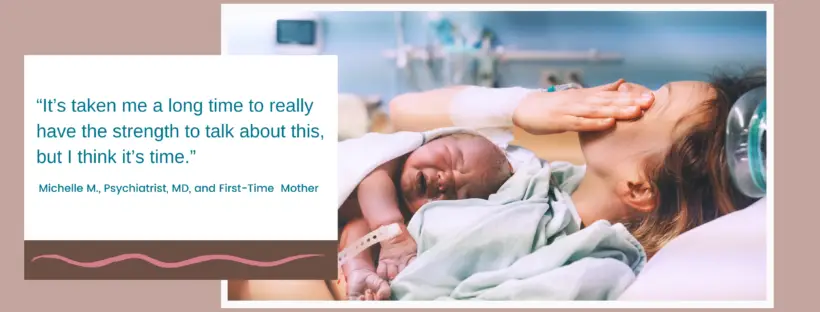
I didn’t have the easiest pregnancy; for one thing, I was considered a geriatric pregnancy, given that medicine was my second career, and I waited until after residency to get pregnant.
I also have a history of depression and anxiety; thankfully, my depression was under control during pregnancy, but my anxiety certainly wasn’t – it worsened when I learned I was diagnosed with gestational diabetes (likely due mainly to my advanced maternal age).
In my mental preparations to have my baby, there was one thing I was always sure of: I would certainly attempt to breastfeed my child, but if it didn’t work out, that would be okay because, in my clinical experience, formula-fed babies did just fine. Furthermore, from the years of my struggles with my mental health, I learned the importance of choosing my battles, and it simply wasn’t worth it to me to agonize over breastfeeding if it didn’t come easily. Continue reading