FREQUENTLY ASKED QUESTIONS
Written and Edited by Jody Segrave-Daly, RN, IBCLC, Lynnette Hafken, MA, IBCLC, and Christie del Castillo-Hegyi, MD
Our goal is to respond to the many statements that have been made about the Fed is Best Foundation and to answer questions we receive about what the Foundation stands for. Unfortunately, our #FedIsBest phrase has been used incorrectly by others, and it’s important that we clarify what it means and doesn’t mean. Our mission statement has evolved over time and reflects what our parents tell us they need to support them. Click here and here for FAQs part 1 and 2, respectively.
7. Do you believe exclusive breastfeeding is a good goal to promote?
We do if a mother wants to exclusively breastfeed and they are fully informed about their individualized risk factors for delayed onset and or potential low milk supply. We promote and educate families about safe exclusive breastfeeding because no other health organization informs parents about the risks of insufficient feeding complications and how easy they are to prevent. To be fully informed, parents must be educated about both the benefits and risks of exclusive breastfeeding. Currently, they are only taught about the benefits and not the risks.
Many mothers want to exclusively breastfeed, and day after day in our support group we help mothers achieve this goal by developing an actionable breastfeeding plan that works for their unique needs. Mothers, especially first-time mothers, have told us that they gave up breastfeeding in the days after birth because they felt that they were not making enough milk, when in fact, their milk arrival was simply delayed.
If these mothers were educated about their risk factors for delayed onset of milk or insufficient milk supply, how to safely supplement while waiting for their milk to come in, how to increase their milk production, or how to sustain a combo-feeding relationship if their supply is limited, they could go on to have a sustainable breastfeeding relationship instead of losing confidence and stopping breastfeeding altogether.
Our actionable breastfeeding plan provides guidelines for protecting the mother’s milk supply if temporary supplementation is necessary. It’s not true that supplementing decreases the milk supply if a mother’s breasts are adequately stimulated and emptied while supplementing breastfeeding.
Responsible breastfeeding education requires families to be taught when to offer safe supplementation of expressed breastmilk or properly prepared formula to protect their baby’s health in the case of insufficient breast milk supply or intake. In some instances, the need for supplementation cannot wait for the consultation with a pediatrician or lactation consultant as doing so may result in serious harm. Many mothers have told us they panicked when they needed to purchase formula and they didn’t know how to safely prepare it or how much to give.
While we do support safe exclusive breastfeeding, we also recognize that some mothers find that it is not working for them or their babies. In those cases, we believe it is important to provide a mother with all of her feeding options, as opposed to encouraging only continued exclusive breastfeeding. Mothers tell us they do not feel heard when there is a clear agenda to support only exclusive breastfeeding. We will support her in her choice, whether that is exclusive breastfeeding, exclusive formula feeding, or a combination. If she states that continued exclusive breastfeeding is important to her, then it is important to us also. We support her feeding goal while prioritizing her infant’s health and safety by recommending supplementation with milk bank donor milk or formula if needed before unsafe conditions occur.
As health care professionals, it is our ethical duty to provide families with all of their options, and exclusive breastfeeding is no exception. We believe the exclusive breastfeeding metric needs immediate reform in light of the current data regarding harm and lack of data showing efficacy. The practice guidelines also need to reflect the need to respects maternal choice. A new alternative to the Baby-Friendly policy is the new Family-Friendly Protocol at Rush Foundation Hospital, whose philosophy is to improve patient outcomes by respecting parental choice to breastfeed, combo-feed or formula feed while providing all the education and support needed to achieve individual feeding goals.
8. If you believe exclusive breastfeeding is an important goal, why are you not promoting it as the ideal or best?
We believe a fully fed baby is the ideal, and for the mothers who are not making enough milk, supplementation with banked donor milk or formula is ideal and best infant feeding. An infant who is exclusively breastfed and is not safely or sufficiently fed is never ideal or best.
When we started our first Facebook page it was titled “Breast is best, if you have enough breast milk.” Mothers started messaging us with their own heartbreaking stories and we’ve taken to heart the thousands of letters we have received from mothers describing the pressure they felt to achieve the “ideal” of exclusive breastfeeding from birth to 6 months, and the fear they have that formula will hurt their babies’ health and future potential. They describe suffering from unbearable shame and guilt when it was not possible for biological, economic, psychological, and/or other personal reasons. Parents told us they desperately needed to hear a more inclusive infant feeding message. The suggestion to change our phraseology from “Breast is best if you have enough breastmilk” to “Fed Is Best” was heard, and this is how #FedIsBest was born. It was the right thing to do.
