About two days after initial discharge from her Indiana birth hospital, my three-day-old baby was admitted to the Children’s Hospital with dehydration and high sodium levels (hypernatremia). My purpose in sharing the following exceptionally personal detail is that these words might prevent similar suffering for others.
Several separate oversights in care culminated in my baby’s health crisis. If only she had been supplemented earlier, she might not have faced hypernatremia and dehydration.
After reading and attending classes, I knew how wonderful breastfeeding can be for babies and mothers. I chose my labor and delivery hospital because I was excited about its Baby-Friendly designation. With my master’s degree, I believe in research-based practices so the skin-to-skin sounded so good for the baby and me. It was! She seemed to cry less when held, and holding the sweetheart was cathartic. Fortunately, the baby latched well right after birth thanks to the help of some extraordinarily skilled labor and delivery nurses.
My attempts at breastfeeding by myself did not go well; I did not think the baby was latching well even with the nipple shield so I asked to see the lactation consultant (IBCLC) a few hours after birth. Even though the IBCLC confirmed my baby had a poor latch and believed I might have inverted nipples, I was not encouraged to pump and check for colostrum milk or supplement. She did instruct me to dry pump before each feeding to draw out my nipples to encourage a better latch.
At one day old, my baby was already showing hunger cues immediately after a feeding session. https://www.instagram.com/p/BJ05R-2Be1I/
When my baby was about 30 hours old, breastfeeding was still not going well and she cried often so I asked the IBCLC to return even though the only time she could come was during quiet hours. Since the baby had fed often the previous evening, the IBCLC thought the baby had been “cluster feeding.” Since the baby’s latch was still poor, I was concerned about how much milk the baby was ingesting, and I could not express any milk at any time without extreme effort and pain. 
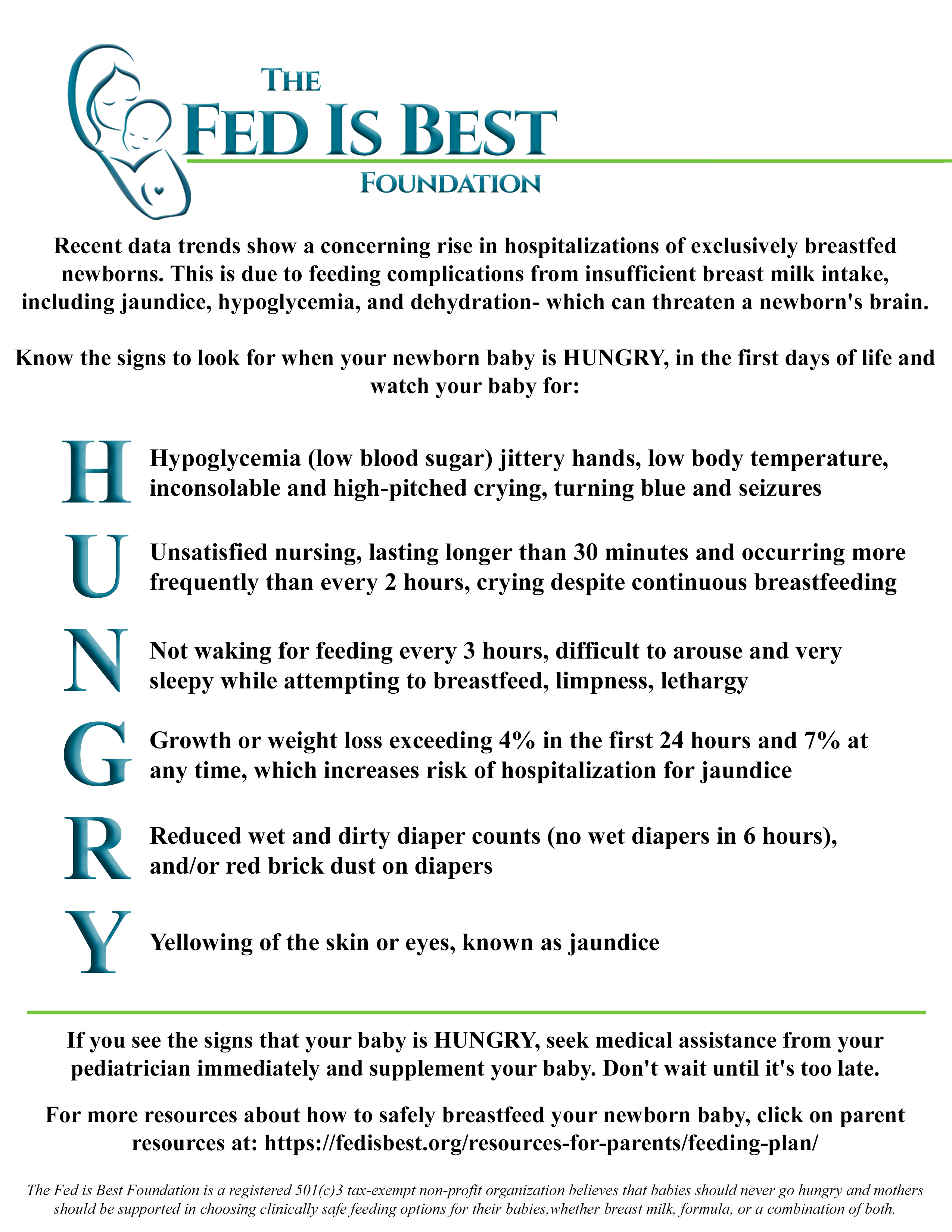
During my stay I started to notice redness in the baby’s diaper, when I mentioned that I was concerned about the redness that was often in the baby’s diaper, the first nurse said it was probably blood from vaginal discharge. This is where I wish I could go back in time and show the nurse one of the diapers from the trash just to be certain, but I told myself at the time that, if the nurse needed to see a diaper, she would have asked to see it. My baby seemed to have that red-pink color in her diaper almost every time I changed her diaper before we were discharged.
