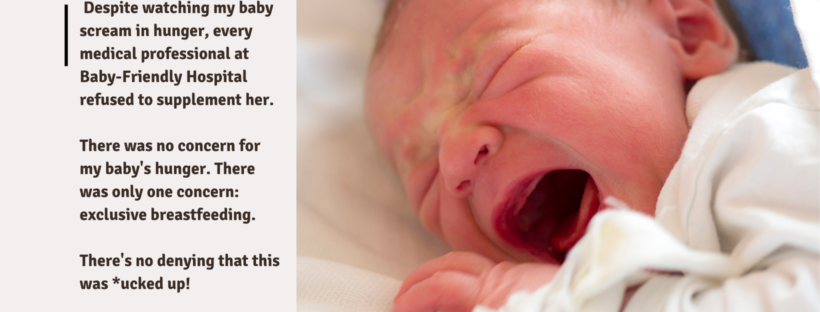
I am sharing my story because I know new parents are struggling with lactivism right now; they need to hear my story to protect themselves. It was lactivism that compromised my mental health, and it was lactivism that caused my child to suffer.
I thought lactivist rhetoric existed only on social media, but I was wrong. It’s also part of our medical institutions and is harming moms and babies.
When I was pregnant, I wasn’t sure how I wanted to feed my baby, so I planned to try breastfeeding and switch to formula if it didn’t work. After her birth, my daughter had a difficult time breastfeeding. My nurse told me that babies are born to breastfeed, so I should keep trying until she does. I stayed up all night with her trying to breastfeed, but she just
wouldn’t for more than a few minutes and would fall back asleep. Continue reading