As the Foundation has grown, we quickly learned that mothers are under the impression that low or delayed milk supply is rare. This puts mothers in a position where they feel they have failed or that they are somehow biologically “abnormal” when they were not producing enough milk, even when they have followed the advice of their lactation professionals. They also feel alone because of how breastfeeding education downplays the prevalence of insufficient milk.
Sadly, mothers have told us they knew their babies were hungry but were taught that feeding their babies formula milk is very harmful when the true harm comes from not feeding their baby enough! Isn’t the first rule in lactation support “feed the baby”? It’s not “push the baby to the limits of his tolerance to avoid a few milliliters of donor milk or formula.”
Parents have unknowingly harmed their infants under the guidance of their lactation educators and health professionals. Some of these mothers lose trust in breastfeeding altogether, which is not what any of us want.
Every lactation consultant knows that if a baby is not getting enough to eat, temporary donor milk or formula supplementation can help breastfeeding, not harm it. Mothers have the right to know and should be empowered with a supplementation plan in case they need it. To do otherwise is to hide the truth and while making mothers dependent on expert help that they may not have access to in the time required to prevent harm.
Having a Plan B does not destroy mothers’ confidence in their bodies; it gives them the confidence to know they can care for their babies no matter what happens, and it gives them the knowledge they need to support their milk supply until the breastfeeding problem can be addressed.
9. Cluster feeding is a well-known phenomenon. Why would you say it’s a sign of the baby not eating enough? The LLL describes the “second-night syndrome” as normal, why do you say it’s not?
Cluster feeding can be normal when it lasts for a few hours once a day and the baby becomes satisfied after several short feedings. The Academy Of Breastfeeding Medicine defines cluster feeding as “several short feedings close together.” However, mothers are being told constant and prolonged feeding around the clock is “cluster feeding,” and this is where confusion that can result in harm begins. There is a point when cluster feeding becomes a clear sign of insufficient breast milk and/or insufficient transfer of milk, and those signs must be taken seriously for the health and safety of the infant. Mothers tell us they receive conflicting information and as a result, they become very frustrated, lose confidence and want to stop breastfeeding. Or, they persist with exclusive breastfeeding due to incorrect advice, and negative outcomes occur.
It is important to define what cluster feeding really is as health professionals and evaluate and intervene when an infant is in danger of insufficient feeding complications.
There is no stronger maternal drive than to feed your baby and protect him from harm. Mothers experience incredible emotional suffering when they are told their baby “was just cluster feeding,” but it turns out in hindsight they were not eating a sufficient amount, even after nursing for hours. They blame themselves rather than the health professionals who should have taken their concerns seriously.
The “Second Night Syndrome” may be common, but this does not imply that it is normal, safe or ideal. In fact, there has never been a single study documenting the safety of “Second Night Syndrome,” which we know has led to critical illness and injuries in breastfed infants who were not supplemented in a timely or adequate fashion. Our Co-Founder Jody, wrote about the Second Night Syndrome drawing from years of clinical experience working in the Nursery/NICU to inform the article. Some breastfeeding mothers talk about the “Second Night Syndrome” by describing it as absolute hell! They describe their babies as nursing non-stop and as soon as they take baby off the breast they cry frantically. The only time their babies are not crying is when they are breastfeeding. Some mothers say their babies even cry while frantically nursing and nothing consoles them. This is neither safe nor humane to the mother, who is recovering, and the baby who has to endure prolonged hunger. Such conditions not only increase the risk of feeding complications and admissions, but it can also result in accidental bed-sharing and infant falls or suffocation, known as Sudden Unexpected Postnatal Collapse.
The second night of your baby’s life should never be hell. If your baby is crying non-stop despite adequate breastfeeding, an immediate physical assessment by the RN or MD should be made to determine why your baby is crying and if immediate supplementation is necessary.
A check of their glucose, bilirubin, weight and possibly their electrolytes should be performed by a nurse, physician or nurse practitioner to assess whether a newborn is being sufficiently fed and whether supplementation is needed to protect your newborn. Research tells us that 1 in 5 mothers have delayed onset of full milk production, so we simply cannot ignore the abnormal behavior of a non-stop crying baby, knowing there will be babies who need to be supplemented.
