My feeding journey was not at all what I envisioned for my little one and me. When I was pregnant with my firstborn, I heard stories from my mom that she never used a bottle with my brother and me. When I researched breastfeeding, parents were told how wonderful and natural it is. I believed breastfeeding would come naturally.
The day my son was born was a whirlwind. I had to have a c-section due to complications, but we were so excited to meet him. The first few days, I tried to get him to latch on, and he would stay for a little while and then unlatch. I felt uneasy that he wasn’t getting enough colostrum, but the medical staff told me I was doing great. My husband and I were so focused on getting breastfeeding down that I forgot to get pictures of me and my little one. My focus was getting him fed the right way. Sometimes, nursing hurt so much that I would dread it when it was time for feeding. The on-site lactation consultant came the day after the c-section. She was with me for an hour and told me everything was wonderful!
After she left, my baby would cry, and I knew something wasn’t right. My husband and I decided it was time to ask for formula. When we asked, the nurse kept asking us if we were sure. As first-time parents, we questioned if we were doing the right thing.
I was so exhausted and needed rest that my husband decided to feed my little one formula. Another nurse came in and said, “Dad! Don’t! Breastfeeding is the way! Don’t do that to your little one. Your wife is doing great.” She grabbed the formula from my husband’s hands and stashed it in a cabinet. My husband and I looked at each other in shock, and I tried to breastfeed again.
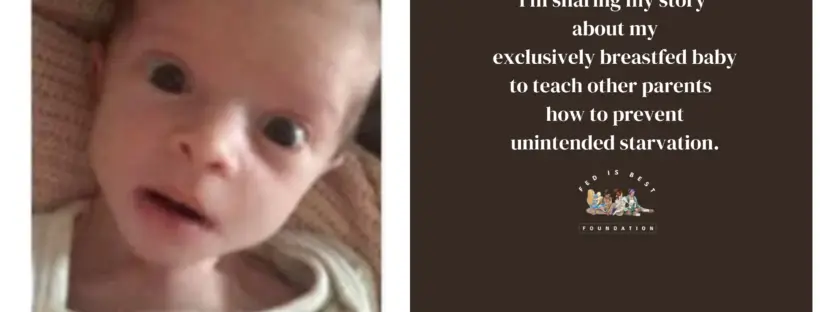
We were discharged on a Friday, and over the weekend, my son cried a lot, and I thought he might be a fussy baby. On Monday morning, we saw that my son had orange urine in his diaper. I lost it. I remember holding him and crying, blaming myself. We went to the doctor’s office and were told that he was dehydrated. He also lost a lot of weight, more than he should have, and my doctor suggested it was time to supplement my baby with formula.
Then came the day that changed my mental health forever.
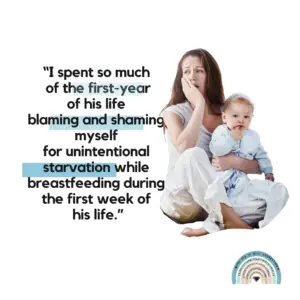
After that, I cried for hours, and I could not get over the guilt. I kept thinking: “Why didn’t I know he was hungry or not getting enough? How could I have let my baby starve?” The guilt stayed with me for months and was the catalyst for my debilitating postpartum depression and anxiety diagnosis.
After that, I became obsessed with feeding my son. I would write down how many ounces of formula or breastmilk he had and at what times. I no longer breastfed, but I pumped, so I knew exactly how many ounces he was consuming. Even when he was a few months older, I would still wake him up to feed him because I thought he would become dehydrated again. I hated when my little one would cry because it would be a reminder of the terrible weekend of his life, and I would break down, and I would cry.
My husband and I hope to have another little one, and I know what I would do differently. I feel guilty that my little one had a rough start on his feeding journey, but I try to remember that we were both learning and following the advice of medical professionals in the hospital.
I can’t tell you how much I appreciate Fed is Best Foundation and their work. I honestly don’t know what would have happened to me without finding your support community. I got so emotional writing my story. Thank you for being there for mothers and babies.
Warmly,
Maria

FREE infant feeding resources:
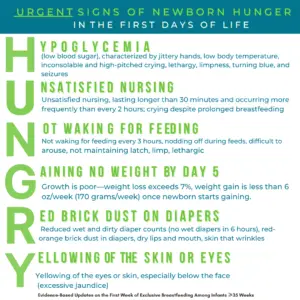
Knowing if Your Newborn is HUNGRY and Needs Urgent Evaluation / Supplementation – Fed Is Best
Safe Infant Feeding Resources (fedisbest.org)
Fed is Best Feeding Plan – Updated 2024 – Fed Is Best
Pre-order our new book being published June 25th, 2024 : Fed Is Best Book – Fed Is Best Book
How to Breastfeed During the First 2 Weeks of Life – The New York Times (nytimes.com)
Contact Information – The Fed is Best Foundation