The Fed is Best Clinical Guidelines for Safe Breastfeeding Support in the Newborn Period
the Fed is Best Foundation
October 20, 2018
The mission of the Fed is Best Foundation is to provide safe, evidence-based education and clinical guidelines to prevent complications of insufficient feeding, particularly in exclusively breastfed newborns. At this time, the leading causes of preventable newborn readmissions and extended hospitalizations are due to insufficient feeding from insufficient exclusive breastfeeding, namely hyperbilirubinemia, dehydration, hypoglycemia and hypernatremia. The primary goal of this document is to provide clinician guidelines to ensure safe and adequate feeding for all healthy newborns ≥ 36 weeks gestation while providing breastfeeding education and support in the immediate postnatal period.
1. Teach mothers breastfeeding technique prior to delivery
Mothers can be taught breastfeeding technique, latch, safe positioning through video instruction prior to delivery. Mothers can also be taught manual expression of colostrum and pumping in the event of missed feeds due to mother-baby separation
2. Counsel and review the mother’s Feeding Plan
Evaluate and counsel mother on risk factors for late onset or insufficient breast milk production and plans for supplementation to avoid hospitalization and health risks to her newborn if breast milk is delayed or insufficient. Evaluate and respect the mother’s values and wishes to avoid risks to her newborn’s brain and health. The priority of safe breastfeeding support is avoidance of feeding complications and hospitalization for hyberbilirubinemia, hypernatremia, dehydration and hypoglycemia and newborn safety, not exclusive breastfeeding rates at discharge. Provide judgment-free support for her infant feeding goals.
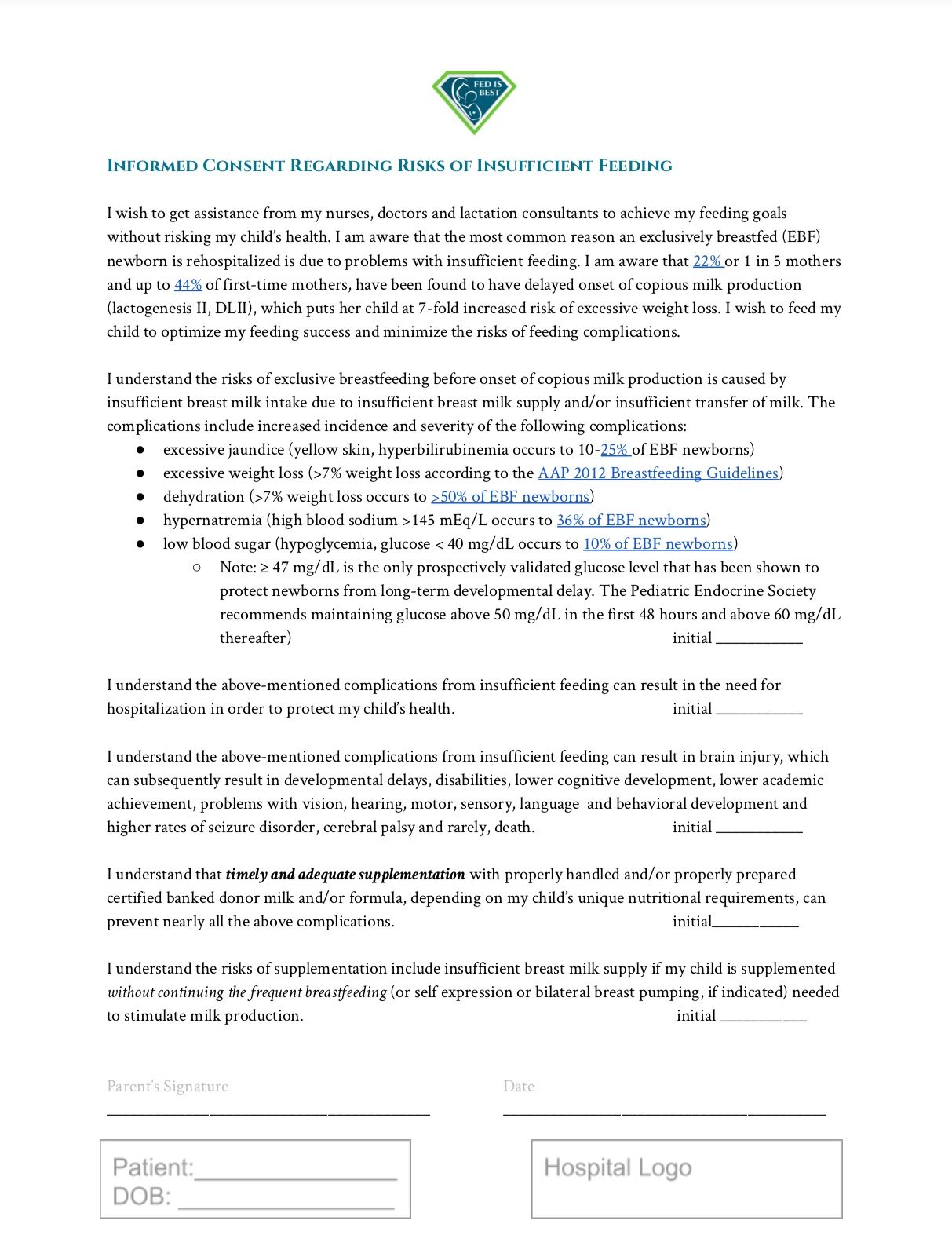
3. Informed consent of risks of insufficient feeding and its clinical signs
Parents have a legal right to information on the risk of brain injury, disability and rare death from insufficient feeding of infants and the clinical signs of excessive jaundice, excessive weight loss, dehydration, hypoglycemia and hypernatremia. Providing patients information on the signs and consequences of insufficient feeding and a plan to prevent these complications with rescue supplementation while maintaining breast milk supply can protect a child from serious and irreversible outcomes. Below is a downloadable and printable informed consent form that can be modified for hospital use.
