The Newborn Weight Loss Tool can provide an answer.
Parents are taught that it’s normal for babies to lose 7–10% of their body weight in the first few days after birth, but is this true? Well, that depends. According to the AAP, a baby who loses more than 7% of his body weight may be losing excessive weight and requires a comprehensive lactation evaluation to rule out delayed onset of copious milk production, primary lactation failure, and/or infant oral anomalies that prevent adequate colostrum/milk transfer.
From the American Academy of Pediatrics HealthyChildren.org website. Breastfed newborns should lose no more than 7 percent of birth weight in the first few days after birth before starting to gain weight again. (Accessed July 16, 2020)
Weight loss has typically been assessed using simple percentages, but now there is a much more precise and accurate way to track excessive weight loss in newborns and many hospitals, pediatricians, and lactation consultants are adopting this method for greater accuracy in making clinical recommendations. The Newborn Weight Tool, or NEWT, is an online tool, the first of its kind, to help pediatricians determine whether exclusively breastfed newborns have lost too much weight in the first days of life. The tool was developed at Penn State College of Medicine through research conducted jointly with University of California, San Francisco. It was developed using a research sample of hourly birth weights from more than 100,000 breastfed newborns. For a quick synopsis of this tool from the lead investigator and one of developers of the tool, Dr. Ian Paul, watch the video below.
Source: Penn State Health News
In this video, Dr. Ian Paul, professor of pediatrics and public health sciences at Penn State College of Medicine and pediatrician at Penn State Hershey Children’s Hospital, talks about how NEWT fills an important void. Determining whether an exclusively breastfed newborn is losing excessive weight is important because higher weight loss almost always reflects suboptimal milk intake. It is also associated with increased risk of medical complications such as low blood sugar, jaundice, and dehydration, which can result in the need for medical interventions and future health and developmental problems. This weight-loss tool shows that how quickly babies lose weight is just as important as how much they lose.
How to USE the Newborn Weight Loss Tool
We recommend practicing using the Newborn Weight Loss Tool before delivery to become familiar with how it works. We have provided a few examples here to help you practice using the tool. We encourage all parents to ask their health care providers for the numbers they need (birth weight and follow-up weights in grams and time of weighing) to use this tool. Along with the Fed is Best Infant Feeding Plan, the NEWT provides parents with the confidence they need to meet their breastfeeding goals while meeting their infant’s nutritional needs safely. If you are having trouble using the NEWT resource, you may reach us at contact@fedisbest.org for assistance. For urgent medical concerns regarding your infant, please contact your pediatrician’s office.
-
- The first step is to record the weight in grams and time of the weighing each time it is done at your health facility, starting with the birth weight. The Fed is Best Feeding Plan has a helpful chart to help you record all weights and other clinical data.
- Please note the weight time entered is in military time. Click here to convert the time to military time.
- Please click here to convert pounds/ounces to grams which are used in the hospital.
- Next, go to newbornweight.org to enter the following data:
- Birth weight in grams
- Birth date and time (in military time)
- Mode of feeding: either exclusive breastfeeding or exclusively formula-feeding.
- If you are giving formula exclusively or supplementing breastfeeding with formula from the first feeding, choose exclusive formula-feeding
- Vaginal or Cesarean Delivery
- Then the next weighing after the birth weighing
- When you submit the data, the tool will plot the weight loss data on a graph. Weight loss greater than the 75th percentile (or below the yellow line on the graph) is considered to be excessive weight loss and requires an urgent assessment of the breastfeeding technique and of the newborn for signs of jaundice, dehydration, and other conditions to determine the need for supplementation.
- The first step is to record the weight in grams and time of the weighing each time it is done at your health facility, starting with the birth weight. The Fed is Best Feeding Plan has a helpful chart to help you record all weights and other clinical data.
With this tool, excessive weight loss can be detected earlier. Previously 7% weight loss was believed to be normal and safe for all newborns but if they lose this amount in the first 24 hours, this would be considered excessive weight loss that is greater than what is lost by 95% of all exclusively breastfed newborns. This may be a sign of insufficient breast milk supply and/or poor transfer of milk. Supplementation with milk bank donor milk or formula would be strongly recommended at this time if the correction of the latch is unable to stabilize the weight loss. Earlier detection and supplementation can prevent complications that could require hospital interventions and longer hospital stays. Alternatively, the tool may provide mothers reassurance that their infant is getting sufficient breast milk and that supplementation may not be needed at this time.
