When the Fed Is Best Foundation launched two years ago, a few nurses sent us messages about their experiences working in a BFHI hospital. Some of the nurses felt comfortable speaking out because they left their jobs or retired early, as they did not want to be part of the restrictive breastfeeding policies that were implemented. They shared common concerns of watching exclusively breastfed babies being refused supplementation, while babies were crying out in hunger from not enough colostrum which resulted in NICU admissions.
Two years later, we now receive messages from nurses, physicians, LC’s and other health professionals, regularly. They express their concerns while asking for help and for patient resources. They tell us their stories and they need support and direction of what to do about unethical and dangerous practices they are forced to practice. We collected their stories and are beginning a blog series of health professionals who are now speaking out about the Baby-Friendly Health Initiative and the WHO Ten Steps of Breastfeeding.
Heather, NICU and nursery nurse at a level 3 NICU
I see babies crying from being starved and dehydrated at work frequently and we aren’t even Baby-Friendly. Our management is looking to become Baby-Friendly and I’m very concerned it will get worse. Because we push breastfeeding so much even our pre-term infants in the NICU end up suffering from longer hospital stays because we refuse to feed them with the appropriate bottles due to worries about nipple confusion.
It’s extremely disturbing how strong the shaming is. When I delivered my own babies, I was in the hospital where I work postpartum and needed to supplement. I felt so guilty supplementing them, even though they absolutely needed it. I am one of the mothers who experienced delayed onset of milk supply but went on to exclusively breastfeed both of my babies.
Jenny, Mother-Baby Nurse in a small community based non-Baby-Friendly hospital with a Level 1 NICU.
According to my manager, we will not apply for the certification because of the cost. We, however, do have very similar breastfeeding protocols in place. The vast majority of our staff has completed the 15-hour training “10 Steps to Successful Breastfeeding” by the World Health Organization.
Our breastfed babies tend to be somewhat quiet and sleepy during the first 24 hours of life. After that, they ‘wake up’ and realize they are hungry. We see babies either at the breast or crying for more. We tell mothers that ‘cluster feeding’ is normal newborn behavior. (It’s not–they are crying out in hunger.) Hungry babies sound angry and sad at the same time. Mothers are exhausted and upset. They try and try to breastfeed constantly worrying about their milk supply or whether their baby is getting anything at the breast.
Not very many mothers ask about supplementation. When they do, we are supposed to tell them the few drops of colostrum they are producing is enough for most babies. When the staff feels that a baby needs to be supplemented medically, most moms decline supplementation because they have been educated on the dangers of using formula. We are currently seeing more mothers willing to supplement since we are now also offering donated breast milk for very limited medical reasons.
“Informed” Consent Forms
HEATHER
We probably have half of the breastfeeding babies in the nursery at some point during the night because they are crying and the moms are exhausted, medicated, have bloody cracked nipples and need to sleep just an hour or two. We try hard not to supplement the babies who are crying because we know our charts are being audited and if we supplement too much, we are identified and called out. We will sneak pacifiers to help soothe babies who are screaming and sometimes we will use sweet ease (sugar solution used to console babies during procedures) to help the ones who are inconsolable. Some moms just do not have enough colostrum and these babies are paying the price.

Research tells us that 1 in 5 mothers have delayed onset of full milk production, so we simply cannot ignore the abnormal behavior of a non-stop crying baby, knowing there will be babies who need to be supplemented.
I have been in situations where I feel forced to lie about how much I supplement babies so I don’t get in trouble, but these babies are very clearly starving and need to eat more than 10 ml. We can’t deny food and fluids for our adult patients so why are we forced to with newborns?
Mothers are required to sign a consent form to supplement their babies, even when they require supplementation to prevent jaundice, hypoglycemia or dehydration. The consents have very misleading information often making the mothers feel very guilty for using formula. Ironically, mothers are not taught the risks of exclusive breastfeeding, namely inadequate milk transfer or supply.
Jenny
A risk consent form is listed as a part of our feeding intervention, however, our manager will not allow a consent form to be used. We do have to document that the parent was educated on risks of formula use. However, parents are not taught the risks of exclusive breastfeeding.
