Is that some kind of sick joke? Infant formula is safe nutrition—scientifically created to replace human milk and thus consists of fluids and nutrients necessary to nourish a baby. Brain damage is irreversible. That should be glaringly obvious, but it looks like the AAP Breastfeeding Section responsible for the recently released “Breastfeeding and the Use of Human Milk” (June 2022) has lost sight of this critical fact.
Let’s focus on this appalling statement:
“The need for phototherapy in an otherwise healthy infant without signs of dehydration and/or insufficient intake is not an indication for supplementation with formula unless the levels are approaching exchange transfusion levels.”
Hyperbilirubinemia (excessive jaundice) and Phototherapy
To explain why we are horrified, let’s look carefully at what the statement means. Jaundice is a common and usually benign condition experienced by about 60% of healthy newborns. It is caused by a substance called bilirubin, a breakdown product of fetal red blood cells after birth to transition to mature red blood cells. However, if a baby’s bilirubin levels are greater than a certain level and continue to climb, the risk for brain damage increases.
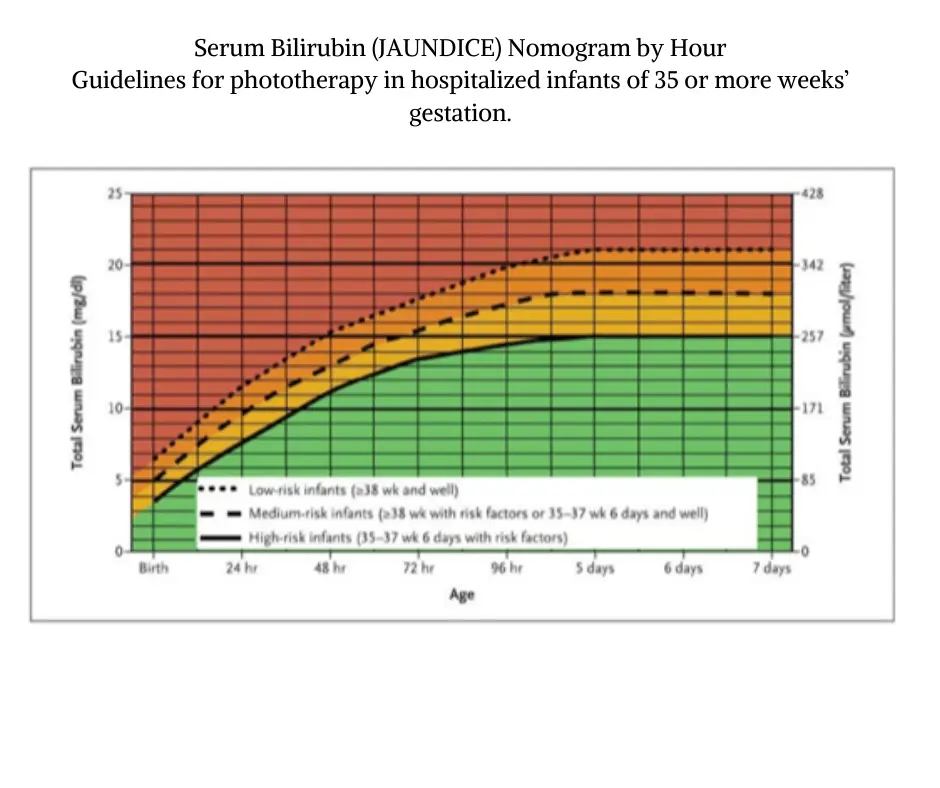
A baby should never be allowed to experience a dangerous bilirubin level, and all interventions should be utilized to bring the levels down quickly!
There is, however, a cost-effective preventable intervention available—it’s called adequate feeding of donor milk or infant formula with a bottle which is the absolute BEST way to reduce bilirubin levels. It also provides comfort for a baby who is lethargic, hungry, thirsty and has dry, chapped lips and mouth. Multiple blood checks will also be necessary to monitor bilirubin levels, which are painful for newborns.