4. Breastfeed within 1 hour with confirmed transfer of colostrum
Give instruction on breastfeeding technique during the first feeding, namely latch, safe positioning, hearing of swallows within 1 hour of birth if the mother’s and infant’s clinical conditions allow.
5. Universal screening of glucose within 1 hour of birth
Universal screening of glucose within 1 hour of birth and ongoing screening for newborns who are at risk of hypoglycemia per hospital protocol, not receiving ad-lib supplementation or the full daily requirement of 100-120 Cal/kg/day or 5-6 oz/kg/day (breast milk and/or formula).[1] Glucose screening can prevent unsafe levels of hypoglycemia that can impair brain development, which can occur in all newborns, including healthy, term appropriate-for-gestational-age (AGA) newborns.[3] Ten percent of healthy, term, exclusively breastfed (EBF) newborns with good latch undergoing the Baby-Friendly exclusively breastfeeding guidelines have been shown to develop asymptomatic hypoglycemia of < 40 mg/dL when screened to 48 hours of life (23% of first-born EBF newborns developed the same).[2] The deleterious effects of asymptomatic hypoglycemia (< 45 mg/dL) within the first 3 hours of life have been documented and have been associated with lower academic achievement, even when corrected.[3] Furthermore, a population study with over 101,000 healthy non-hyperinsulinemic newborns followed up at ages 2-6 showed that developing hypoglycemia of < 40 mg/dL was associated with higher risk of developmental delay, motor developmental delay and cognitive developmental delay, which were pronounced if diagnosed within 6 hours after birth (relative risks shown below).[4] Late onset starvation-related hypoglycemia found among previously healthy, term AGA breastfed newborns discovered between 3-5 days of life has been shown to result in extensive brain injury resulting in significant long-term disability.[5]

Blank staring is a commonly missed sign of hypoglycemia. This breastfed newborn developed hypoglycemia and lethargy by 9.8% weight loss and had a glucose level of 20 mg/dL shortly after this photograph was taken.
Risks of adverse neurodevelopmental outcomes related to hypoglycemia (< 40 mg/dL)[4]
| Increased Risk of Developmental Delay | |
| Any neurological or neurodevelopmental outcome |
1.48-fold |
| Any developmental delay |
2.53-fold |
| Motor developmental delay |
1.91-fold |
| Cognitive developmental delay |
2.85-fold |
*Only statistically significant risk ratios are listed and have been adjusted for mode of delivery, birth weight for gestational age, gestational age, sex, Apgar score and birth year
Risks of adverse neurodevelopmental outcomes by early (< 6 hours) and late (> 6 hours) neonatal hypoglycemia (< 40 mg/dL)[4]
| Early hypoglycemia < 6 hrs | Late hypoglycemia > 6 hours | |
| Any neurological or neurodevelopmental outcome (one or more disorders) |
1.94-fold |
1.29-fold (NS) |
| Any developmental delay |
3.01-fold |
2.33-fold |
| Motor developmental delay |
2.34-fold (NS) |
1.93-fold (NS) |
| Cognitive developmental delay |
3.17-fold |
2.54-fold |
NS = not significant. Any hypoglycemia of <40 mg/dL was a statistically significant risk factor for motor developmental delay but the effect became less statistically significant when broken down between early and late presentation. All other listed risk ratios are statistically significant and adjusted for mode of delivery, birth weight for gestational age, gestational age, sex, Apgar score and birth year
6. Avoid low blood sugar or hypoglycemia < 50-60 mg/dL by ensuring adequate feeding
The Pediatric Endocrine Society recommends glucose levels no lower than 50 mg/dL in the first 48 hours and no lower than 60 mg/dL thereafter,[6] particularly for high risk newborns, which now include healthy, term appropriate-size-for-gestational-age exclusively breastfed newborns.[2] Glucose levels < 45 mg/dL, even early transitional hypoglycemia, have been associated with permanent declines in long-term academic achievement.[3] If the newborn is at or near the hypoglycemic threshold and lactogenesis II has not occurred or baby is not transferring effectively, supplement to satisfaction. For some newborns this may require 5-6 oz/kg/day of milk (breast milk and/or formula) which provides the full daily requirement of 100-120 kcal/kg/day to restore caloric reserve and stabilize serum glucose. Please refer to the PES guidelines for indications for IV dextrose.[1,6] Avoid hyperglycemia during correction of hypoglycemia as it can worsen neurological outcomes.[7]
7. Every 12 hour weight checks
Healthy, term exclusively breastfed newborns can lose 7-8% of their birth weight in 24 hours.[8] Every 12 hour weight checks during the birth hospitalization captures the newborns at highest risk of complications from excessive weight loss within the first 24 hours and can signal need for supplementation for newborns with > 75%ile weight loss, particularly those showing signs of persistent hunger and distress.
