Good information isn’t always enough to overcome bad systems.
By Sarah Christopherson
I wrote this article in late 2018, a few months after giving birth to my daughter. My experience at my “Baby Friendly” hospital was traumatic and it was painful to relive, but I felt like I could help other new parents by telling my story, and it seemed like a good match for the work I was doing professionally to dismantle coercive systems that deprive women of their autonomy.
At the time, I was the policy advocacy director for a national non-profit focused on empowering women as they navigate healthcare in the US. My article was printed in our organizational newsletter in early 2019 and published on our website.
It was shared by Fed Is Best, which also interviewed me. From time to time, I would send the link to expecting parents, not to scare them, but to empower them to stand up for themselves when they sensed that something wasn’t right. It helped me to help others. And telling my story made a difference.
A friend who gave birth in the same hospital texted me, “Your article helped me so much when I was having trouble breastfeeding. I look at the pictures of [my son’s] early days and think about how it would have gotten worse if I hadn’t talked to you and others. I started supplementing with formula early AND I signed that dumb form without blinking. The post-partum period exhausts you so that normal problems you would easily solve seem so much harder… and then you’re dealing with some of the most consequential decisions you’ve ever had to make. It was the things I’d already thought through a bit—like the stuff in your piece—that I was prepared to tackle.”
Eventually my non-profit changed leadership and I moved into a different policy field. My infant turned into a happy, healthy, precocious, and articulate 6-year-old bouncing ball of energy. And that’s where I thought things ended.
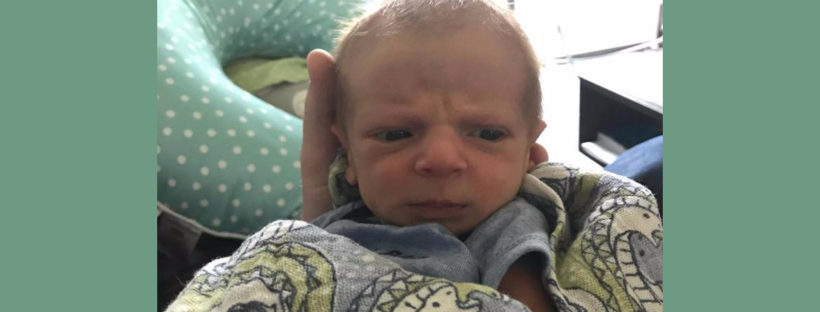
Until last week, when I discovered that without my knowledge or permission, my former organization had rewritten my article in January. They’d kept my name, my story, and the picture my husband took of me in a hospital gown holding my infant daughter on the day she was born. But they’d stripped out paragraph after paragraph that cautioned against breastfeeding coercion.
Gone was any mention of the scientific literature suggesting that the benefits of breastfeeding had been overhyped. Gone was Laura Dorwart’s first-person account of her own disturbing experience in a “baby friendly” hospital. Gone too was the brief nod to Hannah Rosin’s cautionary note that exclusive breastfeeding had played a role in creating lasting inequities in her marriage over caretaking responsibilities.
But cutting out what I wrote wasn’t enough. Their editors also put words in my mouth that I would never say: “Breastfeeding is still considered best for baby and mom, but feeding your baby formula will provide your baby with the same nutrients to thrive.” And sure, saying that makes sense after you’ve cut out every mention of where breastfeeding isn’t best for baby and mom.
Seeing this new article, this breastfeeding propaganda article, under the picture of my sweet little baby who became so dehydrated from breastfeeding coercion that the nurses had to slice and slice and slice her little heel and still couldn’t get enough blood to fill a pen cap… I started to sob, deep, wrenching sobs. I felt violated. I felt betrayed. I demanded that they take the article down immediately. They complied, and my story disappeared from the internet, as though it had never happened. Until today.
Originally Published: Feb 6, 2019
The decision to breast- or formula-feed is a highly personal one, with the right answer varying parent to parent. But this is not an article about the benefits of breastfeeding or about concerns that previous studies may have exaggerated those benefits.
This isn’t an overview of the long history of bad behavior by formula companies or the Trump administration’s politically motivated refusal to endorse a 2018 World Health Organization resolution promoting breastfeeding. Nor is it a discussion of the feminist case for formula-feeding made by Hanna Rosin and others.
Rather, this is a story about what happens when good information isn’t enough to overcome bad systems. But first, some background.
I’m white, middle-class, and well-educated—with all of the status and privilege that affords. This is my third child, I work in health policy, and I already had a pretty good sense of the medical literature on breastfeeding when I walked into the maternity ward.
Before joining the National Women’s Health Network, I spent a decade as a senior aide to two members of Congress, so I’ve had a lot of experience telling powerful people why they’re wrong. In short, there aren’t many patients better positioned to stand up for themselves and their children.
And yet, I didn’t. Or at least not until my daughter was so dehydrated she couldn’t give enough blood to fill a pen cap.