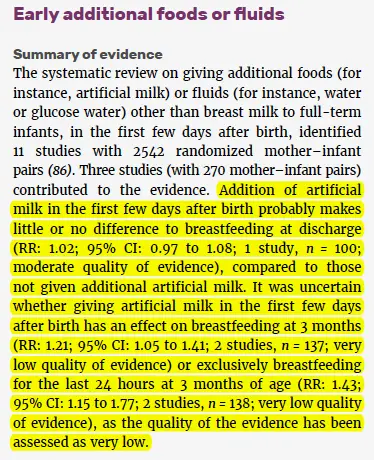
To be clear, supplementation does NOT interfere with exclusive breastfeeding. Exclusive breastfeeding can be resumed when the full milk supply has come in after the danger has passed. Brain damage can never be undone.
Source: The World Health Organization
This video educates parents about newborn jaundice and the importance of supplementing.
brain-threatening Jaundice is preventable
Jaundice high enough to require phototherapy happens to about 15% of newborns (according to a large 2018 study). Prevention of phototherapy from insufficient breastfeeding can be prevented with temporary supplementation.
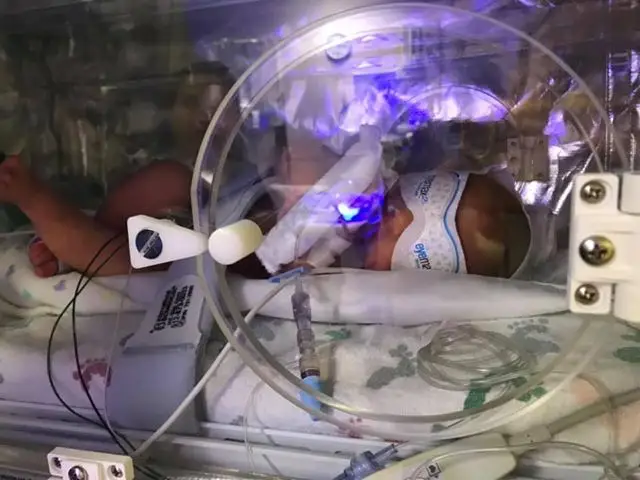
Ella (now two years old) was one of these newborns. (Her mother, Becca shared her story with us in 2019, after her baby experienced multiple complications of insufficient milk, while she received loads of professional advice not to supplement.) Ella wouldn’t have been supplemented with formula under these guidelines because her jaundice wouldn’t have been considered severe enough. Her pediatrician would probably disagree, given that he’s watching her closely for suspected developmental delay—a known complication of severe jaundice:
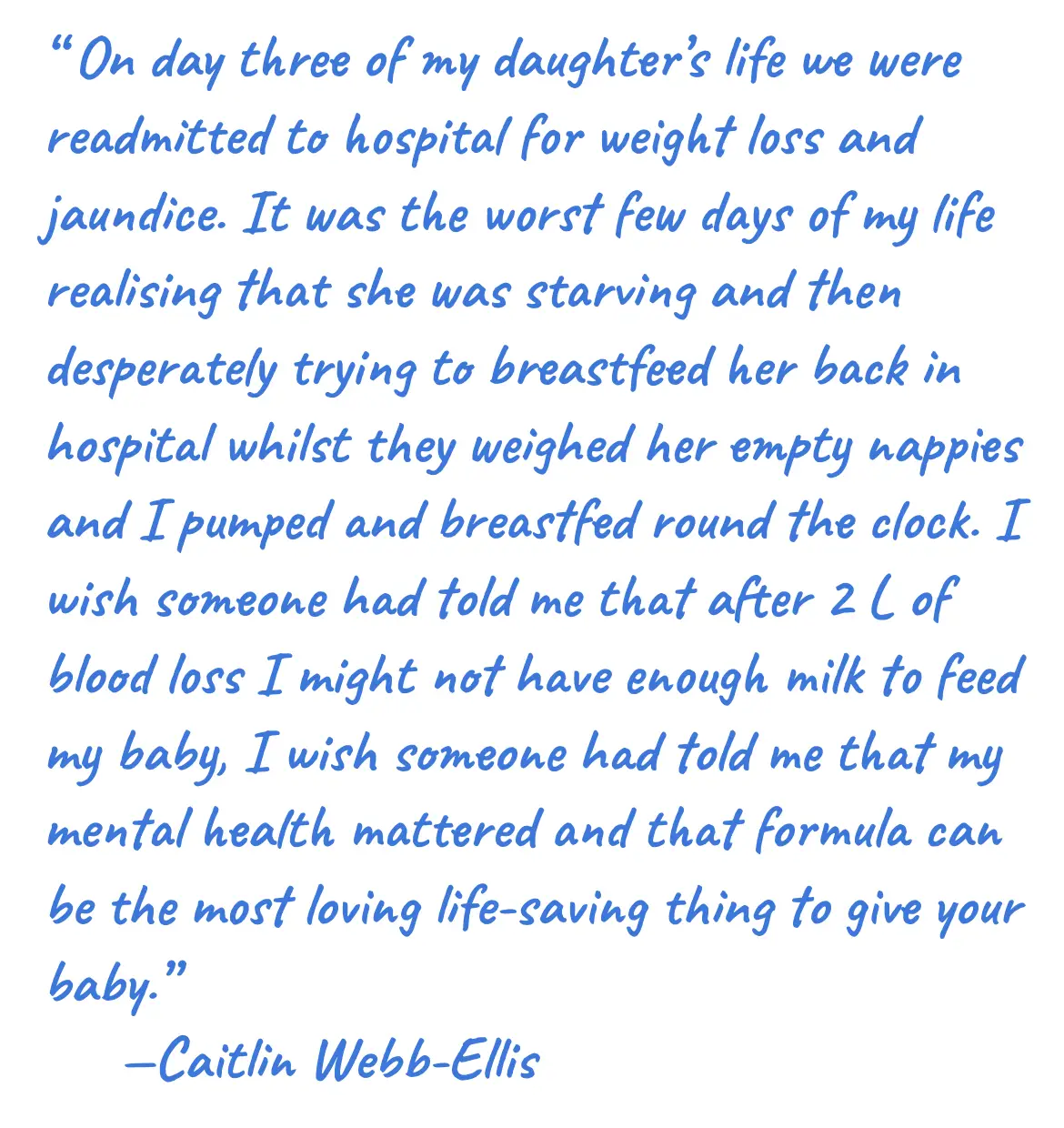
Becca (Ella’s mother) and other parents of babies who experienced high bilirubin levels have to live with the knowledge that their babies didn’t get enough to eat and that it may have affected their brains. The psychological trauma of this cannot be overstated.
Medical Ethics: “do no harm” and informed consent
Rarely are parents told that increased feeding from supplementation with formula (or banked donor human milk if available) can prevent as well as reduce high bilirubin levels, shorten the need for costly and emotionally grueling hospitalizations, and most importantly, reduce their baby’s exposure to a substance that damage brain cells.