When we were leaving the birth hospital at just over 36 hours, I couldn’t shake this bad feeling about the redness in the baby’s diaper. I asked another nurse about it twice, but she did not respond to those specific diaper questions, and so I felt awkward having asked what I assumed must have been stupid questions. In reflection, I realize there are no stupid questions concerning a baby’s welfare.
Unfortunately it wasn’t until my baby was three days old and readmitted into the Children’s Hospital that a nurse mentioned the redness might be concentrated urine, commonly known as “brick dust” and not vaginal discharge. Sadly, I learned that even when she was only one day old, the baby was probably already suffering from lack of fluids.
My baby was born Wednesday morning, and we were discharged Thursday evening. On Friday, I was at home by myself on a holiday weekend beside myself because I thought something was seriously wrong with the baby. My baby had been feeding continuously or would cry nonstop. She rarely unlatched without howling. I was lucky to get 5 minutes without her on my breast every few hours to relieve myself. I knew newborns were difficult, but I thought, “It should not be this difficult; something is wrong,” but I told myself the baby would bounce back and assumed that I was over-reacting as an anxious new mother.
At three-days-old, my baby stopped howling and became sleepy. She was weak when awake, often had a gazed-over look in her eyes, and could stare often into space without making eye contact; this was different behavior from the baby who was alert and engaged throughout her first day of life. She urinated only once and did not have a bowel movement, but the “red brick dust” was still appearing in her diaper. When I phoned the hospital, the on-call pediatrician asked me to bring her to the ER.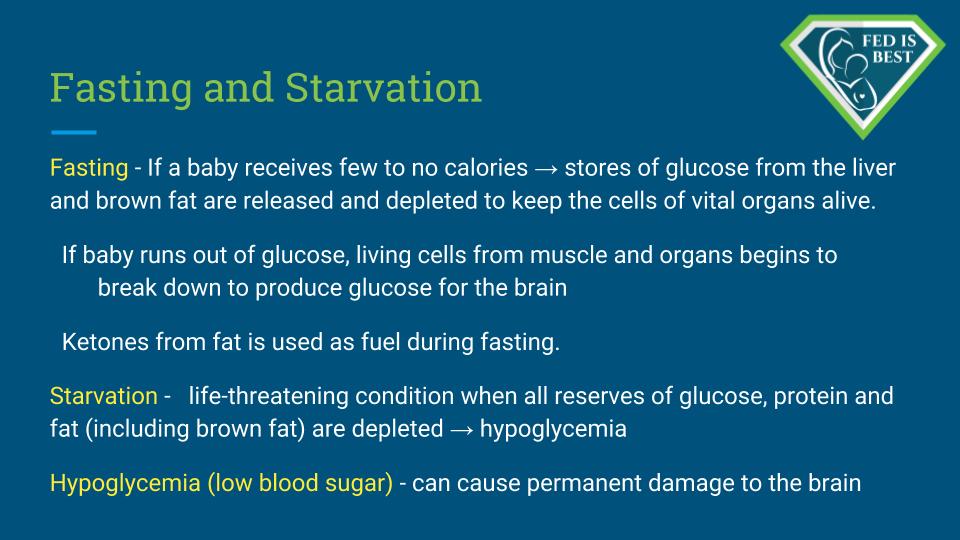
The Children’s Hospital pediatrician seemed frustrated that we were discharged 36 hours after birth; he believed babies need at least 48 hours at the hospital after birth. He was concerned about her weight loss. With trepidation, I asked him if the baby was going to be brain-damaged; he said he thought we had made it to the Children’s Hospital in time.