8. Minimum of daily bilirubin checks in Exclusively Breastfed newborns
Exclusive breastfeeding, particularly when breast milk supply or transfer of milk is insufficient, is a major risk factor for severe hyperbilirubinemia according to the AAP Hyperbilirubinemia Guidelines Committee.[9] The first TcB/TsB screening should be done within the first 4-24 hours depending on risk factors as listed in the AAP guidelines. Daily transcutaneous and/or serum bilirubin checks should be obtained in all EBF newborns until the full daily nutritional requirement is met with onset of daily weight gain, including at the outpatient follow-up appointment. Bilirubin levels are expected to increase until the onset of lactogenesis II occurs and exclusive breastfeeding is capable of providing the full requirement of 5-6 oz/kg/day of breast milk and/or formula.[1] Refer to the AAP Hyperbilirubinemia guidelines for in-hospital management of hyperbilirubinemia.[8] For newborns who are approaching the phototherapy threshold, higher volumes of milk intake through supplemented breastfeeding with safe, tested human donor milk or formula (if the mother has less than full breast milk supply of 5-6 oz/kg/day) has been shown to decrease bilirubin levels more effectively than exclusive breastfeeding with phototherapy alone.[10,11]
9. Check sodium levels at Greater than 5-7% weight loss in Exclusively Breastfed newborns
Hypernatremic dehydration is a complication that is solely caused by insufficient feeding of milk to an exclusively or near-exclusively breastfed newborn and can result in multi-organ injury, brain injury, long-term disability and death.[12-14] Check sodium levels at > 5-7% weight loss or in distressed newborns given increased risk of hypernatremia in newborns with > 5% weight loss. Three studies have shown that hypernatremia can develop by weight loss of 5-7%.[15-17] The most recently published study universally screening healthy, term newborns before discharge showed that 30% of newborns overall and 36% of exclusively breastfed and mix-fed babies developed hypernatremia of > 145 mEq/L vs. 6% among exclusively formula-fed newborns.[17] The study found that hypernatremia developed by a weight loss of 4.77% in one high risk newborn (male, delivered to a highly-educated mother by cesarean section), the majority occurring at >5% weight loss. Sodium screening should be considered in newborns with <5% weight loss in newborns with rapid weight loss and signs of distress. If lactogenesis II has not occurred or there is ongoing weight loss, supplement with pumped milk, donor milk or formula to infant satisfaction for sodium levels near 145 meQ/L or between 145-150 mEq/L to prevent further sodium elevation (typically 30-60 mL per feeding). It has been shown that over half of newborns with sodium levels > 150 meQ/L have abnormal developmental scores by 12 months of age.[12] Sodium levels > 150 mEq/L require parenteral management in intensive care setting and should not be corrected faster than 0.5 mEq/L/hr as rapid correction has been associated with increased seizure risk and higher mortality.[18]

Once an underfed newborn develops critical levels of dehydration and/or hypoglycemia, they will commonly stop crying in order to preserve caloric reserve. Dry lips in a quiet, insufficiently fed newborn is a commonly misssed sign of dehydration.
10. Supplement breastfeeding before reaching the hyperbilirubinemia, hypernatremia and hypoglycemia threshold to protect the newborn brain
Ad lib supplementation to satisfaction with safe, laboratory-test human donor milk or properly-prepared formula of newborns developing unsafe bilirubin, sodium and glucose levels from insufficient feeding can prevent extended and repeat hospitalization, prevent brain injury and its neurological sequelae and protect the long-term breastfeeding relationship.[19] Many mothers whose children require hospitalization for feeding complications may associate breastfeeding with harm and may give up breastfeeding altogether. Mothers with insufficient supply whose children are experiencing persistent hunger may be more likely to continue breastfeeding if they know their child is not suffering and is safely fed through combination feeding. Counseling mothers on the importance of safe and sufficient feeding can build their confidence regardless of their breast milk supply, allow for a more sustainable breastfeeding relationship for mothers with low supply and protect infants from feeding complications. The ABM guideline’s recommended volumes for supplementation correlating to the colostrum production volumes of postpartum mothers are unproven to be sufficient to correct metabolic abnormalities consistent with starvation and dehydration when colostrum has proven to be insufficient.[20] Ad lib supplementation to satisfaction in newborns developing abnormal values can allow the newborn to self-correct metabolic abnormalities like hypernatremia and hyperbilirubinemia and can prevent further depletion of caloric and fluid reserve. In cases where oral repletion of nutritional deficiencies is insufficient, parenteral correction should occur in the intensive care setting.
