Ella D.
I am a neonatal intensive care unit (NICU) nurse and the hospital where I work delivers more than 2,000 babies annually, over half from high-risk pregnancies. In our part of the country, “natural parenting” is widely embraced, and it is difficult to find a hospital that isn’t “Baby-Friendly.” Our hospital administration views the Baby-Friendly Hospital Initiative (BFHI) designation as a marketing tool, hoping new parents will choose our hospital to deliver their babies. Any criticism of the BFHI risks a backlash.
COMPLICATIONS on the mother-baby unit
Since our hospital became BFHI certified, NICU admissions for acute starvation while exclusively breastfeeding have escalated to at least 4 admissions weekly. (It should be zero.) Fortunately, once the baby reaches the doors of the NICU, we are free from the BFHI protocol. We are not, however, free from all the indoctrination the parents have already received, and they’ve received an impressive and dangerous amount. We require verbal consent and a physician’s order for donor milk use, but only low birth weight babies qualify for that. We also require a physician’s or Neonatal Nurse Practitioner’s (NNP) order for formula milk use. It is not uncommon for parents to request IV fluids over formula supplementation.
The Baby Friendly Hospital Initiative and the 10 steps to successful breastfeeding are now under critical review for newborn complication.Their unacceptable consequences are serious and irreversible and absolutely preventable.
admissions to the nicu
The second day of life is the most common time for NICU admissions. Complications from inadequate colostrum intake include hypoglycemia, dehydration, hyperbilirubinemia and hypernatremia, which are all very serious. Hypoglycemia is the number one reason for NICU admission from our mother-baby unit. We have a very large maternal-fetal medicine presence at our hospital, with the majority of our mothers qualifying as high risk. These mothers are not prepared in their antenatal breastfeeding education class about having multiple risk factors for low or delayed milk production. Unfortunately, they