By Dr. Christie del Castillo-Hegyi, M.D.
The Fed is Best Foundation has written about countless cases of serious complications caused by poor standards of breastfeeding management established by multiple exclusive breastfeeding advocacy organizations. The primary causes of these poor outcomes are:
-
- the persistent denial of the seriousness of newborn weight loss
- the lack of transparency about the consequences of insufficient feeding complications in patient education and health professional training
- and the dangerous obsession with exclusivity in breastfeeding.
Exclusive breastfeeding, according to the WHO, means “the infant receives only breast milk. No other liquids or solids are given – not even water – with the exception of oral rehydration solution, or drops/syrups of vitamins, minerals or medicine.” While breastfeeding is a positive thing to support, the obsession with exclusivity in breastfeeding promotion results in approximately 190,000 newborn admissions a year in the U.S. alone, mostly from complications of jaundice and dehydration caused by underfeeding. This article will discuss the actual reason why exclusively breastfed newborns lose weight and why newborn weight loss is not due to IV fluids given to mothers before delivery. This is to address a commonly circulated unsafe recommendation by exclusive breastfeeding advocates and lactation professionals suggesting we increase the AAP recommended maximum weight loss threshold of 7% and to weigh infants at 24 hours, which would likely increase newborn insufficient feeding complications, hospitalizations, and brain injury.
Part 1: Why a Newborn Loses Weight in the First Days
Let’s start the conversation off with why newborns lose weight in the first days of life. Exclusive breastfeeding advocates have hypothesized that infant weight loss is caused by fluid shifts and “diuresis” or elimination of fluid through urination. Diuresis is defined as overproduction of urine caused by excess body fluid, which should be at least 6-8 wet diapers a day, the normal urine production of a hydrated newborn. In fact, exclusively colostrum-fed newborns, only produce 1-2 wet and dirty diapers a day the first 2 days of life, which is lower than the normal number of wet diapers a day for a hydrated newborn. Therefore, weight loss is not in fact caused by fluid loss.
Here are some basic facts about newborn nutrition:
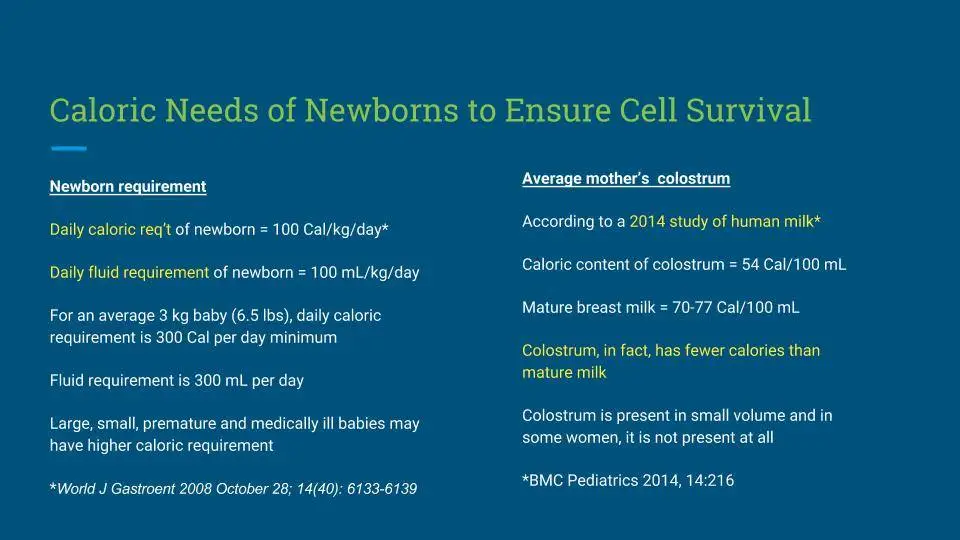
- The caloric requirement of a newborn from birth through the first weeks of life is 100-120 Calories/kg/day, a figure that is determined by the number of living cells a baby has to keep alive.
- The fluid requirement of a newborn is more variable, which can be affected by how much fluid reserve they are born with. But according to the pediatric literature it is approximately 60-80 mL/kg/day the first 2 days then 100 mL/kg/day thereafter.
- That means a 3 kg newborn needs 300 to 360 Calories per day and 180-240 mL of fluid for the first 2 days and 300 mL thereafter.
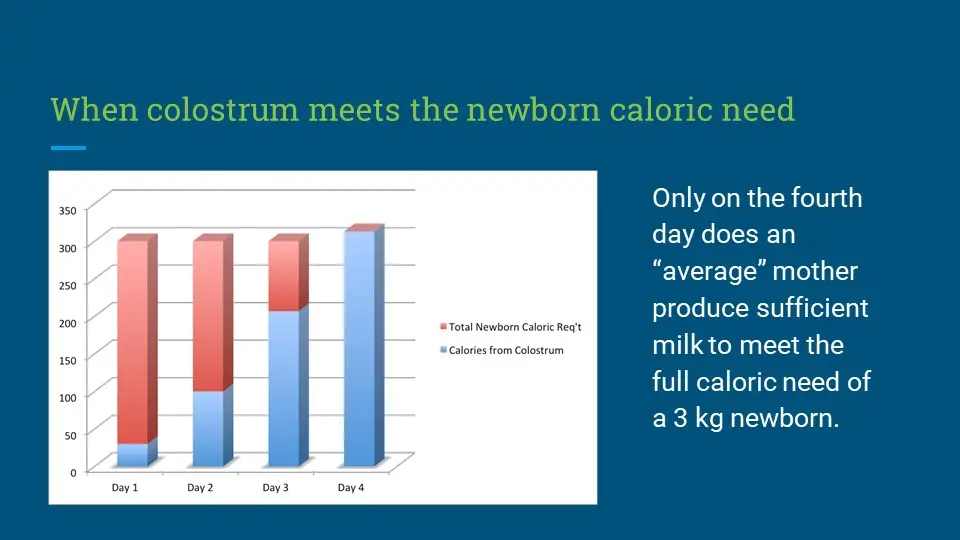
How much of this is provided by colostrum alone?