Instead of emphasizing the dangers of excessive jaundice, the guidelines claim that the higher bilirubin levels commonly found in exclusively breastfed newborns may be beneficial because bilirubin is an “antioxidant.” Studies on excessive jaundice are very clear—high bilirubin levels can result in developmental delay, cognitive impairment, and behavioral and psychiatric disorders. There are simply no facts—none—to support their idea that there are benefits.
In every other area of medicine, patients (and parents of patients) receive informed consent and counseling about their options, especially when a serious complication like excessive jaundice can occur. However, providing this information is not currently standard practice. In reality, the failure to fully inform parents of the causes (e.g., insufficient milk intake) and risks of newborn jaundice commonly result in parents going home believing they are doing what is best for their infants by avoiding formula supplementation. If their infant does not receive enough milk because the milk comes in late or it is not enough, then they may find a distressed or lethargic jaundiced, and dehydrated baby that now requires hospital admission for conditions that can cause permanent disability. It is unbelievable—yet true—that parents aren’t being informed that insufficient feeding problems and jaundice are currently the leading causes of newborn rehospitalization.
This lying by omission is an outrageous violation of patient rights.
Parents should be told that temporary supplementation in response to signs of infant hunger and jaundice can prevent and treat these complications. Supplemental milk, whether it be formula or banked donor milk, can reduce bilirubin levels in both insufficiently fed babies and babies who have excessive bilirubin due to other medical conditions (like blood type incompatibility) because elimination through digestion is the way babies remove bilirubin.
