matter what country she lives in, to prevent brain damage and death from insufficient breastfeeding.
Category: *Top Blogs
How To Prepare For Supplementing When Breastfeeding Your Baby In The Hospital
Mothers who experienced delayed onset of milk production or experienced low milk supply with their first baby often contact us for support to try breastfeeding again. They typically have anticipatory anxiety because they have lost trust in their lactation professionals and hospital staff and are unwilling to attempt breastfeeding again without supplementation. They want to know how to supplement their baby until their milk supply becomes sufficient to feed them safely while providing proper breastfeeding stimulation for optimal milk production.
The New Seven Letter “F” Word
As soon as the word “formula” rolls off your tongue and leaves your mouth for everyone to hear, uncomfortable silence occurs. Parents are reluctant to talk about or admit freely they feed their babies infant formula. Most are suffering from the deeply entrenched shame and judgment that is associated with formula feeding; they have experienced it first hand in countless social media parenting groups, from friends, their health care professionals, WIC offices, and even in their hospitals.
How did we get to the place where talking about infant formula is profoundly divisive, shameful, and anxiety provoking for parents?
Let’s face it, infant FORMULA is the new seven letter F word. The scarlet letter F. FAILURE.
Why Fed Is Best: From One Therapist’s Point Of View
Written by Sarah Edge
I am a Counsellor Psychotherapist, specialising in postnatal mental health in the United Kingdom. I am also a Mum of two small children. I recently wrote a guest blog on “The Process of Healing From Infant Feeding Trauma, Guilt, and Shame: When You Wanted To Breastfeed and Couldn’t” for the Fed is Best Foundation, and when I was asked to write again, I jumped at the chance. In this piece, I aim to examine the Fed is Best message through my therapist’s lens and discuss why the Fed is Best message is an essential part of healing and recovery.
Is My Baby’s Weight Loss Normal Or Excessive?
The Newborn Weight Loss Tool can provide an answer.
Parents are taught that it’s normal for babies to lose 7–10% of their body weight in the first few days after birth, but is this true? Well, that depends. According to the AAP, a baby who loses more than 7% of his body weight may be losing excessive weight and requires a comprehensive lactation evaluation to rule out delayed onset of copious milk production, primary lactation failure, and/or infant oral anomalies that prevent adequate colostrum/milk transfer.
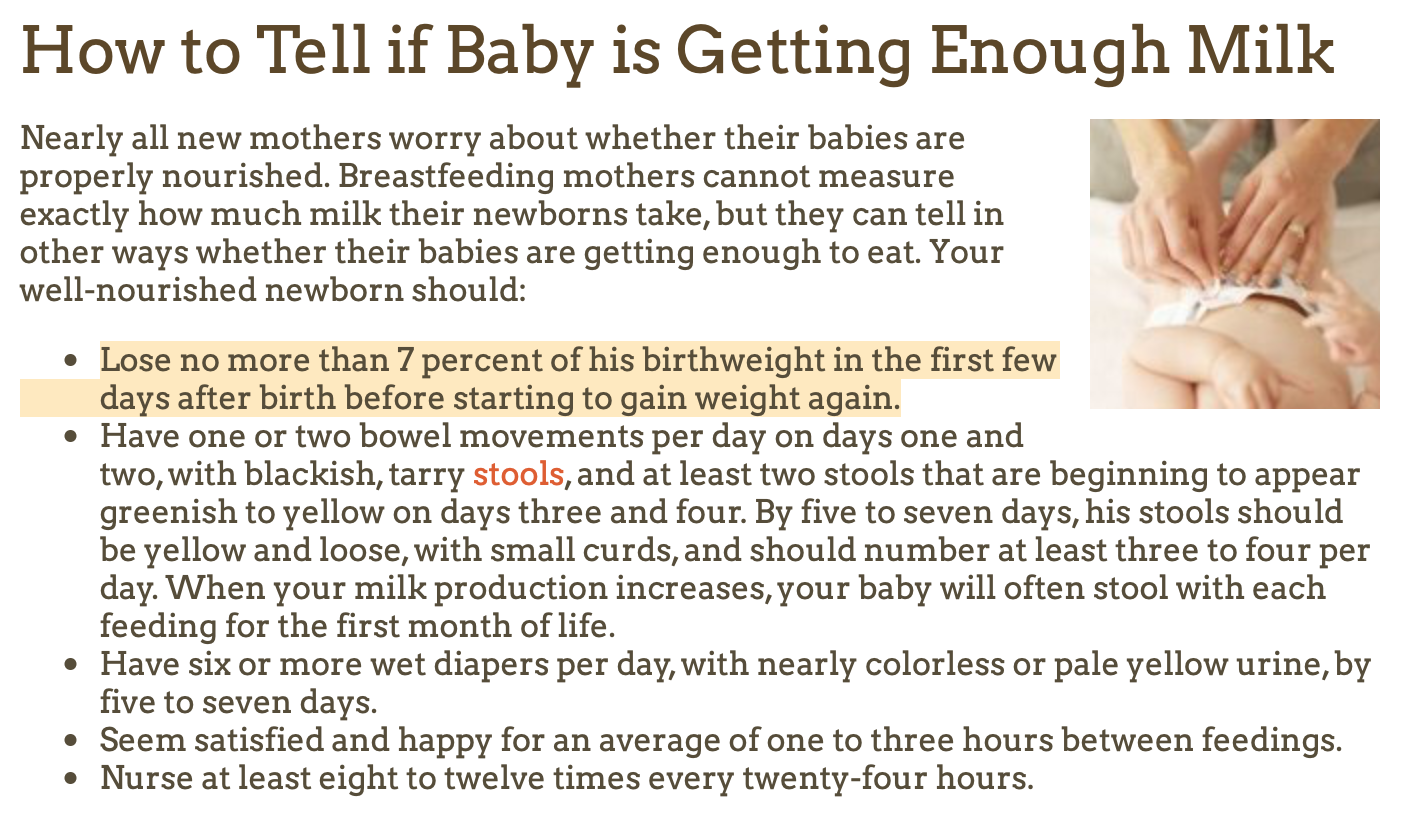
From the American Academy of Pediatrics HealthyChildren.org website. Breastfed newborns should lose no more than 7 percent of birth weight in the first few days after birth before starting to gain weight again. (Accessed July 16, 2020)
Weight loss has typically been assessed using simple percentages, but now there is a much more precise and accurate way to track excessive weight loss in newborns and many hospitals, pediatricians, and lactation consultants are adopting this method for greater accuracy in making clinical recommendations. The Newborn Weight Tool, or NEWT, is an online tool, the first of its kind, to help pediatricians determine whether exclusively breastfed newborns have lost too much weight in the first days of life. The tool was developed at Penn State College of Medicine through research conducted jointly with University of California, San Francisco. It was developed using a research sample of hourly birth weights from more than 100,000 breastfed newborns. For a quick synopsis of this tool from the lead investigator and one of developers of the tool, Dr. Ian Paul, watch the video below.
Source: Penn State Health News
In this video, Dr. Ian Paul, professor of pediatrics and public health sciences at Penn State College of Medicine and pediatrician at Penn State Hershey Children’s Hospital, talks about how NEWT fills an important void. Determining whether an exclusively breastfed newborn is losing excessive weight is important because higher weight loss almost always reflects suboptimal milk intake. It is also associated with increased risk of medical complications such as low blood sugar, jaundice, and dehydration, which can result in the need for medical interventions and future health and developmental problems. This weight-loss tool shows that how quickly babies lose weight is just as important as how much they lose.