learn it when it is too late, and their babies need emergency supplementation and other invasive interventions due to hypoglycemia. The discussions that then ensue take place while the mother is dealing with her previously “normal” infant’s now low blood sugar and her new feelings of inadequacy. What results is a form of postpartum depression and anxiety that potentially could have been avoided with proper prenatal teaching about the need and importance of temporary nutritional supplementation.
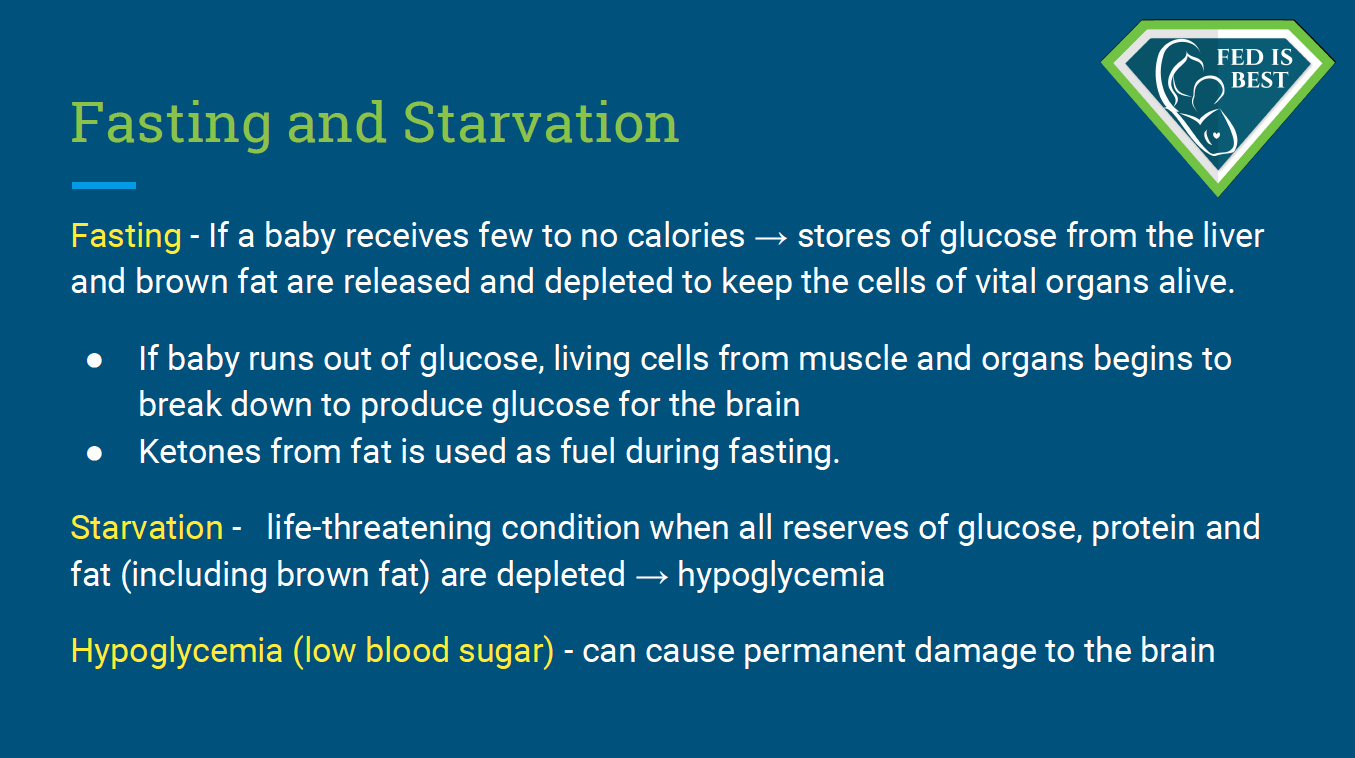
Babies are dependent on their reserves until the onset of copious milk production. However, some babies do not have enough reserves and this can result in acute starvation-related complications. These complications can result in irreversible impairments in brain development. The term “starvation” is being used according to the medical definition explained above.
Our mother-baby unit recently implemented glucose gel to treat hypoglycemia without utilizing formula for stabilization of blood sugars. Most babies still end up in NICU despite giving the glucose gel. It is not nearly as effective as formula milk. Many mothers will still refuse the glucose gel and opt for an IV and NICU admission to avoid feeding their baby formula milk. They also won’t allow us to provide a pacifier for sucking and comfort from the pain while we insert the IV catheter because they were taught pacifiers cause ‘nipple-confusion’and will ruin their breastfeeding relationship. In this part of the country a large percentage of mothers are anti-formula; they typically believe that any amount of formula that is fed to their baby means they have failed at “exclusive breastfeeding.”
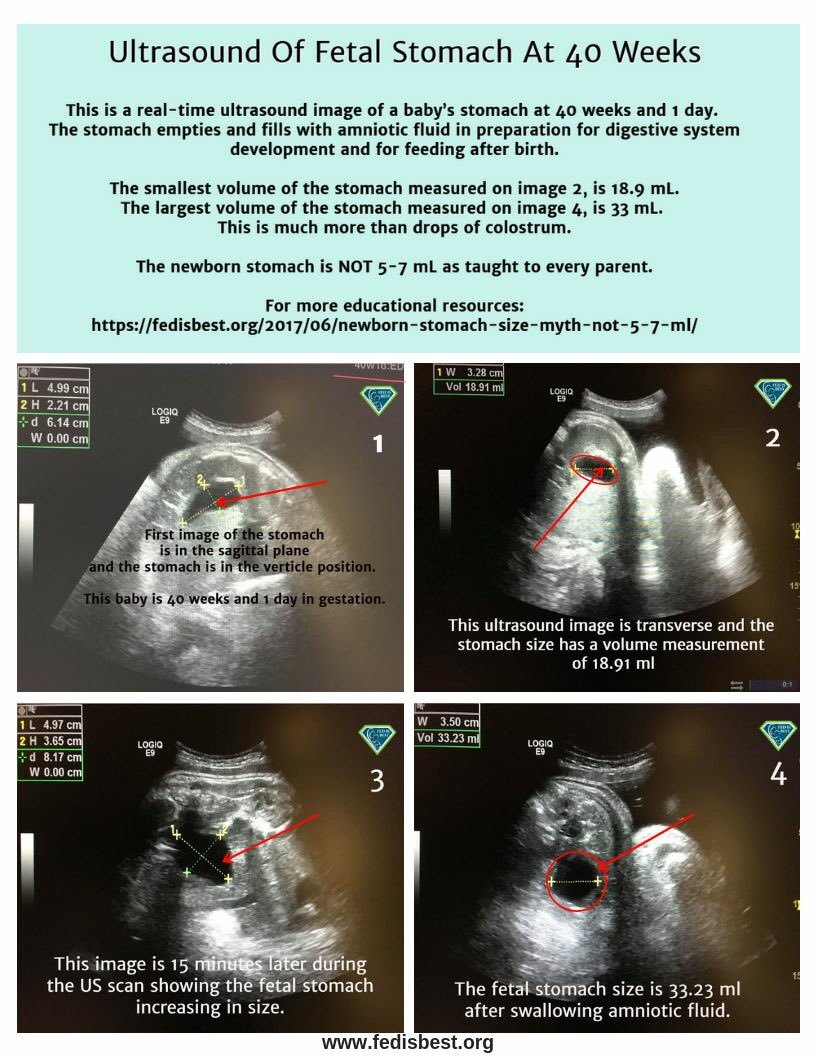
For the mothers who allow formula, they are in disbelief when told their babies are suffering from acute starvation because they have been told the newborn stomach is the size of a marble and that babies are satisfied by merely a few drops of colostrum. Watching their baby guzzle down an ounce of formula is a big reality check, and it dispels the newborn stomach size myth.
