Written by: Jody Segrave-Daly, MS, RN, IBCLC
Cluster feeding is a phrase that is used to describe infant feeding behavior(s). Generally, it’s breastfeeding or bottle feeding that is in a different pattern from your baby’s typical feeding pattern. It is described as breastfeeding sessions or bottle-feeding sessions that are much shorter and more frequent, for 3-4 hours of the day. It often happens during a baby’s fussy period of the day. The Academy Of Breastfeeding Medicine defines cluster feeding as “several short feedings close together.” However, new mothers are being told constant and prolonged feeding around the clock in the hospital is “cluster feeding,” and this is where confusion that can result in harm begins. There is a point when cluster feeding becomes a clear sign of insufficient breast milk and/or insufficient transfer of milk, and those signs must be taken seriously for the health and safety of the infant. Mothers tell us they receive conflicting information and as a result, they become very frustrated, lose confidence and want to stop breastfeeding. Or, they persist with exclusive breastfeeding due to incorrect advice, and negative outcomes occur.
Cluster feeding is also a phrase that sometimes is also called “comfort-feeding.” As parents, we react to infant cries and feeding cues, so naturally, we will assume a baby is hungry and when we feed them, they will be satisfied. But some babies will snack and will not take a full feeding during their cluster-feeding time; this is normal. Some babies simply want to suckle on a pacifier after nursing or bottle feeding. This is because their bellies are full, but they want to suckle for soothing and not for feeding of milk. Some breastfeeding babies will suckle, using non-nutritive sucking patterns for soothing only. Some babies will also want to be held and snuggled or may want to be carried or want movement while suckling too!
Cluster feeding can also happen during growth spurts as well, but babies generally take in more milk during this time. It can also happen during times when a baby is not feeling well, teething or is tired or cranky. And it’s true—some babies don’t cluster feed at all. My exclusively breastfed babies never did and preferred sucking on a pacifier, after nursing for comfort.
When is cluster feeding considered normal?
- It happens after a mother’s full milk supply is in, after birth.
- It is during a limited time period of 3-4 hours in 24 hours.
- The breastfeeding mother has adequate milk supply.
- Baby is having plenty of dirty and wet diapers.
- The baby is gaining enough weight.
If you are concerned that you are not making enough breast milk, or your baby isn’t transferring enough milk, you can do a simple check to see if you are.
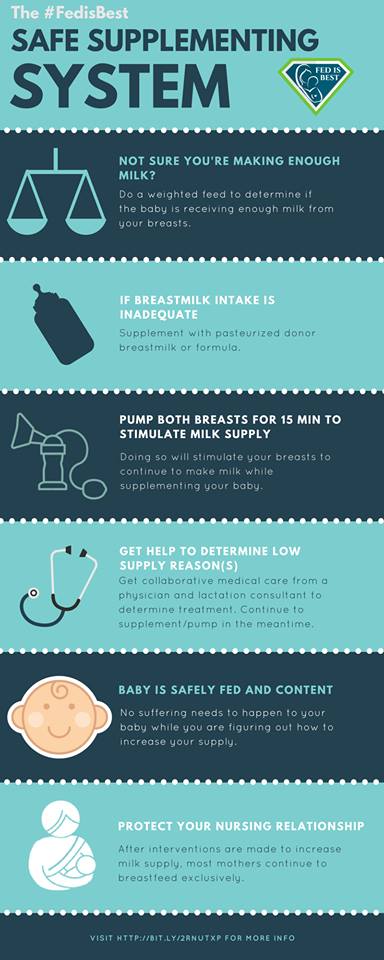
If your milk supply is low and/or your baby isn’t transferring enough breast milk, you can get immediate help to determine why your supply is low. This is very important information to know so that timely milk supplementation can occur to protect your baby from underfeeding. It’s also important so that you won’t miss an opportunity to increase your milk supply.
Do babies “cluster feed” before the onset of copious milk production during the first few days of life?
No. Breastfeeding babies nurse frequently, every 2-3 hours which is normal but different from “cluster feeding.” Bottle-feeding babies do not cluster feed during this time either.
When is frequent breastfeeding not normal?
- A baby who is breastfeeding non-stop, despite having a perfect latch and swallowing confirmed before the onset of copious milk production in the hospital.
