My name is Sarah Edge, and I am a counsellor psychotherapist and mum of two. After my experience with breastfeeding trauma, guilt, and shame, and the associated decline in my mental health after the birth of my son, I was motivated to start my own practice specialising in postnatal mental health.
I suspect that most of you reading this are doing so because you have your own experience of infant feeding guilt or trauma, where breastfeeding didn’t work out how you had planned. My personal story is a tale as old as time. My son was born late preterm, healthy but sleepy and unable to latch. He developed significant jaundice and low blood sugars, resulting in us returning to the hospital, and him being admitted onto the children’s ward at five days old.
I tried everything to breastfeed: nipple shields, continuous pumping, cup feeding expressed breast milk, triple feeding, lactation consultants, and infant feeding professionals. I had alarms set every 90 minutes to feed my son, and I kept this up for almost two weeks without any results. His feeding consultant then prescribed him formula milk, and he began to thrive. He was happy and healthy, and we returned home to start our lives as a family of three, this time formula feeding him.
My baby was finally thriving but I was not. I was left with so much sadness, jealousy, disappointment, and animosity towards breastfeeding. World Breastfeeding Week was unbearable, as the social media pages were flooded with beautiful photos of babies at breast, and seeing other women breastfeeding sparked this intense and animalistic jealousy I had never felt before.
So why was I left with all this sadness?
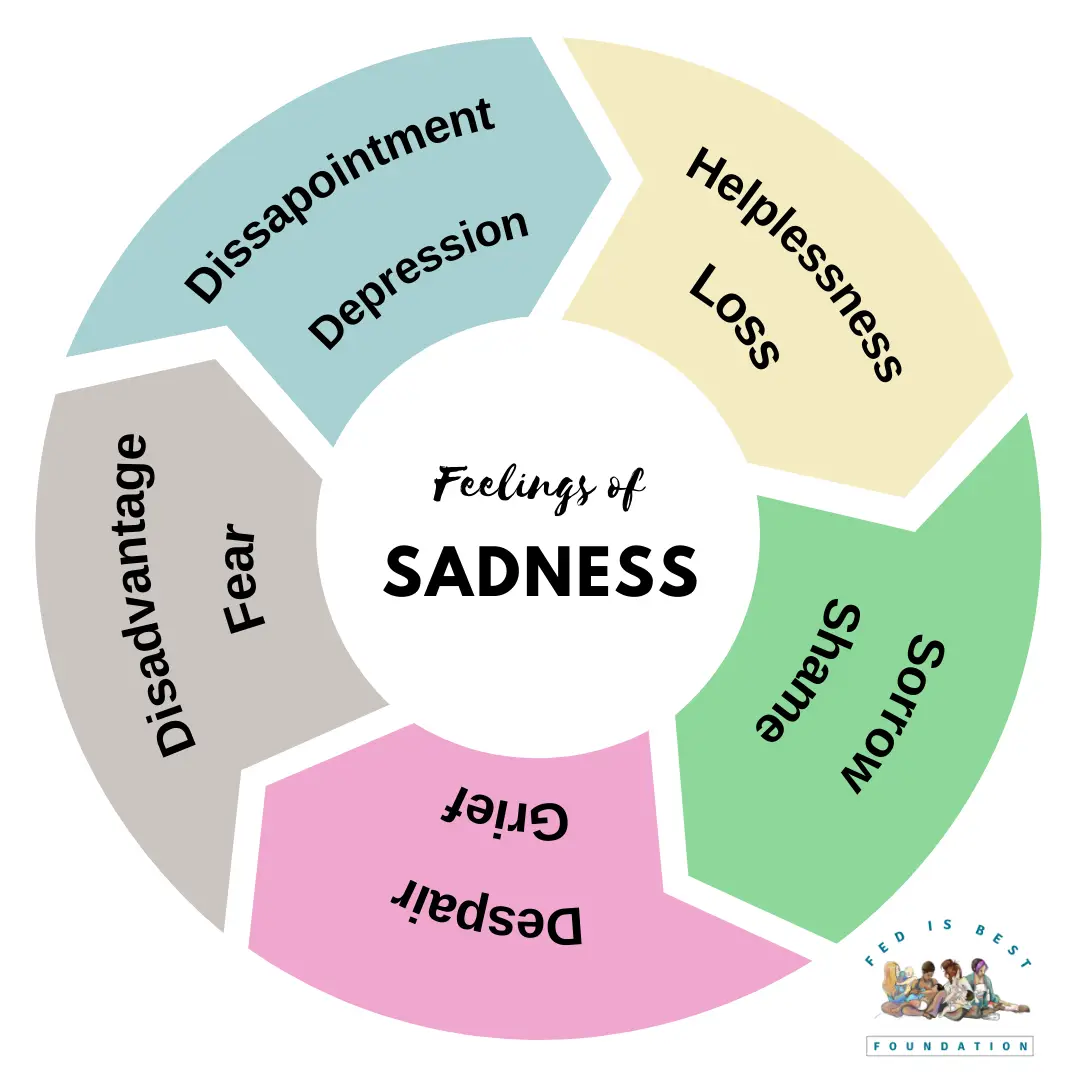
Sadness is an emotion that is associated with feelings of loss, sorrow, depression, grief, guilt, disappointment, shame, despair, helplessness, fear, and disadvantage. It can be difficult to shake and needs to be processed.
