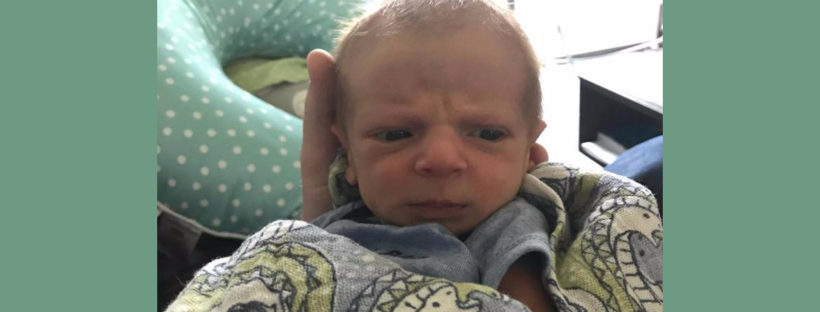
My name is Amber, and I am the mother of a charming, beautiful, and vivacious baby boy. I want to share with you a story: the story of my son’s birth and his first few months earthside. It is a multidimensional story full of love and heartbreak, but I think it’s important that other new mothers hear it. I hope they will know they are not alone if their early motherhood experiences are not what they always dreamed of.
I was working in an emergency room as a nurse and heading into my second-to-last semester of school to become a nurse practitioner. My husband and I had only been trying to conceive for a month. Because I have polycystic ovary syndrome (PCOS) and irregular periods, I figured getting pregnant would take longer, but there I was on September 1 with a positive test. We were ecstatic. As a planner, I spent most of the next nine months thinking about and planning everything about my son’s birth. I consider myself a well-educated woman and medical professional, so it was no surprise that the heart of my plans included breastfeeding my son. I spent months researching the best pumps for when I had to return to work, deciding on a storage-and-feeding set, and learning about ways to strengthen the breastfeeding bond. Formula feeding never crossed my mind. After all, I was always told breast was best. Sure, I had some friends who gave some formula here or there, but I just knew I would be one of the ones who would exclusively breastfeed and pump for my son. Continue reading