- A baby who cries unless they are breastfeeding and continues to exhibiting hunger cues.
- A baby who is jaundiced, becomes lethargic, or has tremors after long periods of non-stop nursing, or at ANY time.
- A baby who has a 4 percent weight loss at 24 hours of life, or a 7 percent weight loss at any time.
- A mother who can’t self express or pump any colostrum.
- A test weight after nursing on both breasts, for at least 15 minutes each, that reveals inadequate colostrum intake.
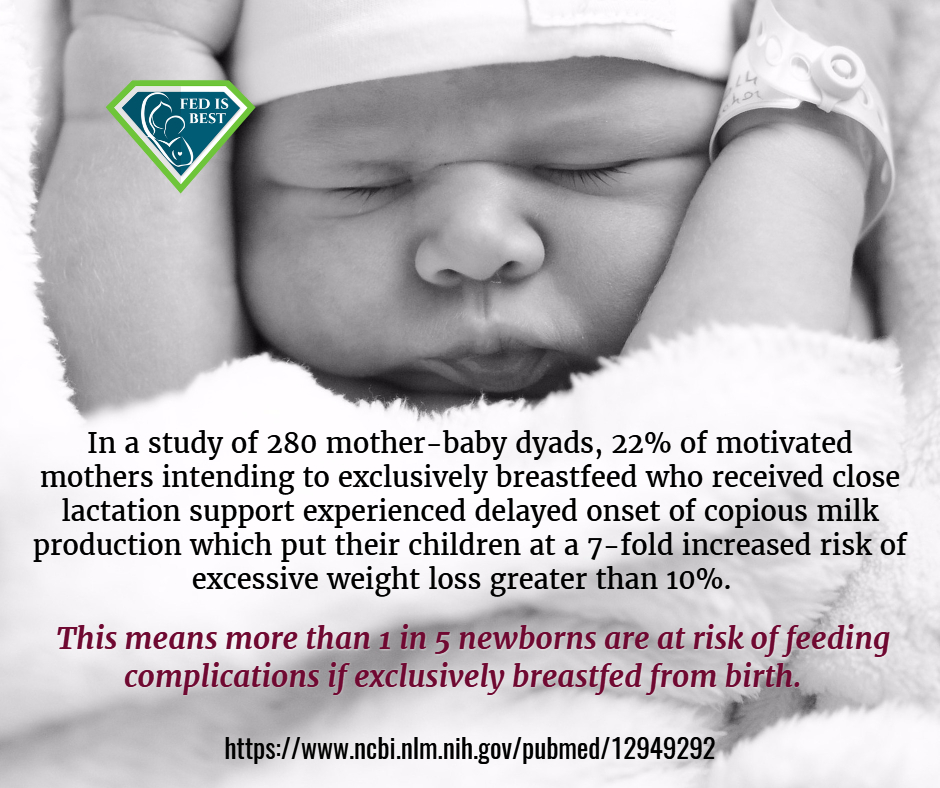
- A mother who is at risk for delayed onset of copious milk production requires special considerations for timely supplementation.
Babies who are nursing constantly or babies who nurse and are not satisfied and cry when removed from breast, require an immediate exam by the pediatrician and a full assessment by the mother-baby RN to be sure they are receiving enough colostrum. Babies who are sleepy or lethargic and not nursing or bottle feeding, require an exam and assessment as well.

Delayed onset of copious milk production is common and happens to one in five mothers. Therefore, it is important for babies to have timely supplementation, to prevent exclusive breastfeeding complications from inadequate colostrum intake.
When your baby requires supplementation, donor milk from a milk bank or formula can be used. Supplementing will protect your baby from complications while waiting for your milk to come in.
A recent study showed underfed babies who were supplemented with limited amounts of formula after breastfeeding nearly doubled their breastfeeding rates at 3 months.
For stories of mothers who supplemented their breast-feeding babies and went on to breast-feed click here.
For stories of mothers who regret not supplementing their breastfeeding babies and who suffered complications click here.
To learn more about our safe infant feeding guidelines we have a FREE downloadable feeding plan for every family to use.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and every thing in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going. Thank you for your advocacy!
