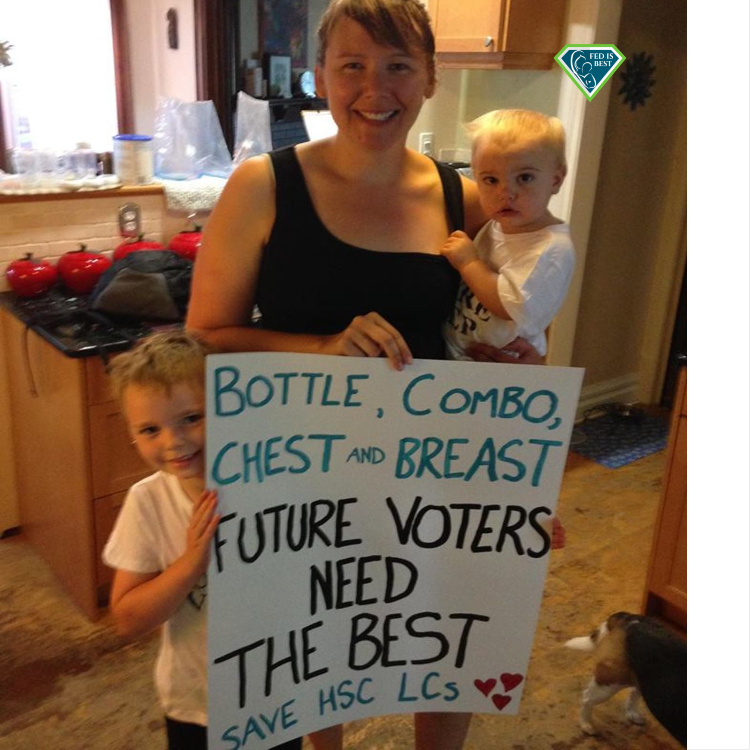
“The sight and sound of babies crying out for food and fluids are why I decided to speak out. Babies are denied food and fluids to promote exclusive breastfeeding.”
As a mother-baby nurse, I’ve seen many preventable episodes of emotional distress for families in my thirty-year career. Unfortunately, The emotional distress increased significantly when the Baby-Friendly Hospital Initiative was implemented at my hospital. Some episodes of emotional distress are unforgettable, so I felt compelled to speak out about them, hoping to bring about the much-needed change to protect newborns from hunger and maternal mental health.
Mothers are incredibly vulnerable after giving birth, as their bodies transition physically and hormonally. They have a new life to take care of while recovering from birth and require compassionate, respectful, and individualized care. However, the Baby-Friendly breastfeeding protocol is one-size-fits-all and does not allow individualized care. Mothers must follow the BFHI protocol regardless of how they feed their baby or how complicated their birth was. We know as health care professionals that no protocol can be safe and effective without individualized care.
Evidence based medicine cannot replace clinical judgment or account sufficiently for the complexity of individual cases. The limitations of EBM must be acknowledged and addressed so that it can be used effectively and without compromising patient care. -Mark R. Tonelli, MD, MA