- Unlike what every parent and health professional is told, colostrum, in fact, contains fewer calories than mature breast milk which contains 54 Cal/100 mL versus 66-77 Cal/100 mL.
- Therefore, the minimum total caloric requirement is provided by 555 mL or 18.5 oz of colostrum (30 mL is 1 oz) or 454 mL (15 oz) per day of mature breast milk.
- The average mother produces 54 mL or less than 2 oz of colostrum the entire first 24 hours after birth.
How many calories does exclusive colostrum feeding provide on the first day?
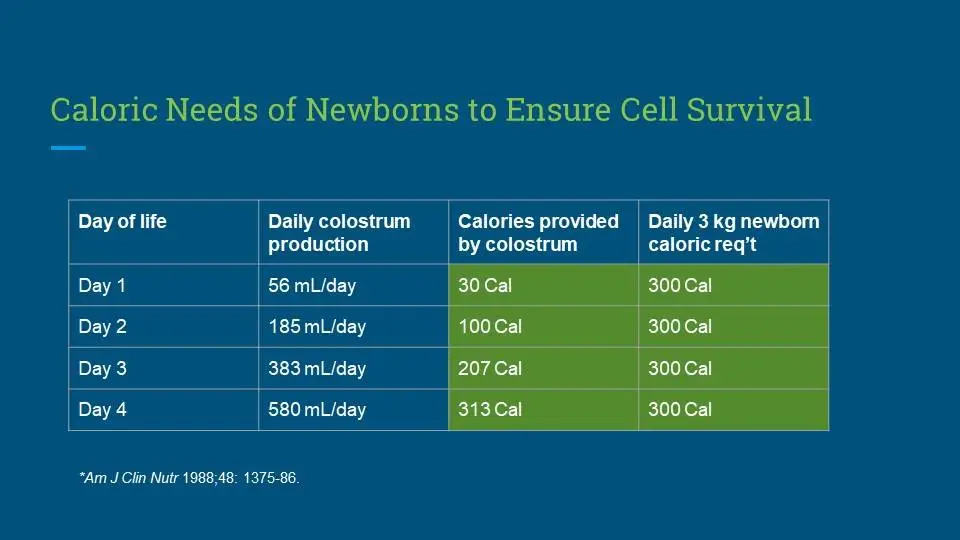
- 54 mL of colostrum provides 30 Calories while the newborn’s daily requirement is 300 Calories.
That means for the whole first day, a 3 kg newborn (6.5 lbs) is in a fasting state because they are receiving about 10% of their full requirement.
How would you feel if you were receiving only 10% of your daily caloric requirement? Pretty hungry. The adult equivalent would be if an average adult with a 2000 Calorie/day requirement received only one-and-a-half slices of whole wheat bread the entire day.
Where do the remaining calories come from?
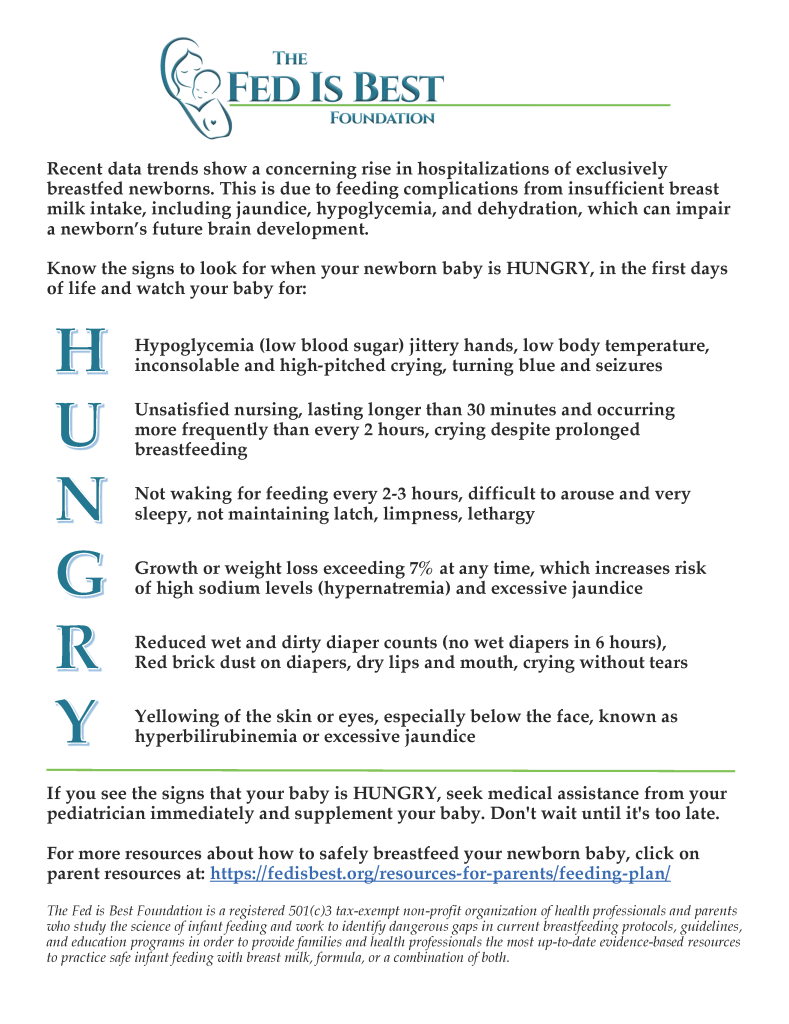
The baby will break down fat and muscle to make up for this low caloric intake and lose weight as a result. For most newborns, this fasting will cause persistent hunger and explains why many exclusively colostrum-fed newborns cry after breastfeeding—because they are hungry. This is also commonly called “Second Night Syndrome,” which is the constant crying and nursing exhibited by newborns who are experiencing persistent hunger from insufficient exclusive colostrum feeding. While some mothers do produce plenty of colostrum to prevent hunger and the negative consequences of weight loss, others do not. Close monitoring of weight loss percent, glucose, sodium, and bilirubin levels can provide objective data on safety in infant feeding but equally important is monitoring for signs of persistent hunger. Preventing a child from suffering and hunger is an important goal that has been left behind by the campaign to increase rates of exclusive breastfeeding at hospital discharge, the primary quality metric of the Baby-Friendly Hospital Initiative. While many parents and health professionals have been taught that “Second Night Syndrome” is normal and safe, there has never been any research done to confirm that it is actually safe. Persistent crying and nursing are also the same signs exhibited by infants experiencing unsafe levels of hypoglycemia and hypernatremia (a severe form of dehydration), which at this time, is inadequately monitored in the healthy, term, average-sized breastfed newborns.
How about fluid loss?
- The average 3 kg exclusively breastfed newborn receives 60 mL of fluid and their daily fluid requirement is 180-300 mL (60-100 mL/kg).