I was personally experiencing grief. I had suffered a loss. Breastfeeding was important to me, and my feelings were—and are—absolutely valid.
No matter the reasons you could not breastfeed—and there are countless—you are allowed to mourn the loss of breastfeeding. Just because your baby is thriving without breastmilk doesn’t mean you don’t deserve to grieve or ask for support or comfort, especially if healing has been difficult.
What I have found with my professional experience is that all women need to feel heard, and their loss must be acknowledged. All the women that have shared their stories with me have had the same thing in common—they were left with a strong feeling of sadness. It didn’t matter if they had stopped breastfeeding after five minutes or five months, if it was earlier than they had wanted and planned, they experienced feelings of sadness.
In my personal and professional experience in seeing breastfeeding heartbreak play out, I have found it helpful to approach these feelings as I would trauma and/or grief.
THE GRIEF PROCESS
Grief is experienced and processed differently by all of us. I do not want to be prescriptive in how to heal from this, nor am I pretending there is a right way to do it. But we can talk about steps to healing, and how to recognize if you may need professional support.
Acknowledge your loss
Try saying “I have suffered a loss and have been through a lot; it is ok to feel sad about it.”
Practice self-compassion, and allow yourself to feel sadness. It matters. I know as a mental health professional that infant feeding difficulties can significantly contribute to poor postnatal mental health.
Practice hope:
“I won’t always feel this sad.”
“My body is enough.”
“I tried my very best.”
“I am enough.”
“My baby loves me.”
“I am a good mom, and I feed my baby with love.”
Talk about your experience with safe people
It may help to talk about your experience with a trusted friend, family member, a safe support group, or mental health professional.
It may help to creatively record your experience through art, journaling/blogging, poetry, dance, or music (whatever your jam is). Express your grief, tell your story, in whatever way feels right to you. Maybe you didn’t get the right education, breastfeeding management, or support; maybe you didn’t produce enough milk; maybe you needed to take incompatible medication; or you have a physical disability. There is surely someone who had the same experience. You are not alone.
Read about and listen to other women talk about their experiences. There are so many parents out there who have their own experience of infant feeding guilt, and if you talk about your experience, you will find they will talk about theirs. Making sense of your experience and telling your story plays a major part in your healing. It doesn’t have to be in the form of a book or blog; it might be sharing your experience in a support group or talking with a friend.
Follow social media accounts that provide accurately balanced and unbiased research and support all different types of infant feeding, like the Fed is Best Foundation and the Infant Feeding Alliance. And in the same breath, unfollow anything that makes you feel worse (even if that isn’t their intention).
You may have heard of the Kubler-Ross stages of grief. They can be applied to any experience of grief or loss, but in this instance, we are going to examine infant feeding guilt through the “stages of grief” lens.
Whilst there are five stages, they are not necessarily experienced in order, and different stages can be re-experienced at different times. However, it is commonly believed that you need to work through each stage to move forward in your grief towards healing.
- Denial – This is believed to be a protective mechanism, to prevent someone from becoming overwhelmed from the grief or experience. It may look like relief, or a reluctance to accept there has been any sort of loss. (It is important to note that this only relates to someone experiencing infant feeding guilt, and not those who are happy and confident in choosing formula for their baby). This stage could be extremely brief, or last longer.
- Anger – This is the stage I see lots of women stuck in. They can become furious about breastfeeding and find it very difficult to see other women breastfeeding without feeling rage or anger. Some women describe it as a very visceral and physical sensation in their chest or stomach. In this stage, those experiencing infant feeding guilt may be looking for someone to blame and may lash out at others. This is where feelings of guilt and anger towards oneself may arise, leading onto…
- Bargaining – Mothers may find themselves plagued with uncertainty, wondering “If I had refused the epidural/pain medication/caesarean section, would I be able to breastfeed?” “Is it because I didn’t have immediate skin-to-skin contact?” “Did I not pump enough?” etc.
- Depression or Sadness – This is part of the process, and possibly the stage where a lot of women seek help or support for their well-being. This is not (necessarily) a sign of mental illness, and is a legitimate part of processing the loss you have experienced. You may feel intense sadness, change in appetite, fatigue, and lack of motivation. You may have thoughts you are not a good mother or have let your baby down. None of this is true.
- Acceptance – This is different from being happy with what happened. You may still feel angry that you have been let down by certain people or support services; you may feel guilt around choices you made and how this may have impacted your ability to breastfeed; you may still feel sadness when seeing other women breastfeed; but you have accepted the reality and that nothing can change this now.
This is not a process you can force, but through self-care, reflection, and support, you can move on peacefully.
