My son, Harrison, was born 8 weeks ago at a Hospital in Fredericksburg, Va. He decided it was time to meet mom and dad two weeks before his due date and was born via C-section after 22 hours of labor. At birth he was 8 pounds 2 ounces and 21 1/2 inches long.
Before giving birth, my husband and I took every class the hospital offered. We took the two hour infant CPR class, nine hour childbirth class, three hour bringing home baby class, and three hour breastfeeding class. As first-time parents, we were filled with nervous excitement. Harrison is our miracle baby. I went through fertility treatments because PCOS and hyperthyroidism made it impossible for me to get pregnant without medical intervention.
After the unplanned C-section I was in no shape to help with Harrison’s care. The sweet nurses spent time with my husband and showed him how to diaper and swaddle. When it came time to breastfeed, Harrison latched right away and fell asleep soon after.
This continued for 12 hours and I started to become concerned. A lactation consultant was making the rounds and stopped in to check on us. I told her I didn’t think Harrison was actually eating or that I was producing anything. She specifically asked if I had PCOS and said that having that condition could affect my milk production. A few minutes later, she sent in another consultant to hook me up to a pump.
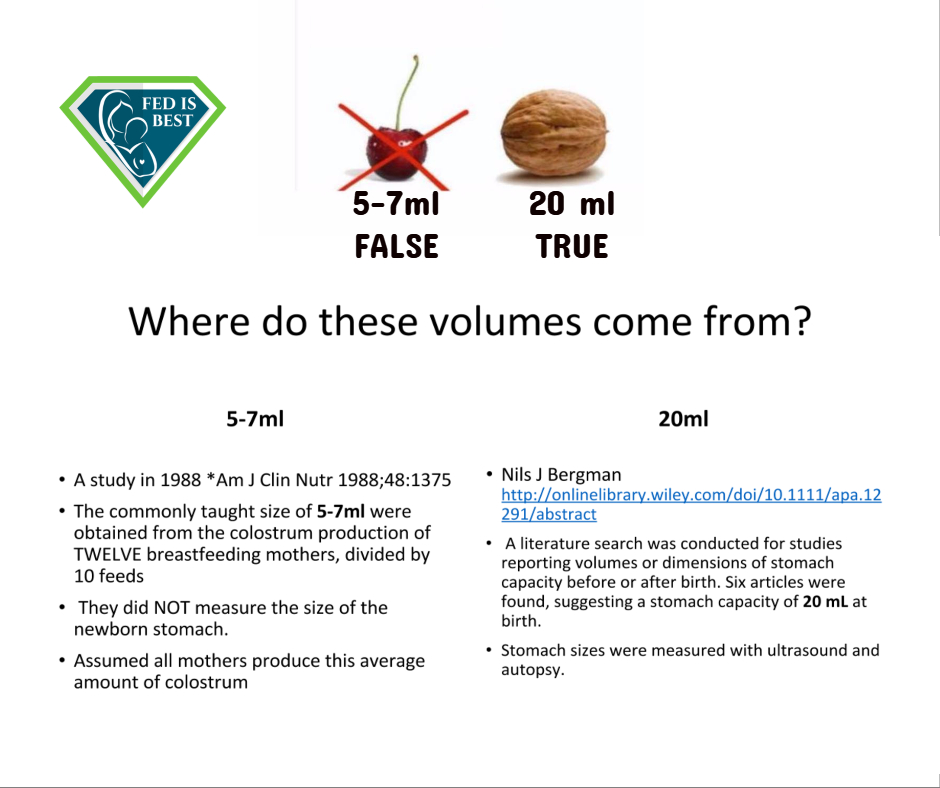
I pumped for 20 minutes and got droplets. The other consultant assured me this was enough to feed my eight pound baby. This was Thursday.
On Friday afternoon my husband left the hospital to install the car seat, set up the bassinet, and buy a few things at Target. I was left alone for the first time since Harrison’s birth. Harrison was born at 10:35 a.m. on Wednesday, so by midday on Friday he was really starting to get hungry. Knowing I wasn’t producing milk and that my baby hadn’t eaten, I started to cry—a lot. A nurse came in and asked what was going on. I explained that I didn’t think Harrison was getting any milk. She sent in a lactation consultant.