Arrival of the “Baby Friendly” Hospitals
When I gave birth for the first time, the “baby friendly hospital” movement was still in its infancy in the United States. It wasn’t until 2010 that the U.S. Department of Health and Human Services endorsed its ten principles, including:
#6 “give infants no food or drink other than breast-milk, unless medically indicated.”
#7 “practice rooming in” (the term for when a baby sleeps in the mother’s hospital room during her recovery instead of in the hospital nursery),
#9 “give no pacifiers or artificial nipples to breastfeeding infants,” and
(The WHO formally dropped their prohibition on pacifiers in a 2018 update, but as of this writing in 2019, the Americans haven’t caught up.)
However well-intentioned, these principles—imposed on exhausted parents by hospital staff and backed up by a tangle of bureaucratic rules and incentives—can quickly turn coercive in practice.
As the Washington Post reported in 2014, “If a mom wants to send her newborn [to the nursery], staff members often have to ask why and then fill out paperwork explaining the reason. … Formula may be provided, but only on request, and only after, in some instances, mothers sign a waiver acknowledging that using a bottle could impede breast-feeding. Lactation consultants roam the floor.” [emphases mine]
“full compliance with the 10 steps of the initiative may inadvertently be promoting potentially hazardous practices”
Writing in JAMA Pediatrics in 2016, pediatricians Joel L. Bass, Tina Gartley, and Ronald Kleinman warned that “there is now emerging evidence that full compliance with the 10 steps of the initiative may inadvertently be promoting potentially hazardous practices and/or having counterproductive outcomes.”
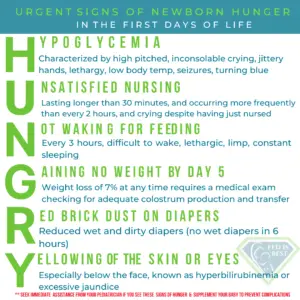
The article highlighted the dangers of mandatory rooming-in and unsupervised skin-to-skin contact when mothers are exhausted or medicated and called into question the practice of banning pacifiers when pacifiers have been shown to reduce the incidence of sudden infant death syndrome (SIDS). It also raised concerns about coercing mothers into exclusive breastfeeding.
Starving My Baby
I first noticed things weren’t right 24 hours after giving birth. My daughter was too sleepy to nurse longer than a few weak tugs on my breast and none of the lactation consultant’s tricks would rouse her. With my other children, I’d satisfactorily supplemented nursing with formula during my hospital stay so I asked for a bottle.
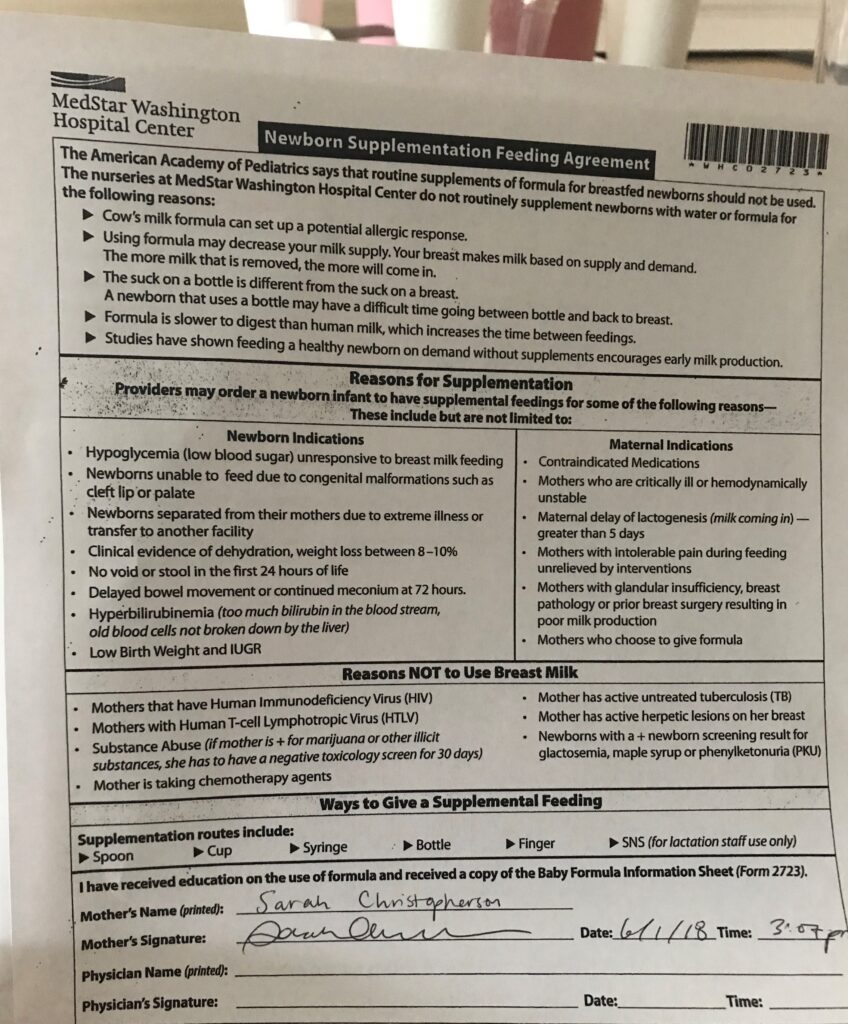
The nurse was stern and disapproving. If I wanted to “give up” on breastfeeding, I’d have to sign a waiver acknowledging all of the risks associated with my terrible choice. “Reasons for supplementation” listed on the form include “mothers who are critically ill,” have “intolerable pain during feeding unrelieved by interventions,” or have “breast pathology.”