- Supplement before reaching the phototherapy threshold for hyperbilirubinemia according to the AAP hyperbilirubinemia guidelines [9] or bilirubin > 15 mg/dL as developing the diagnosis of hyperbilirubinemia and/or need for phototherapy has been associated with increased risk of brain injury, ADHD, seizure disorder, Bilirubin-Induced Neurological Disorder or Chronic Bilirubin Encephalopathy.[21-24] Serum markers of brain injury (S100b, NSE) have been detected at bilirubin levels as low as 17 mg/dL (20 mg ± 3 mg/dL) and 19 mg/dL.[25,26] Neonatal hyperbilirubinemia > 20 mg/dL has been shown to increase risk of long-term neurobehavioral and cognitive problems in a 30-year follow-up study.[27] Gastrointestinal elimination of bilirubin is the primary way the body reduces bilirubin and ad lib supplementation when breast milk is less than the 5-6 oz/kg/day (0.6-0.75 oz/kg/feed every 3 hours) required to meet the full newborn milk requirement can prevent need for phototherapy and protect the newborn brain from negative neurological sequelae.[1] Exclusively breastfed newborns have hyperbilirubinemia rates of 12-35% and phototherapy rates of about 6%.[28-36] In comparison, breastfed newborns supplemented with a combination of 10 mL/kg of oral dextrose gel and formula to satisfaction have been found to have hyperbilirubinemia rates of 1.3% and phototherapy rates of 0.3%.[37]
- Supplement before reaching the hypernatremia threshold of > 145 mEq/L. Greater than 50% of newborns with sodium levels of >150 meQ/L have abnormal developmental scores by 12 months of age.[12] 95% of hypernatremia >150 can occur by 5-7% weight loss and can even occur below 5% weight loss.[15-17]
- Supplement at the hypoglycemia threshold of < 50 mg/dL (first 48 hours) and < 60 mg/dL (after 48 hours).[4] For newborns near the threshold, breastfeed and recheck in 30 minutes. Supplement if not increasing. If the newborn is showing signs of persistent hunger or hypoglycemia symptoms despite breastfeeding, supplementation should be offered to satisfaction. Continue glucose monitoring if the newborn is exclusively colostrum-fed with