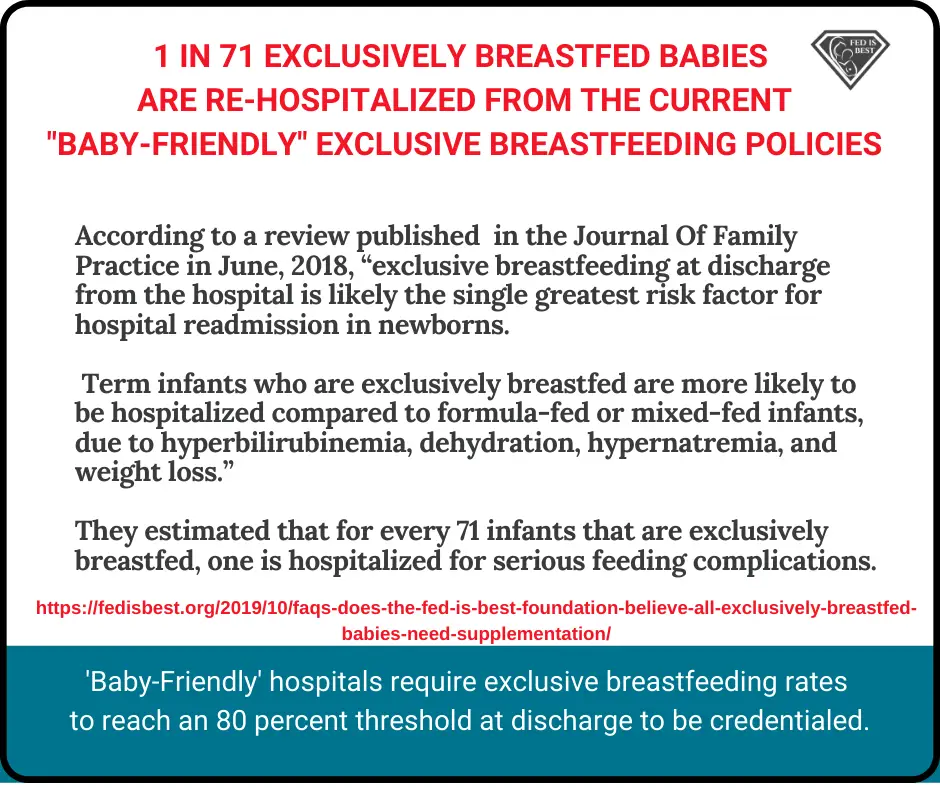
Furthermore, the exclusive breastfeeding quality metric has never been proven in randomized, controlled trials to improve breastfeeding rates, while decades of evidence have shown that rigid insistence on this metric increases the risk of harm.
FAQs Part 1: The Most Common Questions Answered At The Fed Is Best Foundation
http://fedisbest.org/2019/10/faqs-does-the-fed-is-best-foundation-believe-all-exclusively-breastfed-babies-need-supplementation/
CONTACT US/VOLUNTEER
THANK YOU FOR YOUR INTEREST IN THE FED IS BEST FOUNDATION!
Our mission statement is:
The Fed is Best Foundation works to identify critical gaps in current breastfeeding protocols, guidelines, and education programs. We provide families and health professionals with the most up-to-date scientific research, education, and resources to practice safe infant feeding with breast milk, formula, or a combination of both. To be fully informed, parents must be taught about the risks of insufficient breast milk intake while supporting exclusive breastfeeding in order to eliminate preventable hospitalizations for insufficient feeding complications. Finally, we strive to eliminate infant feeding shaming while prioritizing perinatal mental health.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join us in any of the Fed is Best volunteer and advocacy, groups. We currently have– Health Care Professional Advocacy Group, Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Maternal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org– if you are interested in joining any of our volunteer groups. For our health professional advocacy group, join us here.
- If you need infant feeding and parenting support, we have a support group– Join us here.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Sign our petition! Help us reach our policymakers, and drive change at a global level. Help us stand up for the lives of millions of infants who deserve a fighting chance. Sign the Fed is Best Petition at Change.org today, and share it with others.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educational resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write to them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop at Amazon Smile and Amazon donates to Fed Is Best Foundation.
Or simply send us a message to find out how you can help make a difference with new ideas!
For any urgent messages or questions about infant feeding, please do not leave a message on this page as it will not get to us immediately. Instead, please email christie@fedisbest.org.
Thank you and we look forward to hearing from you!

2 thoughts on “FAQs Part 3: Do You Believe Exclusive Breastfeeding is a Good Goal to Promote?”