Our lactation department developed a feeding plan for babies being supplemented. The amounts are the same regardless if the baby is a 35 week 4-pound twin or a 41 week 10-pound baby. Our supplementing feeding plan is 2-10ml per feeding during the first 24h of life. The amount increases to 5-15ml during 24-48 hour of life, and 15-30 ml during 48-72h. We do not need a doctor’s order to supplement with formula but do need one for the donor milk. When parents request pacifiers we are supposed to discourage their use.
Nurses, in general, are frustrated over the strict feeding guidelines and their inability to help the hungry babies and their exhausted mothers. Nurses see the babies getting more jaundiced, struggle chasing the blood glucose of our large and small for gestational age babies, early babies or babies of diabetic mothers. Even when there is a true medical need for supplementation some babies even end up with an IV since some parents feel it is better than a little bit of formula. Early babies typically become tired after attempting to breastfeed and end up with a feeding tube to prevent using a bottle.
Nurses also disagree with the lactation staff on what is considered an adequate feeding. Lactation staff often feels there is no need to follow the feeding plan if the baby has spent any amount of time at the breast. And if a mother pumps, for example, a drop or two of colostrum, the LC staff ‘mixes’ that with some glucose water and calls it a feeding. We do see at times our babies becoming hypoglycemic, and some are readmitted for jaundice. Our late preterm babies typically end up staying with us for a while for ‘feeding issues’.
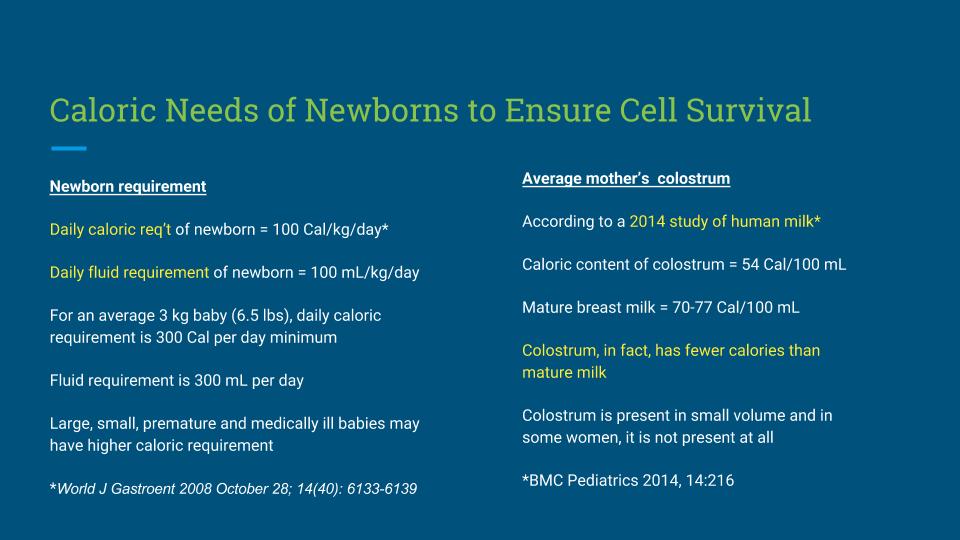
A newborn baby requires calories and fluids to prevent starvation complications. Drops of colostrum are not enough to sustain a baby.
In our hospital, I feel formula feeding mothers are supported by nursing staff and they are educated on how to properly prepare and feed formula. The unit itself only has pro-breastfeeding posters on display.
Breastfeeding “Support”
Heather
In the NICU, we have babies who could go home weeks earlier using regular flow bottles but we must use the slowest flow nipples to promote breastfeeding. The babies get tired and collapse the nipple and can’t finish the feeds in 30 minutes, so they end up with an NG tube again.
We have been told that some exclusively breastfed babies must be withdrawing from medications because of how irritable they are, but really, they are crying from hunger and are starving.
Our lactation consultants only work on day shift and will only see a baby after 24 hours. If a mom has flat nipples and we can’t get the baby to latch, they are left to attempt to breastfeed for 24 hours before they get help, because we are not allowed to give them nipple shields.
Jenny
What I personally feel the most frustrating are our medical providers. They see our babies suffering from hunger at times, but seem very hesitant to step on the LC staff’s toes. Even with our smallest and youngest babies’ (or even our feeder-grower transfers), nutritional needs tend to be managed by LC staff and not the medical provider.