marginal glucose levels or recommend ad lib supplemented breastfeeding (breastfeeding then supplementation) until lactogenesis II occurs if glucose levels are not stably above the hypoglycemic threshold. Since hypoglycemic brain injury can ensue within minutes of neuroglycopenia (low brain glucose levels), correction of glucose with supplementation should be based on bedside glucose and should not be delayed for laboratory confirmation.[6] Delays in treatment and insufficient correction can result in serious, irreversible long-term neurological and cognitive impairment of the newborn.
- The newborn stomach is approximately 20 mL at birth and supplementation can be provided 15 mL at a time until satisfied to allow the newborn to self-correct metabolic abnormalities unless lethargic (commonly 30-60 mL per feed if newborn is depleted).[21]
11. Teach health care staff signs of newborn distress from insufficient feeding
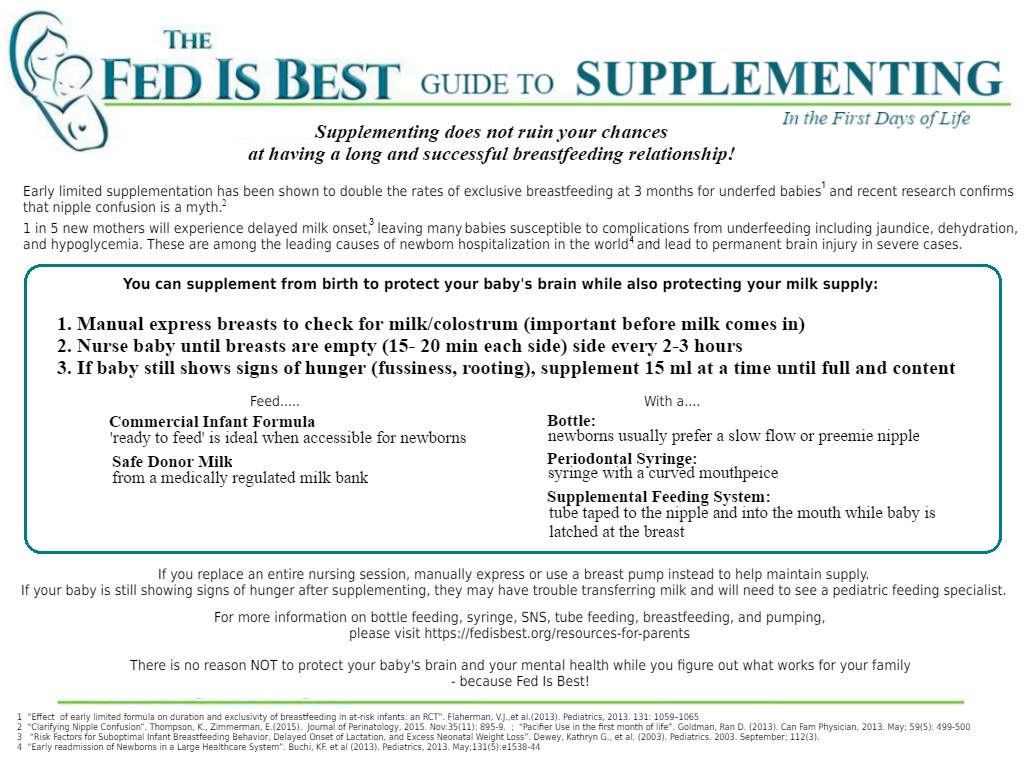
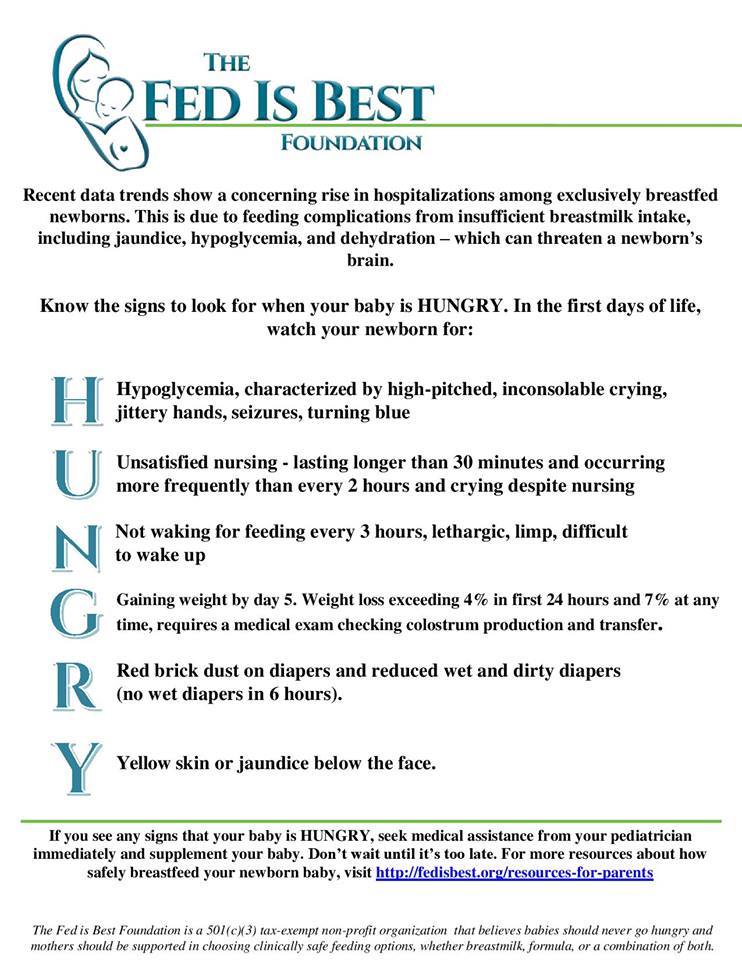
Teach and distribute the HUNGRY infographic for signs of hypoglycemia, hypernatremia, dehydration and jaundice in newborns, which should signal nurse- or doctor-initiated evaluation of glucose, bilirubin, sodium, weight loss percent, breast milk technique, supply and weighted feeds.
12. Teach Parents the signs of newborn distress from insufficient feeding
Teach mothers the signs of newborn distress from insufficient feeding (HUNGRY) and plan for supplementation to prevent excessive weight loss, hyperbilirubinemia, hypoglycemia and hypernatremia after discharge, particularly if lactogenesis II has not occurred. Teach every 12 hour weight check with a home baby scale until the onset of daily weight gain. Before discharge, provide parents the calculated 7% weight loss threshold to avoid at home as greater than 7% weight loss increases the risk of hyperbilirubinemia and hypernatremia. For parents reporting signs of newborn distress at home in the immediate post-discharge period, it is safer to recommend immediate supplementation to protect the newborn brain until urgent medical evaluation is available.