At the Children’s Hospital, the nurses and I recorded her feeding amounts and inspected and weighed her diapers for output; this is the level of attention I would have liked for her at her birth hospital. I also began supplementing my pumped breastmilk with formula. The first several attempts, I only pumped about 2-5 mL, but gradually my production increased over days to less than an ounce. The baby gradually gained more strength and alertness until she was discharged from the Children’s Hospital when she was five days old.
Despite my medication designed to improve milk production, I still was not producing enough, and it seems I had blocked ducts. My nipples were fiery from a yeast-infection, sore, cracked, bruised, bleeding, and painful; the baby had a yeast infection in her mouth and diaper area. I never noticed a milk letdown, but strangely, I couldn’t seem to stay dry; it seemed I leaked constantly. I smelled sour milk and realized the smell was coming from me. I was exhausted and later diagnosed with post-partum depression and anxiety.
After such a traumatic experience, I also recognized that I needed both sleep to heal and medication to stop crying; I knew that a healthy mama is better able to care and advocate for her daughter.
I knew breastfeeding would be challenging, but I did not expect my daughter to suffer hypernatremia and dehydration. If I could go back in time, what would I change? I would ask the nurses for more hands-on newborn care , so I could have a chance to rest, recover, and advocate for my daughter. I would say, “Please check the baby’s diapers,” and would have asked them to do weighted feeds. I would have had someone experienced in newborn care with me advocating for me and the baby during most hours we were in the hospital and at home.
When the baby seemed hungry directly after a feeding, I would have supplemented. I wish I had known how quickly newborn dehydration can begin and how serious it can become.
I wish I had felt that it is okay to follow your concern for a new baby, obtain second opinions, and pose seemingly “stupid” questions even if you have or think you have a postpartum mood disorder. Now that the mental fog of sleep deprivation and post-partum depression and anxiety has departed, it’s easy for me to recognize that I could have asked for more help, but I remember how weak and confused I felt at the time; I was doing the best I could.
Although this was a traumatic experience, what positives can I glean? Despite the scary first few days after birth, my baby is here laughing and playing today because some people acted on the idea of “better safe than sorry.” My baby did not fall through all cracks.
Thank you, Fed Is Best, for working towards preventative measures that will make sure every baby safe and no mother is sorry!
The Fed Is Best Foundation has a free, downloadable safe breastfeeding protocol available for every family. http://fedisbest.org/resources-for-parents/
http://fedisbest.org/resources-for-parents/feeding-plan/
To donate to our foundation to continue developing education resources to safely feed your babies: http://fedisbest.org/donate/

Do you want to join The Fed Is Best Team? Please send a message to: contact@fedisbest.org We can’t wait to meet you!


It really depends on the hospital. The area i live in has a baby friendly hospital and they are absolutely wonderful. I had both my children there. The nurses are really attentive. They call lactation several times a day to check on u amd baby. Lactation always comes and checks and makes sure baby is latched well amd eating. They weighed and checked diapers to make sure baby is doing well. Now the other hospital in my area that is not baby friendly is really horrible. My adopted daughter went in for induction the night before valentines the nurses rarely checked on her. She told them she felt pressure they said she was fine they had just checked her she wasnt having the baby for awhile and left her alone again. My daughter had my grandson at 4am unassisted by a doctor or nurse. She had called them at 3:30 and said she felt alot of pressure they didnt even bother to come in the room. So it really does depend on the hospital and the staff they have working for them.