I’m at times also very worried about the mental health of some of my mothers. We are supposed to send these exhausted, anxious new mothers home following strict crazy feeding plans (triple feedings with SNS, finger feeding, etc) when these poor parents have not even learned how to provide basic baby care independently. Our nursery is only for sick babies. If parents need a break, the staff can offer to bring the babies to the nurse’s station. Before doing so, the staff is supposed to ‘offer support to encourage rooming-in’.
“We discharge babies home knowing they are at risk for complications all the time.”
Heather
About 30 percent of our exclusively breastfed babies are discharged with a weight loss of 7 percent and about 50 percent are discharged at a 10 percent weight loss. We discharge babies home knowing they are at risk for complications all of the time. The only babies who are protected are the babies who are formula fed, combo fed or whose mothers have enough colostrum.
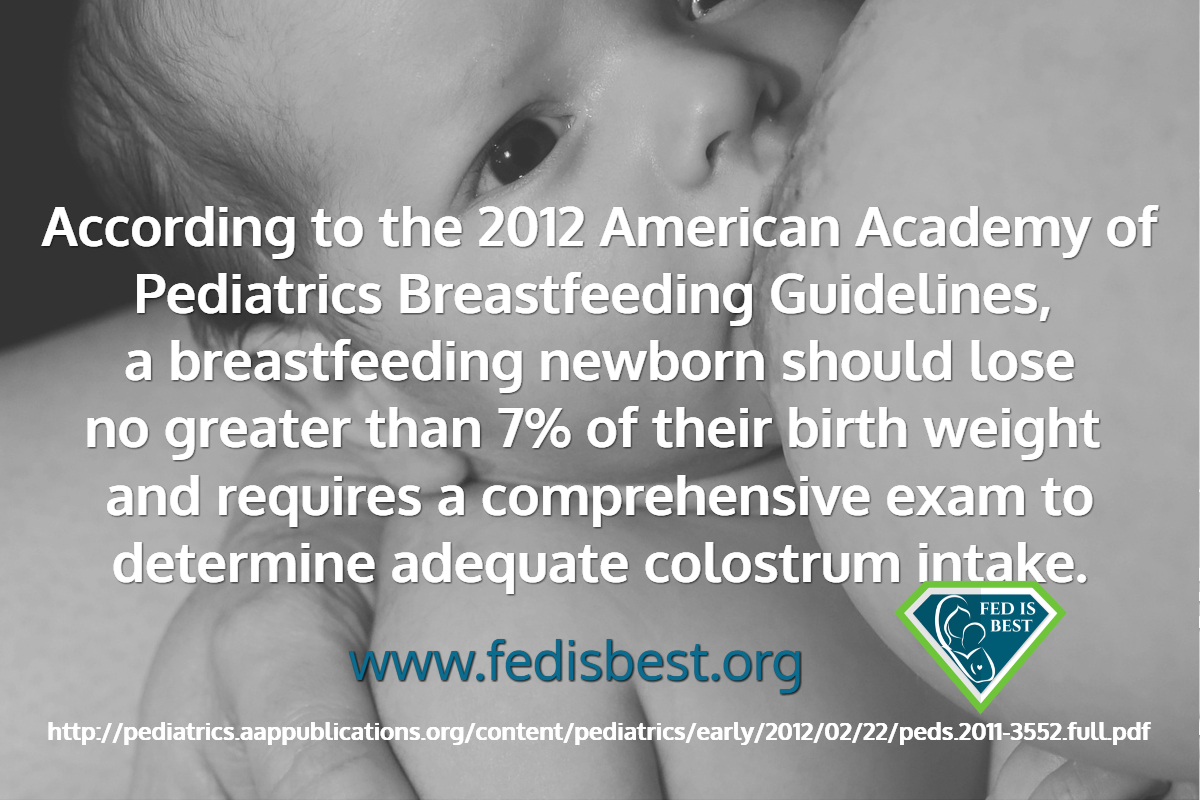
The Baby-Friendly Hospital Initiative’s policy to hide these common and dangerous complications of early exclusive breastfeeding hospitalizes thousands of babies a year in the U.S. alone, and millions more in the rest of the world, complications that can result in a long-term developmental disability that cannot be reversed once the child reaches a critical threshold.
