Among the most vulnerable moms are those who are most educated in exclusive breastfeeding. Because we are trained to fully believe in the guidelines recommended by health organizations and because mothers are not educated about the complications of underfeeding, we can miss serious signs of newborn starvation. Rachel is a Pediatric Nurse Practitioner. She would like to share her story so that other mothers and babies do not have to suffer.
As long as I can remember, I wanted to be a mom. Fresh out of nursing school, I started out as a neonatal nurse in the ICU. I watched the tiniest of babies get fed through tubes. We carefully monitored their weight every day, eventually most would go home, happy and healthy. A few years later, I became a Pediatric Nurse Practitioner and saw babies in an outpatient setting as a primary care provider. I would monitor babies’ weights and help moms through their struggles with breastfeeding and feeding in general.
When it was finally my turn to become a new mom last October. I figured “I got this!” I took all the breastfeeding classes I could, received a ton of breastfeeding supplies and even bought a really expensive nursing chair. I was blessed with a very healthy pregnancy and “normal delivery,” my son even came on his due date of all days. When he came out, we did skin-to-skin for about 20 minutes before they took him and weighed him, 8 lbs 15 oz! They brought him back to me, but my son, Hunter, didn’t “latch on” right away as they told me he would in the classes. He didn’t even “look for my breast.” By time we got into our recovery room, I ate (I went 24 hours without eating, I was starved after labor!), it was about 4 hours after delivery before Hunter finally latched on. The night nurse came into my room to help me breastfeed my son for the first time and I remember her pulling at my nipple “to get it to flowing.” The pain from the tugging and pulling was nothing like I have ever experienced before. It hurt and very badly too! All of this, only to get out a tiny drop of “liquid gold” as they so often call it. I remember him crying and getting frustrated because nothing was coming out. I could barely hold him because I still had an IV in my left wrist and it was painful to get him into the best position. “It’s ok,” the nurse said, “he can go a while without eating, his tummy is so small.”
Somehow, I made it through the first night. The next morning was a blur, doctors coming in to check on him, myself, others asking to fill out forms. I finally got to see a lactation consultant (LC) at 11 AM. She told me my nipples were “inverted” and that I needed a nipple shield, you know that plastic sombrero looking thing that goes over your nipple. Hunter did well and finally “ate,” almost 18 hours after delivery. Before the LC left, she warned me, “get ready for tonight, he is going to want to eat every 15 minutes.” This scared me to death. How was I supposed to have him latch on every 15 minutes? My nipples would crack and bleed before I even started to become “successful” at breastfeed and I would just give up. As the day went on, he had a few medical procedures and was very sleepy from those, but still need to have a wet diaper before going home. By the evening time, Hunter was awake. I tried to get him to latch on and he did “okay” but it was still very painful. He cried every 30 minutes for a solid two hours before I finally “gave in” and gave him 20 mL of formula. I was realistic and brought supplementation formula to the hospital with me. I told myself, “this is temporary, just until your milk comes in.” He drank it all within the blink of an eye and slept peacefully until 3 hours later. The next day, going-home day, Hunter had about four 20 mL feedings of formula overnight and finally urinated. My OB came by to visit me, watching my husband give him a bottle before we left. I could feel the “judgment” of “he’s going to have nipple confusion you know.” I second guessed myself that I gave him too much formula (based on the pictures they showed in the class and in the booklet). Determined, I was only to breastfeed him when I got home. I felt so guilty that I “had to” give him formula. Hunter left the hospital on day three of life, weighing 8 lbs 3 oz (down 8% from delivery). By day 4, my milk came in. I needed to go to the store to get some more breastfeeding supplies, (hey, my husband would be clueless if I sent him to the store). I was gone for less than two hours and in that time, and my husband gave Hunter more formula, “because he kept crying.” I was angry, how could he be hungry, I just fed him! No more formula, it’s not “what’s best for him, my milk is what is best for him,” and I stopped all formula. We saw his doctor the following day, still at 8lbs 3 oz., which she was “fine with, as long as he was having wet diapers.” Next checkup in two weeks. I thought I was doing well with breastfeeding. I even checked off all the little boxes in the breastfeeding guide they gave me at the hospital, ensuring he had enough diapers and stools each day. Three days before our two week checkup, Hunter stopped stooling. My mommy brain said “something is wrong.” My nurse brain told me “it’s ok, he can go a few days without stooling, he is still urinating ok.” But he wasn’t, his urine was even turning orange, which indicted he was dehydrated. Still, I pushed through. Maybe it was the lack of sleep that hindered my nurse brain.