I asked the lactation consultant for formula to supplement, but she didn’t give me any. She said to keep trying to breastfeed because I was able to produce droplets the day before and she put me on a pumping regimen.
We left the hospital Saturday afternoon. Harrison was jaundiced and had lost 10% of his birth weight. He hadn’t eaten yet in his life and I still had no milk. We got home and I continued to breastfeed him every two hours. He’d latch, then fall asleep. My husband would try to wake him up and then hand him back to me to feed. The cycle would continue for an hour. Then we took an hour off and tried it again. At this point Harrison didn’t want to latch any more.
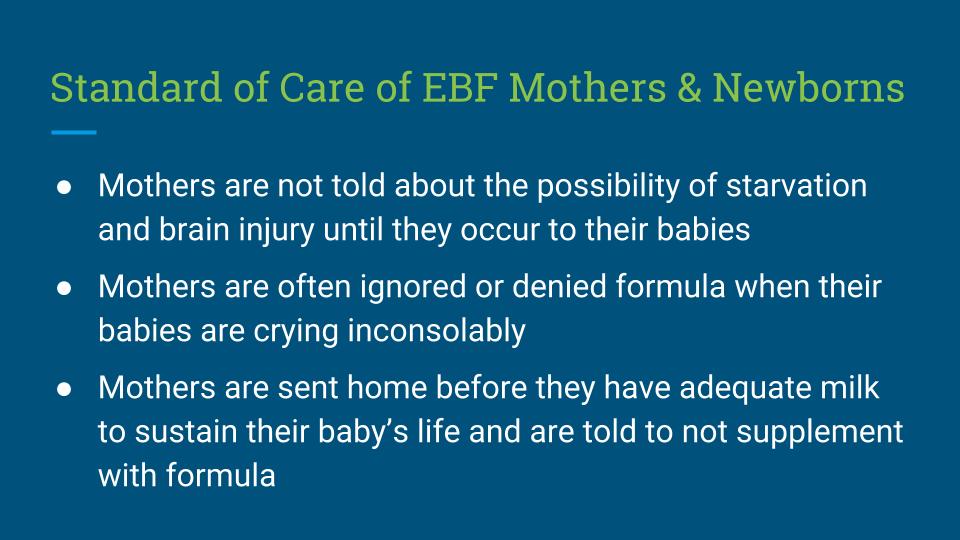
On Sunday morning around 2 a.m. Harrison woke up crying hysterically. He had enough of starving. He cried for hours and refused to latch. My husband got the sample of ready-made formula and gave it to him. I finally saw relief in Harrison’s eyes. It was a relief to me as well—but it was also heartbreaking. I knew, for a fact, that it was the first time he had nourishment of any kind. It was Sunday. He was born that past Wednesday.
I didn’t give up on my breastfeeding goal. I tried to breastfeed Harrison at each feeding. He’d latch and then fall asleep or he wouldn’t latch at all. I started giving him two ounces of ready-made formula after offering him the breast and he would consume the entire bottle. After he ate I pumped for 30 minutes. My highest amount of milk was 20 milliliters for both breasts.
That night I couldn’t sleep. I was convinced Harrison had severe jaundice. In the morning, we went to the pediatrician who ordered blood tests. The results showed that his jaundice was going down since I started giving him formula and his weight began increasing.
We went to see the lactation consultants eight days after Harrison was born and spent two hours with them. They said that Harrison wasn’t eating because he had a tongue tie (he didn’t) and his jaundice was making him lethargic. They again acknowledged that my PCOS may cause me to not produce milk, but kept coming back to the fact that there was something wrong with Harrison. Then they weighed him before and after nursing. There was no change in weight. I again asked how to correctly supplement with formula while my milk “came in.” They said I should stay on the same triple feeding regimen. They never told me to see my pediatrician, but gave me a book and a cookie recipe.
I continued with the pumping regimen for two more weeks. I cried while I pumped. I felt like a complete failure. I was connected to a pump and my supply was getting even lower. I couldn’t do the most fundamental thing that a mother does. My husband finally convinced me to stop. Once I gave up the idea that I had to breastfeed to be a good mother, the crying stopped. Harrison was back to his birth weight by the second week. By the end of his first month, he was a full pound heavier. He’s a happy, beautiful little boy. I’m a good mom and my husband is a wonderful dad.