It is true, some infants may have more fluids stored in their skin due to maternal IV fluids during delivery. Infants receiving less than their full fluid requirement will start concentrating their circulating blood, which will increase the concentration of sodium in the blood. High sodium from dehydration is called hypernatremia. Newer data shows that 36% of breastfed newborns develop hypernatremia. This will cause persistent thirst. This is another reason why some exclusively colostrum-fed newborns will cry. Persistent thirst.
Mothers and health professionals have been trained to believe that forcing a newborn to subsist on this low caloric and fluid intake for a few days of exclusive colostrum feeding is “natural,” “normal,” and how we were designed or evolved to feed our babies. Assuming natural equals best is a logical fallacy, appropriately called the “naturalistic fallacy.” However, what does the historical data actually show?
Before the WHO and UNICEF, in consultation with La Leche League International, created the global recommendation to exclusively breastfeed all babies from birth to 6 months, the vast majority of breastfeeding mothers in places where formula was not available supplemented their newborns with other less nutritionally complete fluids before full milk came in. This is called “prelacteal” feeding. But why did they supplement before mature breast milk production? The vast majority believed that colostrum was not enough milk to satisfy a newborn and that supplementation with either wet nurse milk, animal milk or sugar water (likely if milk was not available) was needed to keep a newborn fed. In fact, a 2002 study of Nigerian doctors and nurses showed that nurses gave prelacteal feeds due to “insufficient milk” and doctors did it to “prevent dehydration, jaundice, and hypoglycemia.” As millions of parents and health professionals have now witnessed, many exclusively colostrum-fed newborns will cry and nurse non-stop or near continuously, some becoming dangerously dehydrated, jaundiced and hypoglycemic. Who was correct? Breastfeeding mothers and doctors from predominantly breastfeeding cultures or Western exclusive breastfeeding advocates who insisted colostrum was almost always enough?
Prelacteal feeding, which has been practiced in every pre-industrial breastfeeding culture in the world, has been deemed by exclusive breastfeeding advocacy organizations as uneducated, unsafe, “cultural” but ultimately harmful to breastfeeding and breastfed newborns. Why do they believe that it is harmful? Some newborns were likely fed less than sterile supplements like unpasteurized milk and teas and some even developed severe gastrointestinal illness from contaminated supplementation. But more importantly, it was deemed harmful because it did not conform to the “exclusive” breastfeeding mandate. But who was right?