It’s very hard to think about what a central glucose of 12 or a bilirubin level that reached exchange transfusion levels does to a baby’s brain after they are discharged. My guess is that we have had many serious complications that result from the BFHI protocol, and I know for certain the teachings promote dangerous behaviors at home. There is one readmission that haunts me. A baby suffocated under his mother’s breast when she fell asleep in bed, ‘cluster-feeding’ after he was discharged home. He survived but had severe encephalopathy and was virtually unresponsive despite resuscitation and cooling. I know of many exclusively breastfed babies that experienced failure to thrive who did not gain weight until their pediatrician finally convinced the parents to introduce formula. I have even had coworkers that have been in denial as their own babies slide off the growth curve. BFHI blindly promotes exclusive breastfeeding without considering individual mother and baby’s unique needs, which should be a safely fed baby and a mentally and physically stable mother.
Allowing infants to develop insufficient feeding complications by not disclosing the preventable risks for the purpose of meeting the BFHI hospital metrics that requires 80 percent of babies to exclusively breastfeed, is a dangerous and unethical evolution of modern-day breastfeeding promotion, and constitutes negligence on the part of those who have supported and carried out the initiative.
admission to nicu AFter discharge from the hospital
It is not uncommon for an exclusively breastfed baby to be readmitted to our NICU after discharge from the hospital after seeing their pediatrician for their follow-up appointment. The most common complications are hyperbilirubinemia secondary to inadequate nutrition and hydration. When they are discharged from our NICU, babies have proven weight gain and/or a feeding supplementation plan in place to prevent complications again. They will also have an appointment with their pediatrician for 1-2 days from discharge.
Research has shown that among healthy term newborns who are discharged from the hospital, exclusively breastfed newborns are twice as likely to be readmitted to the hospital, most commonly for jaundice and dehydration. They are also more likely to require more follow-up visits with their pediatricians for concerns related to feeding and adequate weight gain. (Flaherman et al., 2018)
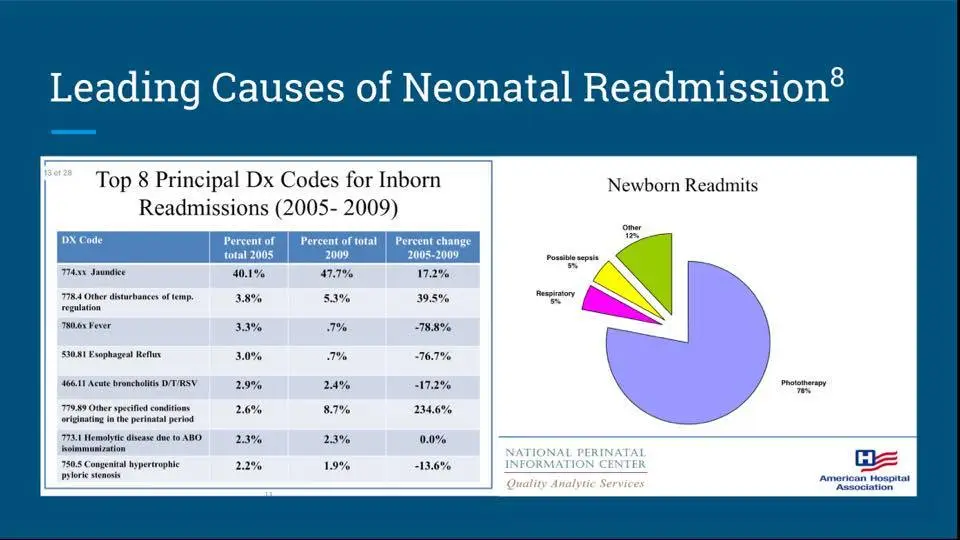
Data from the American Hospital Association showing that the percent of infants readmitted for dehydration-related jaundice increased from 40% of readmissions in 2005 to 48% in 2009. Given that hemolytic jaundice did not increase, staying at 2.3%, only dehydration-related jaundice has increased.