The dreaded weight check-up day. I put Hunter on the scale and blinked twice at the numbers that flashed before me. It read 8 lbs 3 oz. He gained NOTHING, but didn’t lose any additional weight! My nurse brain kicked in, and I knew what I was going to have to do, supplement formula. I cried (and a lot) and was so upset. I failed at breastfeeding, my body failed me. How could I have done that? How could I have not known better and starved my son. All the signs were there, not stooling, orange urination, and the sleeping 4+ hours at night. I thought it was just luck to have my son sleep long periods of time. My pediatrician told me, “Feed him more often and come back tomorrow. If he gains 1 oz, I will let you keep breastfeeding him.” “Let me?” As if I need permission to continue to do something I so desperately wanted to do. But I had too, Hunter was under the 5th percentile for weight. The next day, we brought him back, and the scale read 8 lbs 4 oz,. YAY! He gained one oz, and he stooled twice yesterday. I did it, I felt like the best mom in the world, so happy I fed him “enough.” Little did I know that night would be the worst night of my life. It was 1 AM and Hunter was trying to breastfeed, and wouldn’t latch on, he was crying, NO – more like screaming, because he was starving! Hysterically crying myself, I broke down. “Give him the formula,” I told my husband, “but just 1 oz, no more!”
Again, I made it through another rough night, determined to figure out what went “wrong.” I started pumping as my husband fed Hunter more formula. I got out 75 mL out….not bad I thought! I was proud of myself, I had “plenty of milk” for him. I figured, well I need to go back to work in a few weeks, and I will have to pump anyways, let me just started pumping and bottle feeding him, then I will know how much he is getting. So starts my pumping journey. It was horrible. The pain, the swelling….only getting out anywhere from 1-2 oz total each session. I saw an LC 3 weeks after delivery and she told me my nipples were not “inverted” and to stop using the shield. Somehow Hunter’s “raw latch” (without the shield, that even more was painful) managed to get out 51 mL during a weighted feed. But I still figured pumping was better. From that day forward, Hunter got a mixture of breast milk and formula, but I “limited” how much he got because I didn’t want him to become “overweight.”
Over the next 6 weeks, I found out I have very elastic breast tissue (small percentile of women have this issue), which would cause my nipples to swell (to very large sizes) when I tried to pump, eventually shutting down my milk ducts after 5 minutes of pumping leading to very little output. I would never be able to pump enough for Hunter and only could give him a little under ½ of what he needed each day, average pump session 12 oz total for the whole day. I would also go through 6 different herbal supplements, 9 different flanges (even had some hand-created for me, but didn’t work out sadly), another four LC visits and 3 different pump systems to increase my milk supply before I would finally “give up.” I was desperate and would pay a million dollars to give my son more breast milk. I returned to work after 8 weeks and that made pumping what small amount I was getting that much harder. I work at a very busy urgent care setting and barely had enough time to eat let alone pump every three hours.