The timeline for reaching acceptance, and for the grief becoming a more manageable part of your life, differs for everyone and will depend on lots of different factors, each being unique to you. But there are some milestones that seem to make things a little easier:
- Introducing solids — when your baby no longer solely relies on either breastmilk or formula milk, this can provide some emotional release.
- Baby’s 1st birthday — at this point babies no longer need infant formula and can either continue to breastfeed or be introduced to cows’ milk or dairy alternative milks as part of a varied and balanced diet. For some women, no longer preparing formula milk can feel like a big step in their recovery. (Also by this age you are much less likely to often see babies the same age as yours being breastfed, as the number of women breastfeeding at this stage is relatively small.)
Once your baby is fully weaned and so are her baby friends and peers, infant feeding guilt may feel like a more distant memory.
How to know if you need professional help
You may benefit from some additional help and support. Things to look out for are: persistent low mood, feeling unable to cope, struggling to bond with your baby, feeling worthless, feeling as if you would be better off dead, anxiety about lots of things or worrying a lot of the time, guilt, problems sleeping (not related to the baby), changes in appetite, and a lack of energy. Some women also describe a feeling “of just not feeling right” or “not like me.”
Infant feeding guilt does not necessarily cause postnatal depression, but it can significantly contribute to its development or compound poor postnatal mental health.
If you have experienced suicidal thoughts, please talk to someone who can help immediately. I am writing from the UK, and the advice may be different depending on where in the world you are reading this, but if you are in the postpartum period and you are feeling like you are in a mental health crisis and/or are having suicidal thoughts, you can present at your closest Accident and Emergency department, where they will provide you with urgent care and keep you safe, whilst referring you to the specialist perinatal mental health team for ongoing support and care.
Triggers
Revisit the above suggestions when feeling triggered for comfort and support.
Over time, grief becomes easier and less overwhelming, but it may always be there and may be triggered by certain things such as World Breastfeeding Week, friends having babies, another pregnancy, seeing images of breastfeeding, your child’s milestones and birthdays, and then, of course, the dreaded phrase “breast is best.”
You may find that even after you feel you have put it to bed, something comes and knocks you off your feet again. This is the nature of grief. In the same way that Mother’s Day may be hard for someone who has suffered a loss, various events could trigger low mood, depression and anxiety for those who have suffered from breastfeeding difficulties.
Imagine your brain is your office table, and it is full of papers and books. The papers are your past experiences, and you have spent time either in reflection or therapy, or talking with friends processing your experience of breastfeeding difficulties, and now the papers are stacked neatly in piles. But then someone opens the window or switches on a ceiling fan, and the papers all fly up into the air again. It’s an inconvenience and is frustrating, but you need to spend time sorting the piles out again. Chances are, you are quicker this time as it isn’t quite the mess it started out as, and you have done it once before, so you tidy it up again and carry on. Having another baby, and facing infant feeding again, could feel like an earthquake has hit the room, and it is in a total mess and complete chaos. But with help, and time, you will make sense of your experience and sort it all out again.
If you feel this, speak to your GP; they may discuss medication, counselling, and other specialist perinatal services. There are also lots of specialist counsellors, like myself, working with postnatal mental health. There is no shame in a struggle. You are a good Mum.
Much love & solidarity x

Sarah Edge is a Counsellor Psychotherapist working both online and face to face at the Bump and Baby Hideout in Manchester. Sarah specialises in postpartum mental health, with a particular interest in supporting women in their emotional recovery from breastfeeding difficulties and infant feeding guilt and trauma.
You can find out more about what Sarah offers below.
The Maternal Mental Health Manual is an online guide, designed to support mental health during pregnancy and in the postnatal period. It can be read by either the mother herself or her friends and family, giving everyone a better understanding of the changes in her mental health that may occur during the transition to motherhood. And also very importantly, what to do if you’re worried.
You can find out more about what Sarah offers below.
Instagram: @maternalmentalhealthwellbeing
To find compassionate and judgment-free support, please join our support group. You are not alone. Click> Join us here.
Additional resources and stories:
Sacrificing Your Mental Health Is Not Worth It To Exclusively Breastfeed
Clinicians’ Guide to Supporting Parents with Guilt About Breastfeeding Challenges

These feelings are all normal because of how they got there in the first place-societal ideals based on Public Health ideals, outdated World Health Organization ideals, State and Provincial Perinatal Health ideals . These companies like the Baby Friendly Initiative are paid to put policy in place in Hospitals. You were not there , your friends your Doctor was not there, your lactation consultant or nurse was not there. Big business was there and your hospital/community bought it! You don’t have to buy it ! Your baby does not have to buy it! You can listen to your gut and see what is happening to your baby and yourself. Trust yourself and do what you and your baby needs! That is why we are all here. To support infant feeding, whether breast or formula and cut out the unawareness and ignorance and blatent commercialism of breastfeeding and actually feeding your baby. Be kind to yourself and your baby!