13. Check weight loss percent, glucose, sodium and bilirubin levels in distressed Exclusively Breastfed newborns and before discharge
Exclusively colostrum-fed newborns are known to lose weight in the first days of life due to caloric and fluid intake that is below their full metabolic requirement. The highest risk days for feeding complications are day 2-5 as ongoing weight loss increases the risk of hypoglycemia, hypernatremia and hyperbilirubinemia. Abnormal glucose and sodium levels can occur at different weight loss thresholds depending on the fuel and fluid reserve of the newborn at birth. For exclusively breastfeeding mother-baby dyads for whom lactogenesis II has not occurred and for whom breastfeeding is insufficient to provide the full daily caloric requirement of 5-6 oz/kg/day, it is recommended that ongoing inpatient management be offered if values are approaching the abnormal values of:
-
- Weight loss > 7% (unless a supplementation plan is in place or transfer of milk through breastfeeding is sufficient to prevent further weight loss)[15-17]
- Weight loss > 75%ile at any time according to the Newborn Weight Loss nomogram [42]
- Glucose < 60 mg/dL [6]
- Sodium > 145 mEq/L [15-17]
- Bilirubin in high-intermediate risk zone [9]
Evaluate the breast milk supply and transferred milk volume with weighted feeds. Maternal perception of onset of lactogenesis II and insufficient milk supply has been shown to be accurate and can be proven with breast pumping and/or weighted feeds.[39,40] If lactogenesis II has not occurred and laboratory markers and weight loss are marginal or abnormal, the mother should be counselled on need for supplementation until breast milk can provide the full metabolic requirement as signalled by newborn satisfaction and onset of daily weight gain. The patient should be referred for inpatient management for significant abnormalities. Judicious supplementation while maintaining breast milk supply in cases of marginal breastfeeding sufficiency can prevent avoidable morbidity.
14. Provide ongoing inpatient monitoring or next day follow-up for exclusively breastfed newborns if onset of lactogenesis II has not occurred
Next day follow-up with universal bilirubin, glucose, sodium and weight check should be offered to exclusively breastfed newborns especially if lactogenesis II has not occurred. The immediate post-discharge period is the highest risk time for developing critical feeding complications. Evaluate for signs of newborn distress, lethargy and milk transfer with weighted feeds. Counsel parent(s) on lab values and percent weight loss and offer supportive counseling on breastfeeding technique and supplementation if needed, particularly if exclusive breastfeeding or breast milk supply are insufficient to safely feed the newborn. Emphasize the brain-protective role of supplementation and the importance of protecting the newborn from hunger and thirst to protect newborn health and brain development when breastfeeding is insufficient.
15. Determining the Need for Supplementation
Physicians and nurse practitioners trained in newborn care are the only health professionals trained to interpret laboratory markers of newborn starvation in order to determine the safety of withholding supplementation, particularly among newborns showing signs of persistent hunger. Failure to supplement before an insufficiently fed newborn reaches their individual threshold can result in brain-threatening feeding complications, hospitalization, disability and rarely, death. A parent has the right to choose to supplement without guilt or harassment from health providers. Feeding an infant showing signs of persistent hunger and distress is a protected patient and human right. Timely and sufficient supplementation of a distressed newborn can prevent complications that can result in serious and irreversible harm.
Indications for supplementation otherwise include the following:
- Hypoglycemia < 50 mg/dL in first 48 hours and < 60 mg/dL > 48 hours [6]
- Dehydration / Excessive weight loss > 7% at any time or > 75%ile weight loss at any time per the NEWT weight loss nomogram [42]
- High sodium (sodium > 145 mEq/L)
- Hyperbilirubinemia or abnormal bilirubin approaching 15 mg/dL or high-risk levels on the bilirubin nomogram per AAP Hyperbilirubinemia Guidelines [9]
- Lethargy
- Poor latch and feeding despite correction
- Intolerable pain during feedings despite correction
- Mother – baby separation
- Maternal medications that are unsafe to her baby
- Metabolic abnormalities / congenital abnormalities in newborns that can result in feeding complications
- Physician judgment based on child’s clinical picture
- Mother’s preference
- Insufficient milk production
- Baby’s persistent crying or hunger signs
For a downloadable, printable version of these guidelines, please click on the button below.
To watch the full-length lecture discussing the safe limits of newborn exclusive breastfeeding, please go to http://fedisbest.org/dangers-insufficient-exclusive-breastfeeding-presentation/
The above recommendations are guidelines based on published data of developmental complications from hyperbilirubinemia, dehydration, hypernatremia and hypoglycemia. This does not replace physician evaluation or judgment. Delivery of safe infant feeding requires individualized care and is the responsibility of every health professional involved in the care of mothers and their infants.
References:
- Ben XM. Nutritional management of newborn infants: practical guidelines. World J Gastroenterol. 2008 Oct 28;14(40):6133-9.