Looking back on my experience, I can identify the short comings that nearly landed my baby back in the hospital:
(1) My OB-GYN never telling me that PCOS could affect my ability to breastfeed,
(2) The breastfeeding class never addressing the signs that supplementing needed to occur.
(3) The lactation consultants not giving me formula, attempting to convince me that my milk was going to come in, and worrying me that my little boy—who was getting healthier every day because I was feeding him formula—was really sick.
I spoke to a friend who is a second year resident at another hospital. The other day he had a new mom bring her eight day old into the ER. The baby was suffering from dehydration and was hours from seizing. This wasn’t neglect. It was a mom who was convinced that she was doing what was best for her child—breastfeeding. That baby could easily have been Harrison if I had followed the advice of the lactation consultants. Thank goodness I followed my instincts instead.

HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and every thing in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop and Fed is Best Foundation will earn cash back! We hope to develop our online safe infant feeding classes with these funds.
Thank you so much from the Founders of the Fed is Best Foundation!
YOU ARE NOT ALONE! The exact same thing happened to me except I went almost 2 weeks only breastfeeding. At first, my son was gaining weight and I thought everything was going well but he slowly started to get jaundice. I spent hours on the phone with a lactation consultant and was so scared to supplement him. Up until my second week with him I had not pumped I had only given him the breast. Finally, when I tried pumping to see how much I was producing, I pumped for 30 mins and did not even get a half ounce of breast milk. That was enough for me to realize my son was starving and I immediately grabbed the formula sample out of the closet. I kept trying to pump but it would just upset me everytime because I was seeing how little I was producing. Finally, I traded the pump in for a baby brezza formula pro and IT HAS BEEN THE BEST THING FOR MY SON. Thanks to formula he was able to grow into a healthy little guy. He was 6lbs when I had him and now at 7 months he is 21lbs!!!! THANK YOU FORMULA!!!!!
I was a NICU nurse for many years, now I am working in a postpartum unit in a baby friendly hospital. Couple of weeks ago I told a mother after 24h that maybe she should supplement, her son had lost over 6% of body weight in the first 24 hours, he was getting frantic. I was happy telling her that than bumping into her and finding out something was wrong with him. She was not getting anything when she pumped and nothing when she hand expressed. Told her to keep pumping for the next week, get some fenugreek and mothers milk tea. Don’t know what happened but he was so calm afterwards
I don’t want to discount this mother‘s experience at all but this could not be further from my experience at Mary Washington hospital. I did not deliver my son at Mary Washington but I did go to MW to see the lactation consultants multiple times during the first few weeks after my third child was born. I always have a horrible time in the beginning trying to get my babies latched. I have an oversupply so massive engorgement prevents a tiny newborn mouth from being able to get a good latch and I always end up with clogged ducts and bleeding nipples. When I went in, they taught me how to create a good pumping schedule to keep my supply up and make sure he was fed. It was also suggested he might have a lip tie or tongue tie. I visited an ENT, and my son did in fact have a severe lip tie as well as an anterior and posterior tongue tie which ended up being surgically corrected. At the same LC appointment, we talked about a noise that my son was making while breathing and it suggested that he might have laryngomalacia. The ENT also found this to be true and my son was put on reflux meds which helped tremendously. I was warned by the ENT that sometimes even after correction, babies with lip/tongue ties don’t always figure out how to latch. With all these things stacked against us and my postpartum depression, I was ready to quit trying to nurse. Sometimes as moms, we feel like we need “permission” to stop trying to do something that we think we are “supposed” to do. During my multiple appointments, my LC let me know that she would help me no matter how I chose to feed my son. She said she could help us continue trying to latch, or teach me how to exclusively pump, or if I need her to be the person who told me it was “okay” to use formula, she would be that person for me. I eventually decided to exclusively pump while attempting to keep trying to latch occasionally. She lent me her own personal hospital grade breast pump free of charge for 6 months. My son finally learned to latch at 4 months and is now nursing exclusively at 7 months and I don’t know how to thank the Mary Washington LC Team enough…not just because they helped me finally establish the nursing relationship I wanted to have with my son, but because in the beginning when I was literally drowning in postpartum hormones and depression, my wonderful LC let me know that a fed baby is best and a happy healthy Mom is important too.