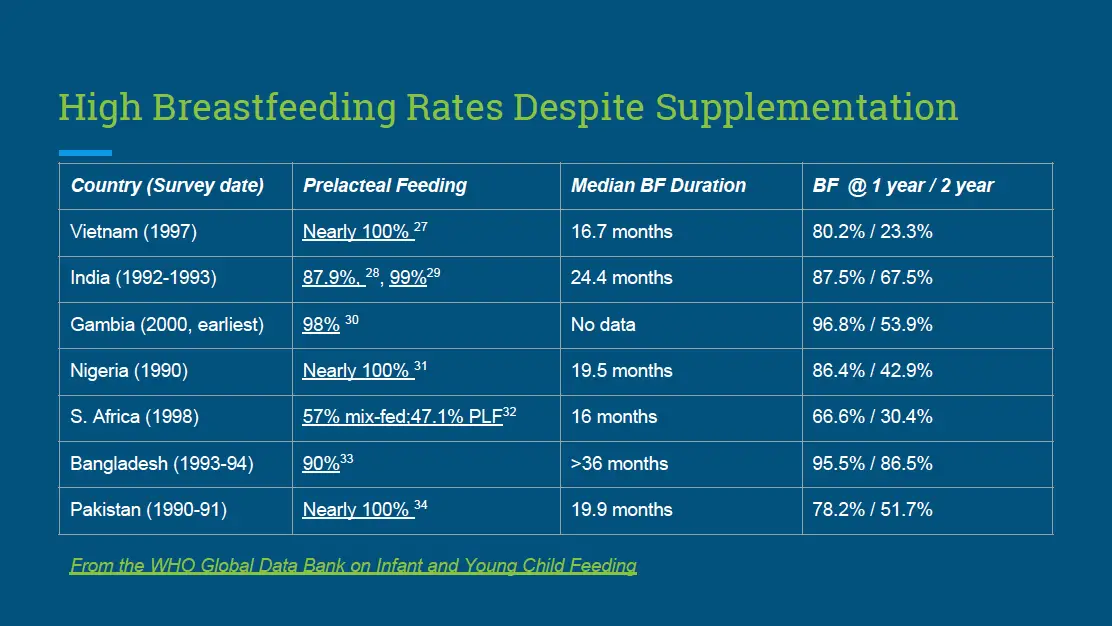
Early supplementation was widely practiced in countries where the majority of mothers breastfed to 1-2 years of life.
Many exclusively colostrum-fed newborns are getting a fraction of their caloric requirements and therefore they are hungry. Breastfeeding mothers have long responded to their babies’ hunger cues with supplemental feeding to prevent hunger if breastfeeding was not enough. This is an advantageous trait that protects babies from the dangers of starvation. The WHO and other exclusive breastfeeding advocacy organizations have stated the colostrum is sufficient to meet a newborn’s nutritional needs without ever stating how many calories a newborn actually needs or how many calories colostrum actually contains. They have even commonly stated that “it is not important how many calories a newborn receives.” According to what study documenting safety? None, whatsoever.
What we now know is that most mothers’ colostrum has fewer calories than can prevent fasting and catabolism, which causes weight loss. Weight loss eventually leads to dehydration, jaundice, and hypoglycemia, also known as the syndrome of starvation. Ultimately, we are fasting exclusively colostrum-fed newborns until a mother’s milk comes in sufficient quantities to prevent starvation. That is why breastfeeding mothers before the WHO guidelines supplemented with prelacteal feeds: to prevent hunger, fasting, starvation and ultimately infant death. They followed the first law of nature, which is “fed is best.”
So what is natural? What did human beings evolve to do? Were we designed to all uniformly exclusively breastfeed from birth to 6 months and let our infants cry for days until milk comes in? Or were we designed to listen to babies and protect them from hunger? Ask yourself who benefits from forcing babies to cry while waiting for your milk to come in? It’s not the moms who have to endure days of sleep-deprivation while trying to console a hungry baby. It’s not the babies who have to endure days of hunger and thirst, some of whom will require hospital admission. Who truly benefits from this system of breastfeeding promotion? Five randomized controlled studies have now shown that judicious supplementation does not interfere with breastfeeding at 3 months, and even up to 1 year of age (when adjusted for confounding maternal intended duration to breastfeed). How many randomized studies show the opposite? None.
Here’s an example of how supplemented breastfeeding is widely practiced to buffer infants from the harmful effects of imperfect breast milk supply.
From the Skeptical OB article entitled “100% of Maasai women breastfeed for a year or more but they’re doing it wrong.”
“100% of the Maasai women breastfed, Nearly 100% began breastfeeding within an hour of birth, 100% breastfed for a year or more, 100% received breastfeeding guidance and support from an older female relative. It’s just the type of indigenous practice that breastfeeding researchers like to invoke when encouraging women in the industrialized world … except for the most startling statistic of all: Supplementing breastfed babies is a universal practice. 0% of the Maasai women breastfed exclusively; 100% of the women practice supplementary feeding!”
What happens the following days?
If a mother-baby pair is lucky, the colostrum will increase to 180 mL in the second 24 hours, which provide 97 Calories, about a third of the newborn’s daily requirement. The weight loss may slow down but the baby is still in a fasting state because they are not receiving their full caloric requirement, which will cause more weight loss. Hunger and thirst can still persist.
On the third day, colostrum may increase to 360 mL. This volume may meet the full minimum fluid requirement but it still does not meet the full caloric requirement, providing only 195 Calories, about 65% or 2/3rd of the full requirement. Baby will still be hungry and will still be losing weight.
How would you feel if you experienced 3 days of fasting and fluid restriction as recommended by the Baby-Friendly Hospital Initiative? Pretty bad. Which is why as many as 10% of vaginally-delivered and 25% of cesarean-delivered exclusively breastfed newborns will lose excessive weight of >10%. Think about it. If all colostrum were actually enough to feed a newborn, why would so many newborns cry, lose weight and develop the complications of insufficient feeding like dehydration, hypoglycemia, and jaundice? Because for many more newborns than exclusive breastfeeding advocates choose to believe, colostrum is actually not enough.