- Samayam P, Ranganathan PK, Kotari UD, Balasundaram R. Study of Asymptomatic
Hypoglycemia in Full Term Exclusively Breastfed Neonates in First 48 Hours of
Life. J Clin Diagn Res. 2015 Sep;9(9):SC07-10. - Kaiser JR, Bai S, Gibson N, Holland G, Lin TM, Swearingen CJ, Mehl JK,
ElHassan NO. Association Between Transient Newborn Hypoglycemia and Fourth-Grade
Achievement Test Proficiency: A Population-Based Study. JAMA Pediatr. 2015
Oct;169(10):913-21. - Wickström, R., Skiöld, B., Petersson, G., Stephansson, O. & Altman, M. Moderate neonatal hypoglycemia and adverse neurological development at 2-6 years of age. Eur. J. Epidemiol. 33, 1011–1020 (2018)
- Seske LM, Merhar SL, Haberman BE. Late-Onset Hypoglycemia in Term Newborns With Poor Breastfeeding. Hosp Pediatr. 2015 Sep;5(9):501-4.
- Thornton PS, Stanley CA, De Leon DD, Harris D, Haymond MW, Hussain K,
Levitsky LL, Murad MH, Rozance PJ, Simmons RA, Sperling MA, Weinstein DA, White
NH, Wolfsdorf JI; Pediatric Endocrine Society.. Recommendations from the
Pediatric Endocrine Society for Evaluation and Management of Persistent
Hypoglycemia in Neonates, Infants, and Children. J Pediatr. 2015
Aug;167(2):238-45. - Grelli KN, Gindville MC, Walker CH, Jordan LC. Association of Blood Pressure, Blood Glucose, and Temperature With Neurological Outcome After Childhood Stroke. JAMA Neurol. 2016 Jul 1;73(7):829-35.
- Flaherman VJ, Schaefer EW, Kuzniewicz MW, Li SX, Walsh EM, Paul IM. Early
weight loss nomograms for exclusively breastfed newborns. Pediatrics. 2015
Jan;135(1):e16-23. doi: 10.1542/peds.2014-1532. Epub 2014 Dec 1. - American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation.Pediatrics. 2004 Jul;114(1):297-316. Erratum in: Pediatrics. 2004 Oct;114(4):1138.
- Wickremasinghe AC, Kuzniewicz MW, McCulloch CE, Newman TB. Efficacy of Subthreshold Newborn Phototherapy During the Birth Hospitalization in Preventing Readmission for Phototherapy. JAMA Pediatr. 2018 Apr 1;172(4):378-385. PMC5875379.
- Tan KL. Decreased response to phototherapy for neonatal jaundice in breast-fed infants. Arch Pediatr Adolesc Med. 1998 Dec;152(12):1187-90.
- Koklu E, Gunes T, Ozturk MA, Kose M, Kurtoglu S, Yuksel F. A review of 116 cases of breastfeeding-associated hypernatremia in rural area of central Turkey. J Trop Pediatr. 2007 Oct;53(5):347-50. Epub 2007 May 12.
- Ergenekon, E. et al. Hypernatremic dehydration in the newborn period and long-term follow up. Pediatr Int 49, 19–23 (2007).
- Kaplan, J. A., Siegler, R. W. & Schmunk, G. A. Fatal hypernatremic dehydration in exclusively breast-fed newborn infants due to maternal lactation failure. Am J Forensic Med Pathol 19, 19–22 (1998).
- Uras N, Karadag A, Dogan G, Tonbul A, Tatli MM. Moderate hypernatremic dehydration in newborn infants: retrospective evaluation of 64 cases. J Matern Fetal Neonatal Med. 2007 Jun;20(6):449-52.
- Lavagno C, Camozzi P, Renzi S, Lava SA, Simonetti GD, Bianchetti MG, Milani GP. Breastfeeding-Associated Hypernatremia: A Systematic Review of the Literature. J Hum Lact. 2016 Feb;32(1):67-74.
- Ferrández-González, M. et al. Weight loss thresholds to detect early hypernatremia in newborns. J Pediatr (Rio J) (2018).
- Bolat F, Oflaz MB, Güven AS, Özdemir G, Alaygut D, Doğan MT, Içağasoğlu FD, Cevit Ö, Gültekin A. What is the safe approach for neonatal hypernatremic dehydration? A retrospective study from a neonatal intensive care unit. Pediatr Emerg Care. 2013 Jul;29(7):808-13.
- Flaherman, V. J. et al. Effect of early limited formula on duration and exclusivity of breastfeeding in at-risk infants: an RCT. Pediatrics 131, 1059–1065 (2013).
- Kellams, A., Harrel, C., Omage, S., Gregory, C. & Rosen-Carole, C. ABM Clinical Protocol #3: Supplementary Feedings in the Healthy Term Breastfed Neonate, Revised 2017. Breastfeed Med 12, 188–198 (2017).