Keep in mind that the choice to supplement is a decision that is ultimately up to the mother, regardless of the findings of this weight loss tool. Choosing to supplement just to relieve the hunger of a persistently hungry newborn or to prevent maternal exhaustion are all valid reasons to supplement a baby. Furthermore, the best evidence available has shown that judicious supplementation after nursing sessions will not harm a mother’s chances of going on to exclusively breastfeeding thereafter may even prevent need for repeat hospitalization. Furthermore, contrary to prior claims, early supplementation in this study found no effect on the gut microbiome as previously claimed.
This is an example of how NEWT works. Click here for a demo.

Now let’s look at an example of how the NEWT tool supports successful breastfeeding while protecting the baby from excessive weight loss and the hunger and thirst that accompany it.

This baby, born by c-section at 37+4 weeks, weighed 3340 g (7 lb 6 oz) at birth. His mother was exclusively breastfeeding and was concerned that he was not getting enough milk. She reported that he would fall asleep at the breast after a few sucks, and would cry and show hunger cues when put down. The pediatrician was concerned because of the baby’s high 24-hr weight loss (>75th %ile) and the fact that his nursing sessions were so short and infrequent due to sleepiness. She recommended that the mother supplement with formula and ordered a lactation consult.
The lactation consultant helped this mother hand express and pump several milliliters of colostrum. She then worked with the mother and baby to breastfeed with a syringe of colostrum and banked donor milk slipped into the corner of his mouth. With the presence of a faster flow, the baby stayed awake for the whole feeding and then appeared satisfied after taking about 18 ml. The mother was given a milk expression plan to ensure adequate stimulation of her breasts while waiting for the arrival of her milk. When her milk came in on Day 4, the baby’s weight loss was still in the normal range (6.6%, around the 50th %ile), and she worked with an outpatient lactation consultant to return to exclusive breastfeeding.
Now let’s look at an example of how the NEWT can detect excessive weight loss.
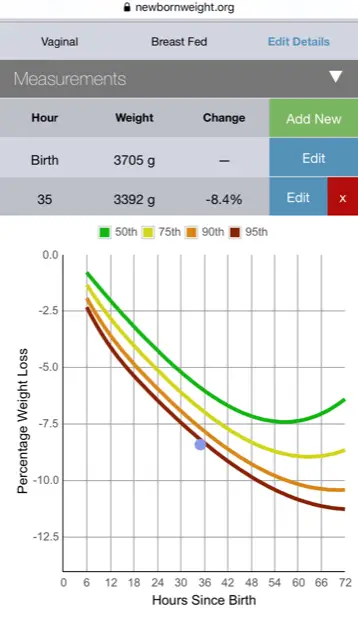
“My baby lost 8.4 percent of his birth weight at 36 hours of age, but a conversation about supplementation never happened before discharge.”
This baby lost 8.4% of his birth weight at 36 hours. No supplementation was offered. Thirty-six hours later the family found out at his follow-up appointment that his weight loss was down to 9.7% and his transcutaneous bilirubin was very high, and they had to send a blood test. The mother of the child, a physician at the hospital where she delivered stated, “The crazy thing about all of this though, was that since he had not lost over 10% of his birth weight, they did not insist on supplementation. But the lab test resulted in immediate readmission for bili lights. His total bilirubin was 21.” From the blog: Hospital Drops Baby-Friendly Program After Doctor’s Baby Was Harmed
This is another example of how NEWT can detect excessive weight loss.
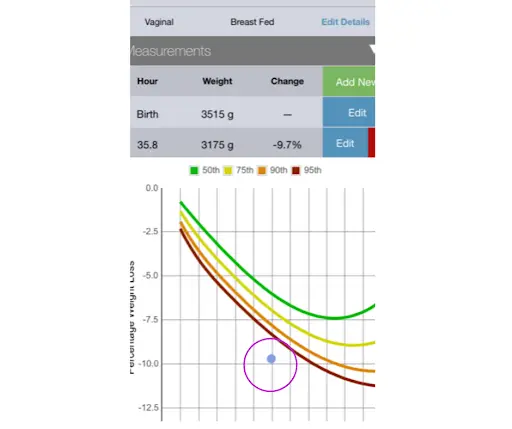
This baby had a 9.7% weight loss at 36 hours of age. Using the NEWT tracking tool, this baby had excessive weight loss at discharge—he had lost much more weight than 95% of vaginally born babies—but no interventions were suggested.