Unfortunately, half of exclusively colostrum-feeding newborns will receive even less than this average because of maternal milk supply. Some will be bigger babies with higher caloric needs or have a smaller caloric reserve, so they will run out of reserve sooner. Some mothers do make enough to prevent hunger. For some babies, their weight loss is tolerated without consequence. The babies who receive the least number of calories and fluid through exclusive breastfeeding will eventually run out of fuel to cry and nurse, will start sleeping or may be difficult to wake for a feed. Unfortunately, in the most severe cases, newborns will seize or stop breathing from excessive jaundice, hypernatremia, and hypoglycemia. The least fed newborns are the most likely to need admission for phototherapy, IV fluids, dextrose and rescue supplementation. They are also the ones most likely to sustain brain injury and have impaired future brain development. Few parents are informed about this when they are encouraged to exclusively breastfeed their newborn and avoid supplementation despite signs of persistent hunger. How can exclusive breastfeeding advocates justify teaching mothers about the largely theoretical risks of formula while ignoring the life- and brain-threatening risks of insufficient breast milk?
Part 2: Weight Loss is Not Caused by IV Fluids Alone
One of the most negligent recommendations that have been circulating in the lactation community is to change the starting point of measuring a newborn’s weight to 24 hours after birth and to consider almost all weight loss as caused by IV fluids given to the mother during birth. Why do they want this? So that infants, regardless of how much they cry from hunger and thirst during this period, are not supplemented so that they can reach their organizations’ exclusive breastfeeding quality improvement metric.
Why is this a bad idea?
The short answer is that the more weight a baby loses, the closer they are to crossing their starvation threshold, which causes brain and vital organ injury. Starving a child not only tortures a baby, but it can cause permanent damage.
We do not know when a baby will cross that threshold and that threshold is different for every child. Furthermore, delaying the weighing to 24 hours after birth in order to increase rates of exclusive breastfeeding before discharge will increase the number of children requiring admissions to correct insufficient feeding complications and will likely permanently harm and maybe kill more babies. For many of our supporters whose newborns have been admitted for jaundice, dehydration or hypoglycemia, some whom have gone on to have developmental disabilities, their children would likely have had worse impairments in brain development. In fact, given the known data on serious complications from weight loss in exclusively breastfed newborns, the AAP has recommended no greater than 7% weight loss in their 2013 breastfeeding guidelines.
Remember this:
No scientific research looking at long-term health and neurological outcomes has ever been done to show that 10% weight loss is safe for all newborns. Not once, not ever. So pushing the weight loss threshold further puts more infants at risk of hospitalization, brain injury and death than are already at risk because of the Baby-Friendly protocol.
The only study using developmental testing looking at the effects of dehydration on newborns is this study, looking at development at 5 years of age in infants who were rehospitalized for dehydration with a weight loss of ≥12% or serum sodium ≥150 mEq/L (hypernatremia). What did this study find? Luckily, the average scores on the developmental tests and the neurological exams were not different between the dehydrated and non-dehydrated newborns. However, there were very important differences that do matter to parents. The study found that the dehydrated newborns were more likely to be exclusively breastfed when compared to the non-dehydrated newborns (88% vs. 58%, p < 0.001). The study investigators found that dehydrated infants were more likely to have poorer fine motor development (40% versus 30%; p = 0.04). Also dehydrated children were more commonly reported to have higher rates of ‘shyness’ (63% vs. 52%, p = 0.05), ‘allergy’ (42% vs. 23%, p < 0.001) and ‘disability’ (15% vs. 7%, p = 0.019, double the rates of non-dehydrated newborns). Finally, parents of dehydrated children were more likely to report a concern about their child’s speech (26% vs. 18%; p = 0.017). Unfortunately, they did not refer to a speech pathologist to formally measure language development using standardized testing, instead looking at the study psychologist or neurologist notes for indications of speech impairment. Their estimations showed no significant differences between the groups (11% vs. 16%,p = 0.40). At best, one cannot determine whether or not dehydrated newborns were in fact delayed in language development.
What the newer evidence suggests is that serious complications can happen before 10% weight loss is reached. In exclusively breastfed newborns screened for hypernatremic dehydration, a serious form of dehydration that can cause brain injury and increased risk of death, 36% were hypernatremic (>145 mEq/L) and the complication occurred by 5% weight loss! A sodium level of 150 mEq/L, which is considered moderate hypernatremia, has been shown to be associated with lower developmental scores at 12 months of age, which occurred to 50% of hypernatremic newborns.
At this time, exclusively breastfed newborns are not screened for hypernatremia. So how many cases of hypernatremic dehydration in exclusively breastfed newborns have we missed over the 28 years the BFHI has been practiced in hospitals? Millions. In addition, insufficiently fed breastfed infants have been shown in the published literature to also develop unsafe levels of hypoglycemia at any percent weight loss and can develop extensive brain injury as a result. Most hospitals do not routinely screen all babies for hypoglycemia.
Unfortunately, mothers will commonly be taught by health professionals educated and trained by the Baby-Friendly Hospital Initiative that persistent crying and nursing is normal and safe newborn behavior despite the fact these are also signs of dehydration, hypernatremia, and hypoglycemia.
Are IV fluids the cause of newborn weight loss?