- Bhutani VK, Johnson-Hamerman L. The clinical syndrome of bilirubin-induced
neurologic dysfunction. Semin Fetal Neonatal Med. 2015 Feb;20(1):6-13. doi:
10.1016/j.siny.2014.12.008. Epub 2015 Jan 7. - Wei, C.-C., Chang, C.-H., Lin, C.-L., Chang, S.-N., Li, T.-C., and Kao, C.-H. (2015). Neonatal jaundice and increased risk of attention-deficit hyperactivity disorder: a population-based cohort study. J Child Psychol Psychiatry 56, 460–467.
- Maimburg, R.D., Olsen, J., and Sun, Y. (2016). Neonatal hyperbilirubinemia and the risk of febrile seizures and childhood epilepsy. Epilepsy Research 124, 67–72.
- Gourley, G.R. (2002). Breast-feeding, neonatal jaundice and kernicterus. Semin Neonatol 7, 135–141.
- Sarici D, Gunes T, Yazici C, Akin MA, Korkmaz L, Memur S, Kurtoglu S, Ozturk
MA, Sarici SU. Investigation on malondialdehyde, S100B, and advanced oxidation
protein product levels in significant hyperbilirubinemia and the effect of
intensive phototherapy on these parameters. Pediatr Neonatol. 2015
Apr;56(2):95-100. - Okumus N, Turkyilmaz C, Onal EE, Atalay Y, Serdaroglu A, Elbeg S, Koc E, Deda G, Cansu A, Gunduz B. Tau and S100B proteins as biochemical markers of bilirubin-induced neurotoxicity in term neonates. Pediatr Neurol. 2008 Oct;39(4):245-52.
- Hokkanen, L., Launes, J., and Michelsson, K. (2014). Adult neurobehavioral outcome of hyperbilirubinemia in full term neonates—a 30 year prospective follow-up study. PeerJ 2, e294.
- Chang, R.-J. et al. Weight loss percentage prediction of subsequent neonatal hyperbilirubinemia in exclusively breastfed neonates. Pediatr Neonatol 53, 41–44 (2012).
- Chen, C.-F. et al. Influence of breast-feeding on weight loss, jaundice, and waste elimination in neonates. Pediatr Neonatol 52, 85–92 (2011).
- Yang, W.-C. et al. Bodyweight loss in predicting neonatal hyperbilirubinemia 72 hours after birth in term newborn infants. BMC Pediatr 13, 145 (2013)
- Han, S. et al. A Model for Predicting Significant Hyperbilirubinemia in Neonates From China. Pediatrics 136, e896-905 (2015)
- Chen, Y.-J., Chen, W.-C. & Chen, C.-M. Risk factors for hyperbilirubinemia in breastfed term neonates. Eur. J. Pediatr. 171, 167–171 (2012).
- Huang MS, Lin MC, Chen HH, Chien KL, Chen CH. Risk factor analysis for late-onset neonatal hyperbilirubinemia in Taiwanese infants. Pediat Neonatol. 2009 Dec;50(6):261-5.
- Huang A, Tai BC, Wong LY, Lee J, Yong EL. Differential risk for early breastfeeding jaundice in a multi-ethnic Asian cohort. Ann Acad Med Singapore. 2009 Mar;38(3):217-24.
- Weight loss and hypernatremia in breast-fed babies: frequency in neonates with non-hemolytic jaundice.Tarcan A, et al. J Paediatr Child Health. 2005 Sep-Oct
- Kuzniewicz et al. Association Between Laboratory Calibrationof a Serum Bilirubin Assay, Neonatal Bilirubin Levels, and Phototherapy Use. JAMA Pediatrics.JAMA Pediatr. 2016;170(6):557-56
- Zaitsu, M., Yoshihara, T., Nakai, H. & Kubota, S. Optimal Thermal Control with Sufficient Nutrition May Reduce the Incidence of Neonatal Jaundice by Preventing Body-Weight Loss Among Non-Low Birth Weight Infants Not Admitted to Neonatal Intensive Care Unit. Neonatology 114, 348–354 (2018).
- Bergman NJ. Neonatal stomach volume and physiology suggest feeding at 1-h
intervals. Acta Paediatr. 2013 Aug;102(8):773-7. doi: 10.1111/apa.12291. Epub
2013 Jun 3. Review. -
Chapman, D. J. & Pérez-Escamilla, R. Maternal perception of the onset of lactation is a valid, public health indicator of lactogenesis stage II. J. Nutr. 130, 2972–2980 (2000).
- Humenick, S. S., Hill, P. D., Thompson, J. & Hart, A. M. Breast-milk sodium as a predictor of breastfeeding patterns. Can J Nurs Res 30, 67–81 (1998).
- Wickström, R., Skiöld, B., Petersson, G., Stephansson, O. & Altman, M. Moderate neonatal hypoglycemia and adverse neurological development at 2-6 years of age. Eur. J. Epidemiol. 33, 1011–1020 (2018).
- https://www.newbornweight.org/