While exclusive breastfeeding can be resumed when the full milk supply has come in, and the danger has passed, brain damage can never be undone.

Sydney F.’s baby was supplemented for five days using our feeding plan, then exclusively breastfed. She is still breastfeeding at 11 months.
The authors’ concern seems to be that if parents are made aware that breastfeeding isn’t perfect, they might entirely stop. Or worse, parents may come to believe that there can be benefits to supplementing some breastfed babies with formula (especially jaundiced newborns) and that the narrative that exclusive breastfeeding is best for all babies (with rare exceptions) is false.
Parents can understand the concept of a temporary nutritional intervention to bridge the gap until their supply increases and how this can protect their baby and support continued breastfeeding. In other words, you don’t have to choose between breastfeeding and reducing your baby’s risk of excessive jaundice—you can do both!
Five well-designed studies suggest that they do understand this and that breastfeeding isn’t destroyed with temporary small supplements. How many clinical trials have shown that judicious supplementation impairs sustained breastfeeding? None. Regardless—and this is important—what gives anyone the right to withhold information because it might change how a parent chooses to feed their child?
WHEN PHOTOTHERAPY ISN’T ENOUGH: EXCHANGE TRANSFUSIONS
The American Academy of Pediatrics—the authority that advises all pediatricians—now recommends that pediatricians should not offer formula supplementation for jaundiced babies receiving phototherapy without signs of “dehydration and/or insufficient intake,” which they do not define until they are “approaching exchange transfusion levels.” An exchange transfusion is essentially a blood transfusion done when a jaundiced baby’s blood has become so toxic from high bilirubin levels that they risk severe brain damage, a condition called kernicterus.

Baby Finn was set up for a blood transfusion for jaundice. Photo by Jim Campion (his father) via Flickr
“Signs of dehydration” range from a slightly dry mouth to total lack of urination and a sunken fontanel (soft spot on babies’ heads). “Insufficient intake” can mean anything from insufficient to make the baby full and comfortable to only enough milk to keep the baby out of danger. We assume they mean the latter, as the Academy of Breastfeeding Medicine, which sets the standards for newborn exclusive breastfeeding management under the Baby Friendly Hospital Initiative endorsed by the AAP guideline, says that if supplementation is necessary, only 1–3 teaspoons (5–15 ml) on days 1 and 2 should be given, respectively. This is despite evidence that the newborn stomach is 20 mL at birth and that much higher volumes of supplemental feedings than they recommend actually reduces rates of jaundice readmission.
How much milk a baby needs: Milk Calculator
How can the AAP discourage pediatricians from offering parents the choice to reduce their child’s bilirubin levels with formula when supplementing can rapidly reduce bilirubin levels, shorten the need for phototherapy, and prevent levels that can require a blood transfusion for any baby with high bilirubin levels?
Studies have shown elevated markers of brain injury in the blood occur by bilirubin levels of 19 and 20 mg/dL. Large studies have shown increased risk of developmental problems, cognitive impairment, speech/language impairment and behavioral problems in newborns who develop high bilirubin levels, even in the moderate range of 13.5–19 mg/dL, well below the threshold for exchange transfusion. These impairments are from BIND—bilirubin induced neurological dysfunction—which is less severe than kernicterus, but still seriously disabling.
Have they ever met a parent whose child has to live with the lifelong disabilities caused by kernicterus, as shown in this video?
Anyone familiar with the devastating impact of kernicterus would not be so casual about jaundice; in fact, they would be outraged at the suggestion in this report.
How can the AAP be trusted with making recommendations on infant feeding when they appear to have lost perspective on what constitutes safe versus unsafe conditions for infants?

Chloe’s baby Lucas
Can we all agree that infant formula is far better than the risk of brain damage? Can we at least let parents know these facts and put the decision in their hands? Can we please prioritize protecting babies’ brains over avoiding formula?
Written by Lynnette Hafken, MA, IBCLC, with Christie del Castillo-Hegyi, MD, and Jody Segrave-Daly, RN, IBCLC (Retired)
Resources