For mothers who simply choose to supplement, the form makes clear: “The American Academy of Pediatrics says that routine supplements of formula for breastfed newborns should not be used.”
Recovering from a C-section, I was dependent on hospital staff for my food and pain medication, and even assistance using the bathroom. Interrupted every hour for two straight days by a seemingly endless parade of doctors, residents, nurses, techs, and support staff—all with their own, uncoordinated schedule of rounds—I had the jellied zombie brain of a torture victim.
I signed their form… but then I didn’t use the formula!
Maybe I’d better speak to the pediatrician first, I thought, see if I’m overreacting to my baby’s listlessness before I give her an allergy, destroy my milk supply, or risk any of the other horrors of formula supplementation described on the waiver.
I asked to see the pediatrician, but the nurses sent me the lactation consultant instead.
And so I delayed for another day, with a signed form and a pack of ready-made formula within reach but too cowed to go against the hospital staff who controlled every aspect of my existence.
Looking back now, it’s incomprehensible to me. Dehydration in newborns can lead to blood clots, strokes, brain swelling, permanent brain damage, and death. I should have fed my baby right away, and I knew it, and yet somehow I didn’t do it.
“Cut, squeeze, repeat, while she screamed in pain and I watched helplessly.”
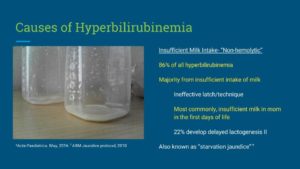
Fortunately for the two of us, jaundice set in first, and with it the need to draw blood for a bilirubin test. The nurses cut my daughter’s heel, she screamed weakly, they squeezed her little foot to express the blood, and collected a single drop. Then the cut quickly clotted closed.
So they had to do it again.
And again.
And again.
Cut, squeeze, repeat, while she screamed in pain and I watched helplessly.
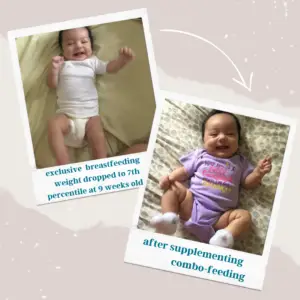
They only needed to collect a tiny vial’s worth, smaller than a pen cap, but she was far too dehydrated. She’d lost 15% of her birthweight by then. After twenty agonizing minutes, they handed my tiny girl back to me. I flung open the cabinet and attached nipple to bottle with shaking hands. With that first sip, her eyes shot wide open and her tiny hands flew instinctively to the sides of the bottle. She responded like a starving person eating for the first time in her life. Which, of course, she was.
It Doesn’t Have to Be This Way
In the months since leaving the hospital, I’ve I thought a lot about how the hospital’s systems were structured, intentionally or not, to strip me of my own decision-making power. Good information is a necessary component of good health outcomes, but it’s not sufficient so long as patients aren’t empowered to follow through.
As Laura Dorwart wrote in The Week about her own experience in a “baby-friendly” hospital, the issue is one of “parental consent within a medical context that too often presents itself as a top-down hierarchy: hospital administration, doctor, nurse, baby — and mother last. Dead last.”
It doesn’t have to be this way. To ensure the well-being of both mother and child, hospitals should:
- coordinate routine nighttime schedules to better support patient recovery since sleep-deprived patients can’t advocate for themselves as effectively
- scrap policies that implicitly or explicitly punish staff—say, with extra paperwork—when a parent asks to use the nursery or wants to formula feed, ensuring instead that policies are bureaucratically neutral and let the patient lead
- eliminate misleading and coercive forms and materialsthat exaggerate the harms of formula feeding while dismissing the potential harms of breastfeeding
- prioritize the parent’s mental health and physical recoveryas highly as maintaining breastfeeding exclusivity
In my professional work, I train health providers on the need to listen to their patients to avoid the pitfalls of coercion. But it wasn’t until I fed my starving child for the first time that I really understood.
Sarah Christopherson was the Policy Advocacy Director for the National Women’s Health Network from 2016 to 2021.