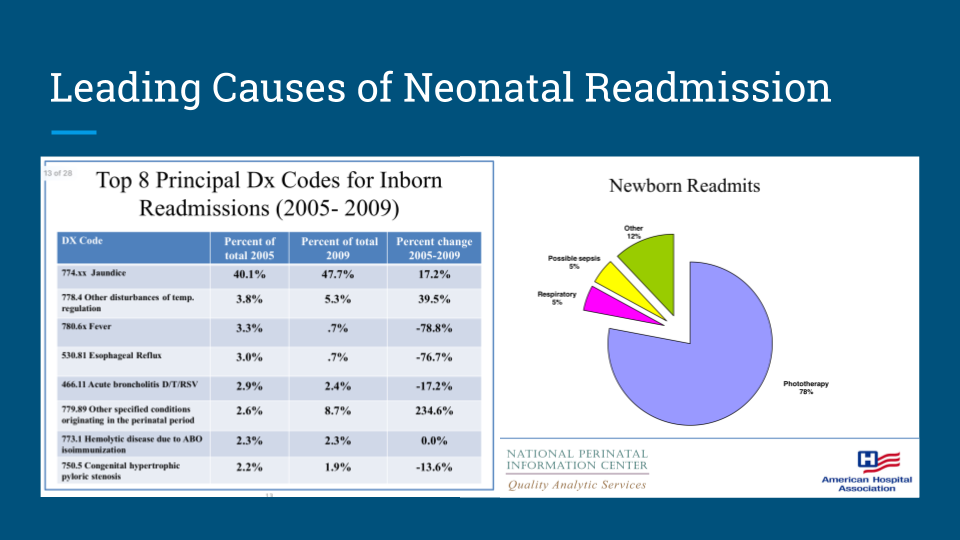
Data from the American Hospital Association showing the leading cause of neonatal readmissions were for jaundice and that among all neonatal readmitted patients, 78% received phototherapy.
We have a private Face book group for licensed health professionals who are interested in learning more about our advocacy. Please contact us at contact@fedisbest.org
References:
If I Had Given Him Just One Bottle, He Would Still Be Alive.
Breast Is Best Failed Me And My Starving Son
From A Pediatric Nurse Practitioner-You Are Not Alone
The Second Night Syndrome is Abnormal and This is Why
I See Myself In Other Mother’s Eyes: A Neonatalogist’s Fed Is Best Story
My Baby Had Been Slowly Starving-The Guidelines For Exclusive Breastfeeding Are Wrong
Feeding Your Baby—When Supplementing Saves Breastfeeding and Lives
The Scientific Evidence on the Effects of Underfeeding on the Newborn Brain
The Medical Professionals At The University Of North Carolina Allowed My Baby To Starve
The Newborn Stomach Size Myth: It is NOT 5-7 mL
Why I’m Angry With My Baby Friendly Hospital in Texas
My Baby Starved at Kaiser Permanente – I Was Told Her Stomach Size Was Only 5 mL
Why Was No One Listening To Me Or My Baby At Our Baby-Friendly Hospital? The Signs Were There.
Q&A: One Nurse’s View on Strict Breastfeeding Policies
“Is Baby-Friendly Safe?”: BFHI Safety Issues Discussed at National Neonatology Conference
Just One Bottle Would Have Prevented My Baby’s Permanent Brain Damage From Hypoglycemia
My Son Became Severely Jaundiced and Dehydrated in a Baby-Friendly Park Slope, Brooklyn Hospital
My Baby Was Starving – She Lost 17 Percent Of Her Body Weight While Exclusively Breastfeeding
I May Never Forgive The Hospital For Starving My Baby While Under Their Care!
When A Mother Says She Isn’t Making Enough Colostrum, Believe Her The First Time
I Supplemented My Starving Baby When My Hospital IBCLC’s, Doctor and WIC Counselor Told Me Not To
I Was Ashamed to Ask for Formula in the Hospital, But I Couldn’t Hear Her Scream Anymore
“I had no idea that it wasn’t normal for a newborn to nurse for hours at a time”
Why Was No One Listening To Me Or My Baby At Our Baby-Friendly Hospital? The Signs Were There.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and every thing in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going. Thank you for your advocacy!


6 thoughts on “Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative”