Hello,
I saw on your website that you guys are encouraging parents to share their feeding journey and I thought I would share mine.
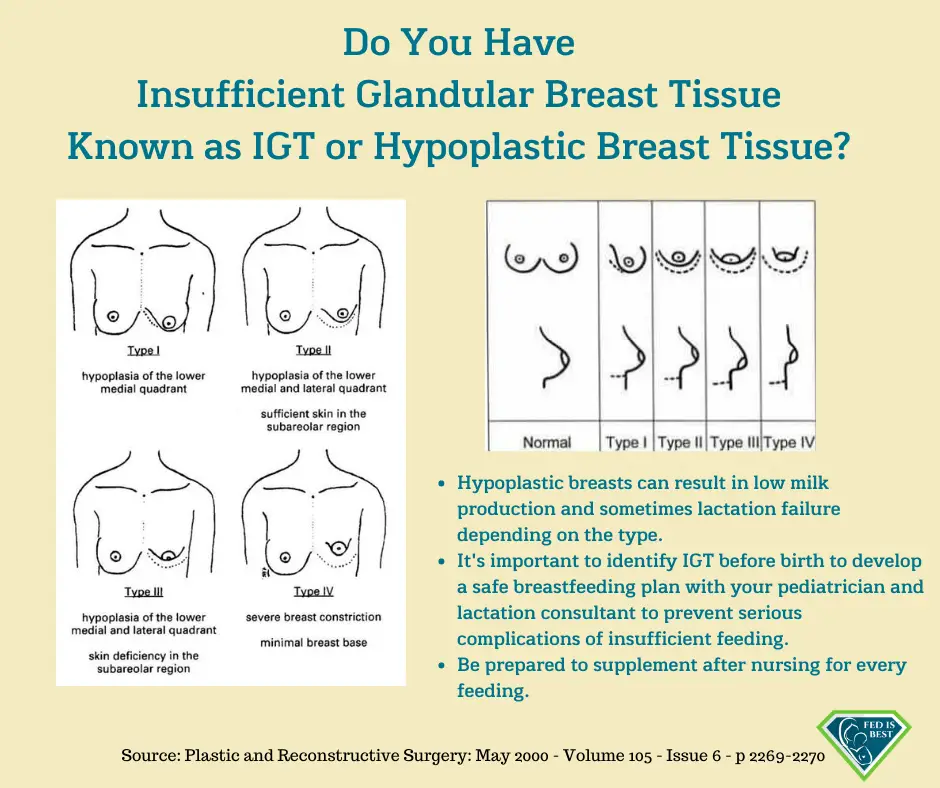
My baby was born March 6, 2021, after 48 hours of labor which resulted in a c-section, just shy of 39 weeks gestation. She was 6 pounds 3 ounces and healthy as can be. My plan was always to breastfeed, so the lactation consultants (LCs) in the hospital helped me right away with latching. We discovered a tongue tie and that was corrected when we left the hospital.