As a NICU nurse, I believe exclusive breastfeeding complications could be easily prevented by the way we prepare and educate women for breastfeeding during their pregnancy. Instead of making exclusive breastfeeding the number one goal during the newborn period, we must make feeding, hydration, and minimizing weight loss below 10% the priority. Women should not be given the impression that IVs, which are terribly painful and come with the risk of infection, are preferable to supplementing their babies with perfectly safe and temporary nutrition. They should be taught to feed and hydrate their babies to prevent hyperbilirubinemia. If they have gestational diabetes, they should know their baby will likely need supplementation. We can praise the benefits of small quantities of colostrum and remind women that those benefits still exist when formula supplementation is necessary to keep their babies safe until their milk comes in. In fact, research shows that it does! We also need to rethink the myth of nipple confusion and use a bottle to supplement babies.
— Ella D.
We have a private and secure Face book group for licensed health professionals who are interested in learning more about and joining our advocacy. Please contact us on Facebook or at contact@fedisbest.org

http://fedisbest.org/2018/11/neonatal-nurse-practitioner-speaks-out-about-the-dangerous-and-deadly-practices-of-the-bfhi/
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
Additional blog stories
If I Had Given Him Just One Bottle, He Would Still Be Alive.
Breast Is Best Failed Me And My Starving Son
From A Pediatric Nurse Practitioner-You Are Not Alone
The Second Night Syndrome is Abnormal and This is Why
I See Myself In Other Mother’s Eyes: A Neonatalogist’s Fed Is Best Story
My Baby Had Been Slowly Starving-The Guidelines For Exclusive Breastfeeding Are Wrong
Feeding Your Baby—When Supplementing Saves Breastfeeding and Lives
The Scientific Evidence on the Effects of Underfeeding on the Newborn Brain
The Medical Professionals At The University Of North Carolina Allowed My Baby To Starve
The Newborn Stomach Size Myth: It is NOT 5-7 mL
Why I’m Angry With My Baby Friendly Hospital in Texas
My Baby Starved at Kaiser Permanente – I Was Told Her Stomach Size Was Only 5 mL
Why Was No One Listening To Me Or My Baby At Our Baby-Friendly Hospital? The Signs Were There.
Q&A: One Nurse’s View on Strict Breastfeeding Policies
“Is Baby-Friendly Safe?”: BFHI Safety Issues Discussed at National Neonatology Conference
Just One Bottle Would Have Prevented My Baby’s Permanent Brain Damage From Hypoglycemia
My Son Became Severely Jaundiced and Dehydrated in a Baby-Friendly Park Slope, Brooklyn Hospital
My Baby Was Starving – She Lost 17 Percent Of Her Body Weight While Exclusively Breastfeeding
I May Never Forgive The Hospital For Starving My Baby While Under Their Care!
When A Mother Says She Isn’t Making Enough Colostrum, Believe Her The First Time
I Supplemented My Starving Baby When My Hospital IBCLC’s, Doctor and WIC Counselor Told Me Not To
I Was Ashamed to Ask for Formula in the Hospital, But I Couldn’t Hear Her Scream Anymore
“I had no idea that it wasn’t normal for a newborn to nurse for hours at a time”
Why Was No One Listening To Me Or My Baby At Our Baby-Friendly Hospital? The Signs Were There.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and every thing in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going. Thank you for your advocacy!
Thank you!

2 thoughts on “NICU Nurse Discloses Newborn Admission Rates From Breastfeeding Complications in BFHI Unit”