The lactation community commonly cites one study to justify their conclusion that all weight loss is caused by IV fluids, which justifies measuring weight loss at 24 hours and thereby pushing the acceptable weight loss to allow before supplementation occurs. It is a study called “Excess Weight Loss in First-Born Breastfed Newborns” by Chantry et al. The study looked at first-born newborns looking for risk factors associated with excessive weight loss of >10%. One factor they looked at was whether there was an association between IV fluids given to mothers before delivery and newborn weight loss. The idea is that more IV fluids a mother gets, the more fluid a baby will be born with at birth, which is thought to be all “water weight.” Therefore, moms who get more IV fluids should have higher rates of excessive weight loss in their newborns. If there is an association, then it is possible that weight loss is simply a loss of water weight and not true weight loss from malnutrition. What does the actual data show?
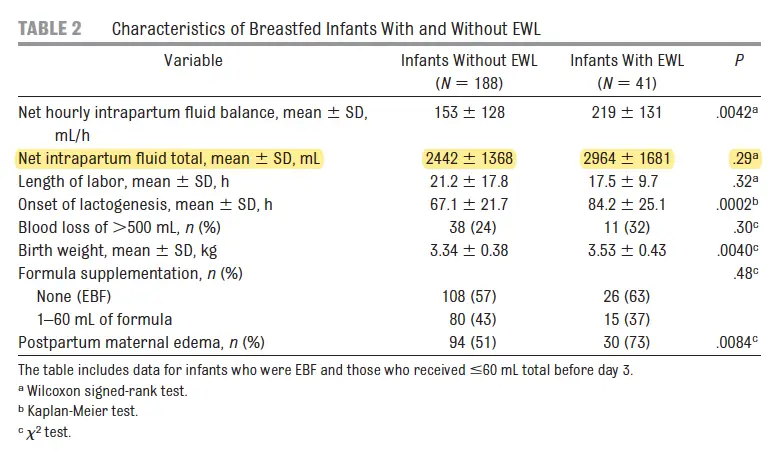
When you examine the data, the authors of the study looked at the total net volume of fluid the mothers received (total IV fluid minus the volume urinated by mom, which they called the net intrapartum fluid total) and looked for an association with newborn weight loss percent, which physiologically, would be the greatest determinant of how much water weight a newborn gets through the placenta. However, they found none! Mothers who received a more net volume of fluids did not have statistically higher rates of newborns losing excessive weight (>10%) (see table below).
Figure 1. Table from Chantry et al. The infants with excessive weight loss had mothers with an average of 29464 +/- 1681 mL compared to 2442 +/- 1368 mL, which was not significantly different (the p-value should be less than .05 if it were and in this case with was .29)
So the authors persisted and looked for another variable related to IV fluids, namely, the rate of IV fluid delivery. The authors found that mothers who received IV fluids at a higher delivery rates (net hourly intrapartum fluid balance >200 mL/hr) did have higher rates of having a newborn that lost excessive weight compared to the low rate group (<100 mL/hr), which increased the rates of excessive weight loss by 3.18 fold. They concluded that because there was a statistically significant increase in excessive weight loss in the higher IV fluid rate group, the weight loss was due to water weight loss.
Why is this slightly ridiculous? Think of it this way, when you fill up your car with gas, does the rate at which the gas pump delivers the gas affect how much gas is your car? No. In the same way, the rate at which the mom receives IV fluid is unlikely to have anything to do with how much fluid the mom’s body has at the time of delivery or how much a baby gains in water weight before being born. The baby’s body weight is more likely to be affected by the total volume of IV fluids the mother receives, not the rate at which she receives it.
The authors did find that the moms who received higher net rates of fluid delivery had higher rates of induction, longer duration of labor and longer periods without sleep before birth. Prolonged labor and other stressors during delivery are known risk factors for delayed lactogenesis II and low colostrum/milk production. Low colostrum/breast milk production and delayed lactogenesis II both cause excessive weight loss because those infants are fed the least amount of milk. In addition, infants with prolonged and complicated deliveries are at the highest risk of having a low caloric reserve.
Despite this, the authors claim that the higher rate of IV fluid delivery suggests that some weight loss may be caused by IV fluids. This has been morphed by the exclusive breastfeeding advocates to mean all weight loss is caused by IV fluids and have even applied it to their clinical practice before any research on safety has been done. Even the authors state in their discussion that, “We postulate that weight loss associated with positive maternal fluid balance represents a loss of excess fluid in the newborn, but caution must be exercised because this weight loss might represent a loss of ‘true’ weight through inadequate nutrition.”
Unfortunately, the authors failed to emphasize the most significant findings in their study, which were:
- The highest risk factor identified by the authors for excessive weight loss is delayed lactogenesis II, which increased the risk of EWL by 3.35-fold.
- Furthermore, they noted that 42% of first-time moms experienced delayed lactogenesis II, which is an incredibly high number of exclusively breastfed newborns at risk of excessive weight loss and its related complications.
- The actual highest risk factors for excessive weight loss identified by the study were exclusive breastfeeding and near-exclusive breastfeeding, which occurred to 19% of exclusively breastfed newborns, 16% of minimally supplemented newborns (<60 mL per day) and only 3% of infants supplemented >60 mL per day. This correlates to a 5- to over 6-fold increased risk of excessive weight loss.