During the month of December, I became very sad and extremely guilty that I was not able to give him “enough” breast milk. Sure, he was gaining weight, but I never felt “complete.” I would cry on my way to work, and my nurse brain knew I had postpartum depression when I started to avoid feeding him, on purpose. I couldn’t stand to look at the formula in the bottle, another constant reminder that it wasn’t my milk. It wasn’t my gift I was able to give to him. I wasn’t able to “parent” the way I hoped to. The never ending thoughts (and you have so many thoughts as a new mom) led me to finally seek professional help. It was recommended that I stop pumping at Hunters 3 month mark. My last pump session I only got out 10 mL total and I cried as he drank it, mixed into the formula. Hunter had no idea what was going on. He only cared that someone was feeding him, changing his diaper and loving him. He didn’t even notice the difference when I stopped pumping. Eventually a few weeks later, I did a trial of “re-lactation” and even put myself on a medication with potential very serious side effects, to prove that I was a good enough mom to give it one last shot. I think it was my way of grieving the loss of not being able to be successful at breastfeeding when I had been very successful my whole life. After two weeks of “re-trying” I stopped for good. I gave myself permission to stop. Stop all the negative thoughts and enjoy my time with my son instead of being hooked up to a pump.
Hunter is now fully formula fed and is right at the 50% percentile for weight at 4.5 months old and is a very happy baby. (Note: as a NP I never care much about the charts, as long as he was growing on his own curve and upward!). I don’t know why I put so much pressure on myself to breastfeed only and clearly missed the signs that I starved him, by accident! Maybe it’s because I was supposed to be the “role model” nurse that breastfed her child. Our society is unfortunately not set up to be successful at breastfeeding. With most moms getting only 1 postpartum visit at 6 weeks and having to pay $100+ to see an outpatient LC, no wonder we have one of the lowest breastfeeding rates in the world. I was not getting paid leave and the stress of trying to be “the best mom ever,” really affected me and I missed out on enjoying the short time off from work with my son. I hope other moms will read this and know they are not alone – you are never alone. Even has a health care professional, I still missed the signs. It’s so easy to do when it’s your own. Please know you are not a horrible mom for ensuring your child is fed. Don’t be ashamed of breastfeeding your child for as long as you like or stopping and giving formula. The best advice I got, was your child will need you for so many things in their life. Early infant feeding is such a small part of their life. Please don’t stress over it not being perfect. In the end, we all want the same thing, healthy children who are loved and well fed!
Educate yourself and seek help if something doesn’t feel right. I promise in the end, everything will be just fine!

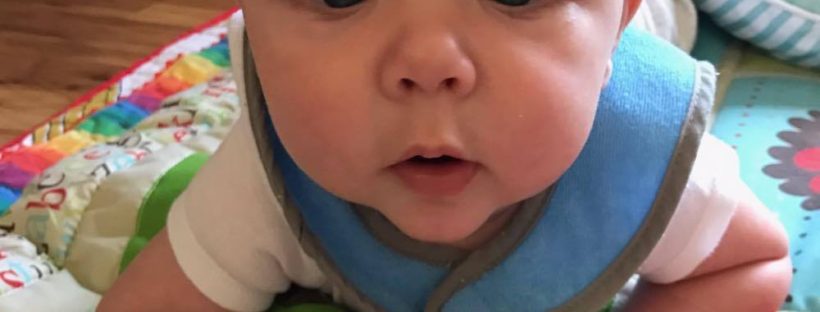
Hunter, thriving from combination feeding
#FedisBest
For more information on how to protect your baby from feeding complications due to early exclusive breastfeeding, please read and download the Fed is Best Feeding Plan, a way to communicate your feeding choices to your health care providers.
In addition, please read and download the Fed is Best Weighing Protocol to prevent newborn dehydration and failure to thrive.
Lastly, for more detailed information, please watch our educational videos on Preventing Feeding Complications.
Our full list of parent resources can be found on our Resource Page.
As a primary care Nurse Practitioner student and long time Registered Nurse, I always asks mothers if they plan to breastfeed at prenatal appointments. When they say ‘I don’t know’ or ‘I don’t think so’ I really encourage them to try after delivery. I explain that colostrum contains lots of good nutrients and antibodies for babies. I then always tell moms that I don’t care how they feed there baby after that as long as they feed them!! I see both views. I understand that breast feeding has many benefits for mothers and babies but I also recognize that each person is individual and, they should be respected and supported individually based on the baby and mothers needs.