Good information isn’t always enough to overcome bad systems.
By Sarah Christopherson
I wrote this article in late 2018, a few months after giving birth to my daughter. My experience at my “Baby Friendly†hospital was traumatic and it was painful to relive, but I felt like I could help other new parents by telling my story, and it seemed like a good match for the work I was doing professionally to dismantle coercive systems that deprive women of their autonomy.
At the time, I was the policy advocacy director for a national non-profit focused on empowering women as they navigate healthcare in the US. My article was printed in our organizational newsletter in early 2019 and published on our website.
It was shared by Fed Is Best, which also interviewed me. From time to time, I would send the link to expecting parents, not to scare them, but to empower them to stand up for themselves when they sensed that something wasn’t right. It helped me to help others. And telling my story made a difference.
A friend who gave birth in the same hospital texted me, “Your article helped me so much when I was having trouble breastfeeding. I look at the pictures of [my son’s] early days and think about how it would have gotten worse if I hadn’t talked to you and others. I started supplementing with formula early AND I signed that dumb form without blinking. The post-partum period exhausts you so that normal problems you would easily solve seem so much harder… and then you’re dealing with some of the most consequential decisions you’ve ever had to make. It was the things I’d already thought through a bit—like the stuff in your piece—that I was prepared to tackle.â€
Eventually my non-profit changed leadership and I moved into a different policy field. My infant turned into a happy, healthy, precocious, and articulate 6-year-old bouncing ball of energy. And that’s where I thought things ended.
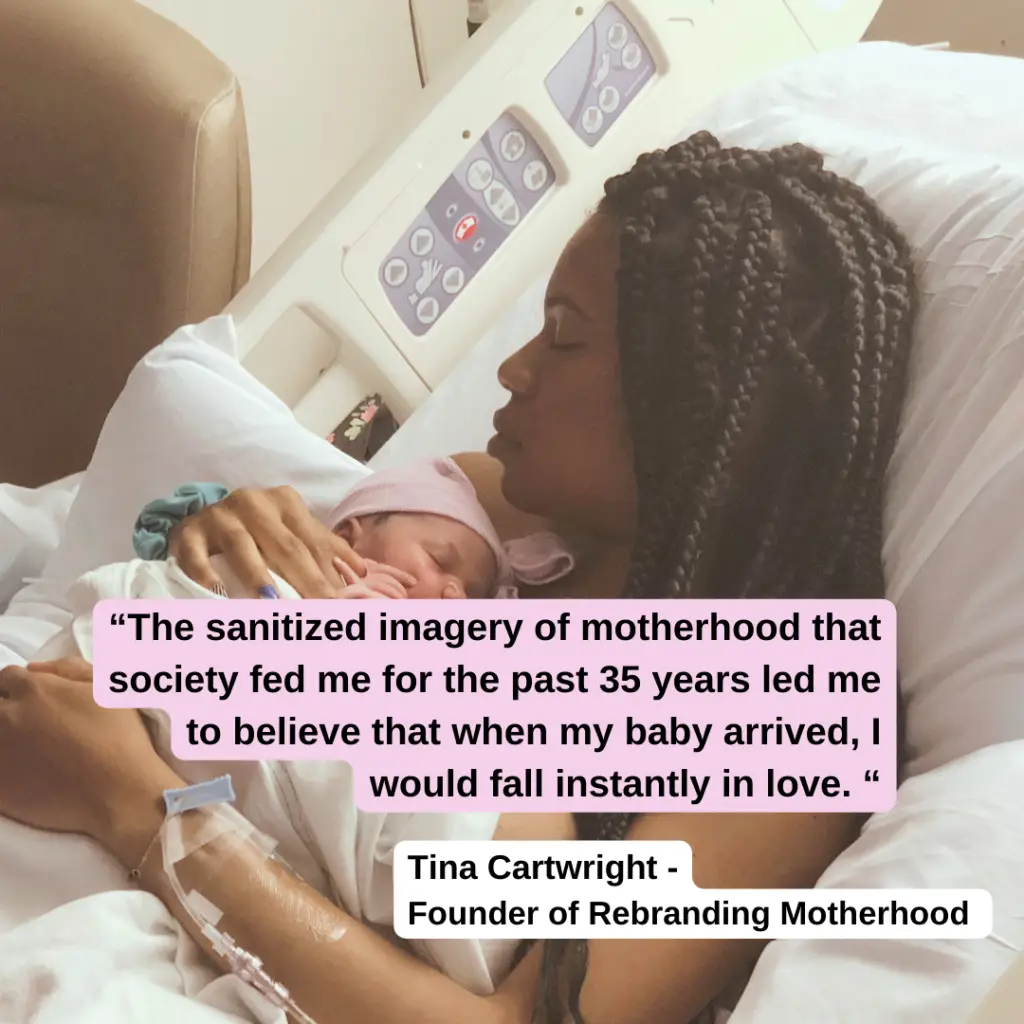
Until last week, when I discovered that without my knowledge or permission, my former organization had rewritten my article in January. They’d kept my name, my story, and the picture my husband took of me in a hospital gown holding my infant daughter on the day she was born. But they’d stripped out paragraph after paragraph that cautioned against breastfeeding coercion. Continue reading