This baby was not scheduled for a follow-up pediatrician appointment until 36 hours later. Unfortunately, by the time this baby was seen in the ER, the weight loss was greater than 22%. He did not survive.
This baby was failed by the arbitrary guideline that 10% weight loss is acceptable for all babies. In addition, this baby should have been seen by the pediatrician the very next morning, which is another systemic failure. We believe if all parents use the NEWT resource, they will have immediate access to determine if their baby needs supplementation and if the mother needs lactation management. The truth is that very often babies are sent home hovering at 7–10% weight loss, putting them at risk before the onset of copious milk production. Because of this, we advocate for all discharged exclusively breastfed babies to have a next day exam and weight check by their pediatrician.
Could this be why 1 in 71 exclusively breastfed babies are rehospitalized for complications of insufficient feeding?
There is One Important Caveat
Although the Newborn Weight Loss Tool is far superior to the previous arbitrary standard of 10% weight loss as being normal, there are some limitations. The tool is the summary of average newborn weight loss in exclusively breastfed babies across a population and therefore cannot fully capture what is going on with an individual infant. As we know, statistical data on a population cannot replace the judgment of the mother and health professionals seeing an individual newborn who may be communicating that despite what appears to be a normal weight loss, they are persistently hungry and that supplementation may still be needed to prevent feeding complications. Weight loss percent is not sufficient to rule out all feeding complications. This may require further clinical evaluation like a blood glucose, bilirubin or metabolic panel, which may cause transient discomfort to your baby but may be important to ensure safe and adequate feeding.
Unfortunately, some feeding complications can occur before 7% weight loss is reached, including hypoglycemia and hypernatremia, a form of severe dehydration that can cause brain injury and increased risk of death. Studies shows that hypernatremia can occur by 5% weight loss, more typically at weight loss greater than 7% of birth weight. The data also shows that among healthy exclusively breastfed newborns, hypoglycemia and the complications it causes to the brain can occur at any weight loss percentage, because some infants are born with low caloric stores. That is why it is important to listen to the baby, first and foremost, and secondly; to all the health professionals reading this, listen to the mother when they are concerned that their newborn is not getting enough milk.
Any newborn with signs of persistent HUNGER (which we have summarized in this article) deserves a full assessment of these hunger cues, clinical signs of dehydration, jaundice, and hypoglycemia which may require blood work, particularly when the weight is above 5–7%. We encourage all mothers to listen to their instincts and raise concerns about their infants when they exhibit persistent signs of hunger despite frequent breastfeeding. In many cases, supplementation can help your infant become more alert and effective at breastfeeding, which may encourage breast milk to come in more robustly and reduce the need for further supplementation.
Written by:
Jody Segrave-Daly, MS, RN, IBCLC
Lynnette Hafken, MA, IBCLC
Christie del Castillo-Hegyi, MD
Newborn Weight Loss Calculator and Infant Growth Chart Calculator
Feeding Your Baby—When Supplementing Saves Breastfeeding and Saves Lives
How To Breastfeed During The First 2 Weeks Of Breastfeeding
Weight Loss is Not Caused by IV Fluids: The Dangerous Obsession with Exclusivity in Breastfeeding:
Know Your Risks for Delayed Onset of Full Breast Milk Supply
Knowing if Your Newborn is HUNGRY and Needs Urgent Evaluation / Supplementation
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join us in any of the Fed is Best volunteer and advocacy, groups. Click here to join our health care professionals group. We have: FIBF Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Perinatal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org if you are interested in joining any of our volunteer groups.
- If you need infant feeding support, we have a private support group– Join us here.
- If you or your baby were harmed from complications of insufficient breastfeeding please send a message to contact@fedisbest.org
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Sign our petition! Help us reach our policymakers, and drive change at a global level. Help us stand up for the lives of millions of infants who deserve a fighting chance. Sign the Fed is Best Petition at Change.org today, and share it with others.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educational resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write to them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for the legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop at Amazon Smile and Amazon donates to Fed Is Best Foundation.
Or simply send us a message to find out how you can help make a difference with new ideas!
For any urgent messages or questions about infant feeding, please do not leave a message on this page as it will not get to us immediately. Instead, please email christie@fedisbest.org.
Thank you and we look forward to hearing from you!



Great article!