Given high rates of excessive weight loss related to delayed lactogenesis II and exclusive or near-exclusive breastfeeding and given the known serious complications associated with greater than 7% weight loss including hypernatremia and hyperbilirubinemia (jaundice), this study suggests that far more babies than expected by the standard of care will need supplementation with donor milk or formula to prevent serious feeding complications.
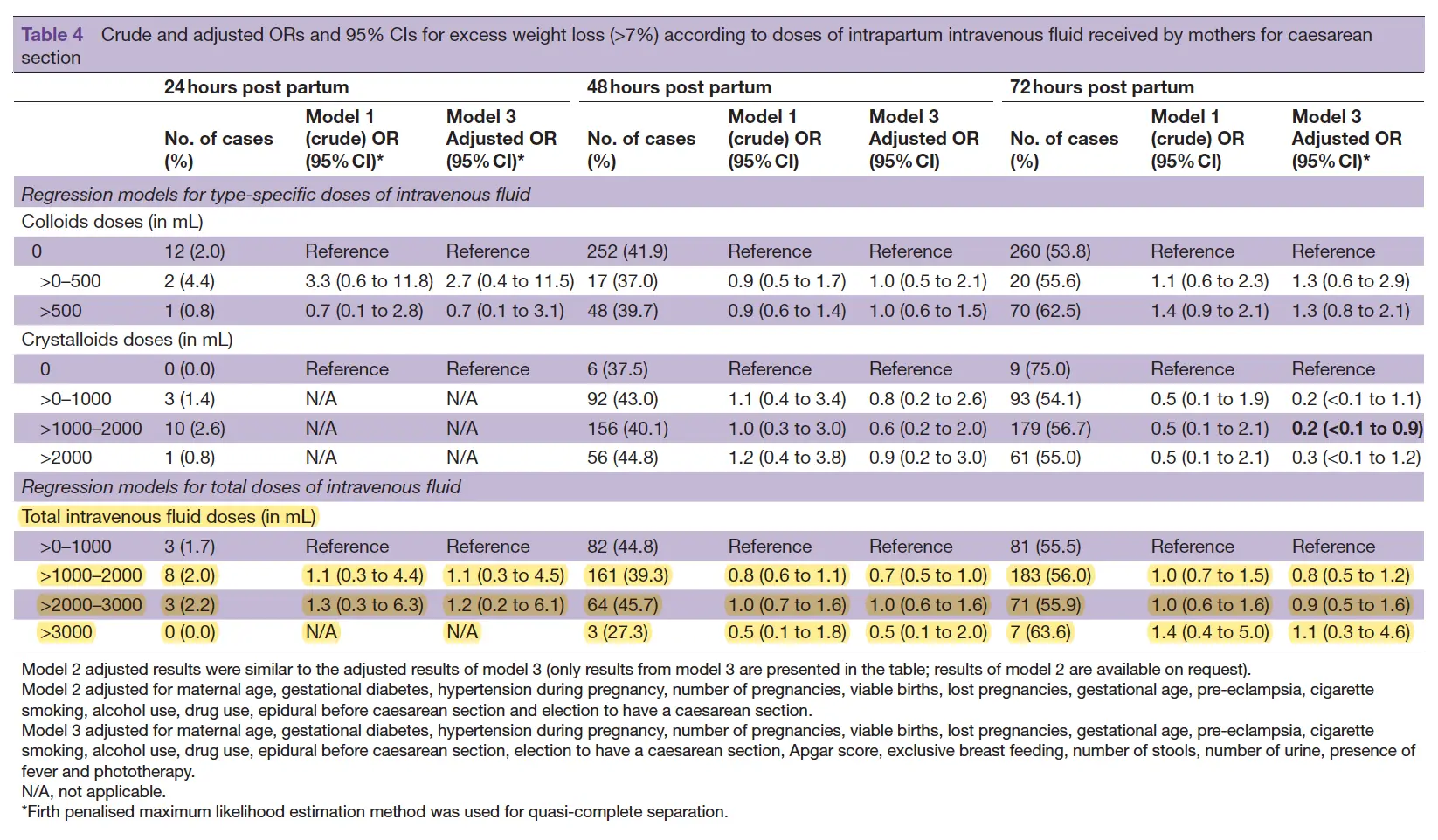
Other studies have similar findings like this study, “Intrapartum intravenous fluids for caesarean delivery and newborn weight loss: a retrospective cohort study” by Eltonsy et al., which also found that there was no difference in excessive weight loss between infants whose mothers received high volumes of IV fluids versus low volumes, which this study defined as > 7%. They also found that exclusive breastfeeding was a risk factor for excessive weight loss.
Figure 2. Table from Elstony et al. Odds Ratios (OR) around 1 with 95% confidence intervals (CI) that cross 1 means there were no differences. The above table shows that >1000-2000 mL and >2000-3000 mL of IV fluids had no relationship to excessive weight loss.
Here are a few more studies for those interested:
A study Noel-Weiss et al. found a statistically significant difference between mothers who got less than 1200 mL of IV fluids versus those that got greater than 1200 mL, which resulted in an average newborn weight loss of 5.51% vs. 6.93%, respectively. However, this difference was only significant at 60 hours of life and specifically stated there was no relationship between maternal IV fluids and weight loss before 60 hours, which would not apply to many mothers getting discharged at 48 hours. While the difference was statistically significant, the difference was clinically insignificant with a difference of only 1.42%. Does a 1.42% difference mean that all or almost all weight loss is caused by fluid loss? No. That means a fraction of the weight loss can be accounted for by fluids. This study also found that the delayed onset of lactogenesis II occurred to 41% of their sample, which also correlated with newborn weight loss.
Another study entitled “Relationships among intrapartum maternal fluid intake, birth type, neonatal output, and neonatal weight loss during the first 48 hours after birth” found no relationship between IV fluids and newborn weight loss. They found that exclusive breastfeeding and the number of wet diapers were better predictors of excessive weight loss.
One of the strongest study designs was, “A Randomized Controlled Trial of the Effect of Intrapartum Intravenous Fluid Management on Breastfed Newborn Weight Loss” randomizing 200 women to receive 500 mL of IV fluids at low (75-100 mL/hr) vs. standard (125 mL/hr) IV fluid delivery. They found no differences in an excessive weight loss of >7% between the two groups of breastfed infants.
The Dangerous Obsession with Exclusivity in Breastfeeding
As I have written about in a different blog, not even the WHO in their 2017 revised breastfeeding guidelines could find any evidence of sufficient quality to support Step 6: “Give no food or water other than breast milk unless medically indicated.” The two randomized, controlled studies cited by the Cochrane review they cited found a slight improvement in breastfeeding rates of 21% in newborns who were supplemented. Despite those findings, the exact opposite was ultimately recommended, which was to stick with the exclusive breastfeeding from birth recommendation. The WHO officials in our September 2017 meeting admitted to not knowing how many newborns developed complications from their exclusive breastfeeding guidelines as they had no programs to monitor safety and stated that all health workers trained in the Baby-Friendly program were taught to look for infants that were “convulsing, lethargic or poorly feeding,” not realizing that these were signs that brain injury has already occurred.
Likewise, the authors of the Chantry study either could not see or chose not to see that the leading risk factor for excessive weight loss was in fact, exclusive breastfeeding. The ability to ignore findings that cast a negative light on the exclusive breastfeeding standard even during the short time before birth when every objective measure shows the milk is commonly not enough shows you the dangerous obsession with exclusivity in breastfeeding advocacy. Because they receive minimal training by the BFHI curriculum on the serious consequences of dehydration, jaundice, and hypoglycemia to a newborn, they appear to be dangerously unaware that pushing this weight loss threshold will result in more infant harm.
It has become a disturbing trend among breastfeeding medicine and lactation professionals to push the boundaries of safety farther and farther back to promote exclusive breastfeeding. Children have literally lost their lives and futures to this obsession as they have pushed to get health professionals to tolerate lower and lower glucose levels, that have now been shown to be brain-threatening, and higher and higher weight loss percentages to prevent newborns from being supplemented. Exclusively breastfed newborns are literally crying day and night from hunger in hospitals and nurses and doctors are helpless to protect them from these dangerous outcomes by offering supplementation lest they get written up or potentially lose their jobs. The risk of brain injury from these complications that now hospitalize perfectly healthy newborns every single day is hidden from parents. Never in the history of medicine has there been such a blatant disregard for patient safety and patient rights before the Baby-Friendly Hospital Initiative. Never have nurses and doctors been muzzled in a way that prevents them from protecting their patients.
This is why the Fed is Best Foundation exists. When the most prominent infant feeding organizations focus all their energies on achieving exclusivity in breastfeeding for as many mothers and babies as they can, they forget the most important thing in infant feeding, which is safety. What results is an unethical, unsafe and inhumane system of feeding that impairs new parents with sleep deprivation and routinely puts newborns at risk. Because too many parents and health professionals have witnessed the unspeakable harms of the exclusive breastfeeding standard, particularly in the days after birth, we will continue to inform parents and health professionals of these harms until the standard changes to protect families and infants from these tragedies.
Safe breastfeeding resources
How To Prepare For Supplementing When Breastfeeding Your Baby In The Hospital
http://fedisbest.org/resources-for-parents/fed-best-guide-safe-infant-feeding-educational-packet/
Knowing if Your Newborn is HUNGRY and Needs Urgent Evaluation / Supplementation
Feed Your Baby—When Supplementing Saves Breastfeeding and Lives

Exclusively breastfed newborn baby who developed dehydration and jaundice from insufficient feeding
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join us in any of the Fed is Best volunteer and advocacy, groups. We currently have– Health Care Professionals group, Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Maternal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org– if you are interested in joining any of our volunteer groups.
- If you need support, we have a private support group– Join us here.
- If you or your baby were harmed from complications of insufficient breastfeeding please send a message to contact@fedisbest.org
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Sign our petition! Help us reach our policymakers, and drive change at a global level. Help us stand up for the lives of millions of infants who deserve a fighting chance. Sign the Fed is Best Petition at Change.org today, and share it with others.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educational resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write to them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop at Amazon Smile and Amazon donates to Fed Is Best Foundation.
- If you need support, we have a private support group– Join us here.
Or simply send us a message to find out how you can help make a difference with new ideas!
For any urgent messages or questions about infant feeding, please do not leave a message on this page as it will not get to us immediately. Instead, please email christie@fedisbest.org.
Thank you and we look forward to hearing from you!


3 thoughts on “Weight Loss is Not Caused by IV Fluids: The Dangerous Obsession with Exclusivity in Breastfeeding:”