First of all, I had always seen your Facebook page and thought to myself “this could never happen to me” or “I wouldn’t be that naive.” But now, can I share my story?
I was induced at 39 weeks due to preeclampsia. Since my cervix was stubborn, however, I ended up with a c-section. My baby was born 7 lbs 11 oz on January 10, 2018.
I was hooked up to magnesium to help with my blood pressure and was bedridden for 24 hours after the c-section. My hospital was a BFHI-certified hospital, and they bragged about their excellent lactation consultants (IBCLCs). That made me happy because I had always dreamed of breastfeeding. I never imagined how hard it would be.
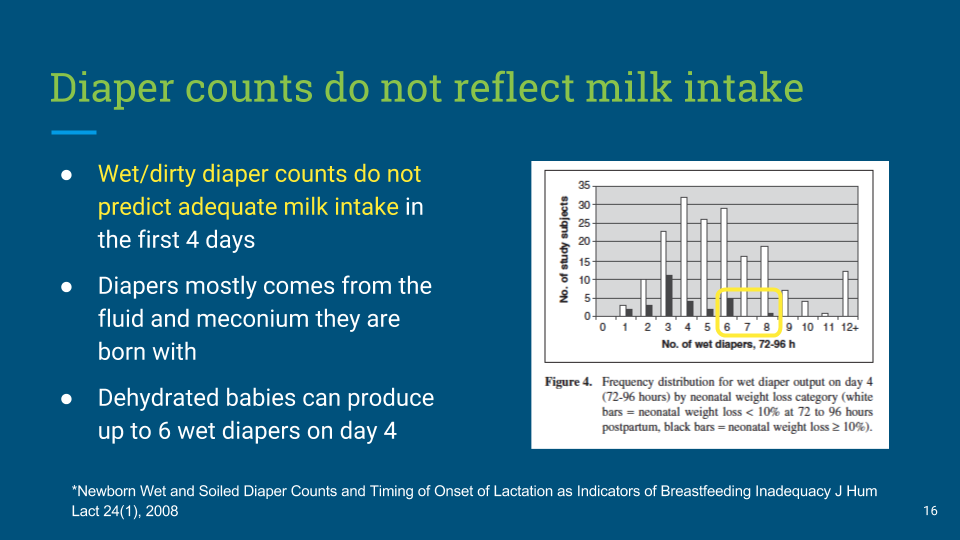
I was recovering from major surgery and felt weak, overwhelmed and quickly became frustrated trying to take care of my baby and breastfeed her. I cried multiple times during my short stay. Why was this so hard? I constantly had to ask for breastfeeding help from the nurses and lactation consultants. By the end of the second day, though, I was proud I got my baby to breastfeed without help. She was constantly feeding, every hour on the dot. No one was concerned about her excessive breastfeeding at all. The nurses seemed pleased with her diapers counts.
We were discharged from the hospital not even 48 hours after my c-section. The first night with my baby was unbearably tough. If she wasn’t breastfeeding, she was crying. This was not fussing. She cried and screamed and the only way she stopped crying was if she was on my breast. My mom stayed by my side most of the night trying to help soothe her, but my baby only wanted to be on my breast.
I knew something was wrong, and I called the pediatrician first thing in the morning. We took the first appointment available, and watched as our little girl finally succumbed to the sheer exhaustion of frantic crying and fell asleep.
The doctor checked her out, and besides her losing 9.8 percent of her birth weight, he was not concerned. We changed a very dirty diaper at the appointment. I told him I had witnessed her peeing the night before as well. He said our little girl looked hydrated. He told us to come back the next day just to be safe, but my milk should be there any second. He never told me to supplement my baby.
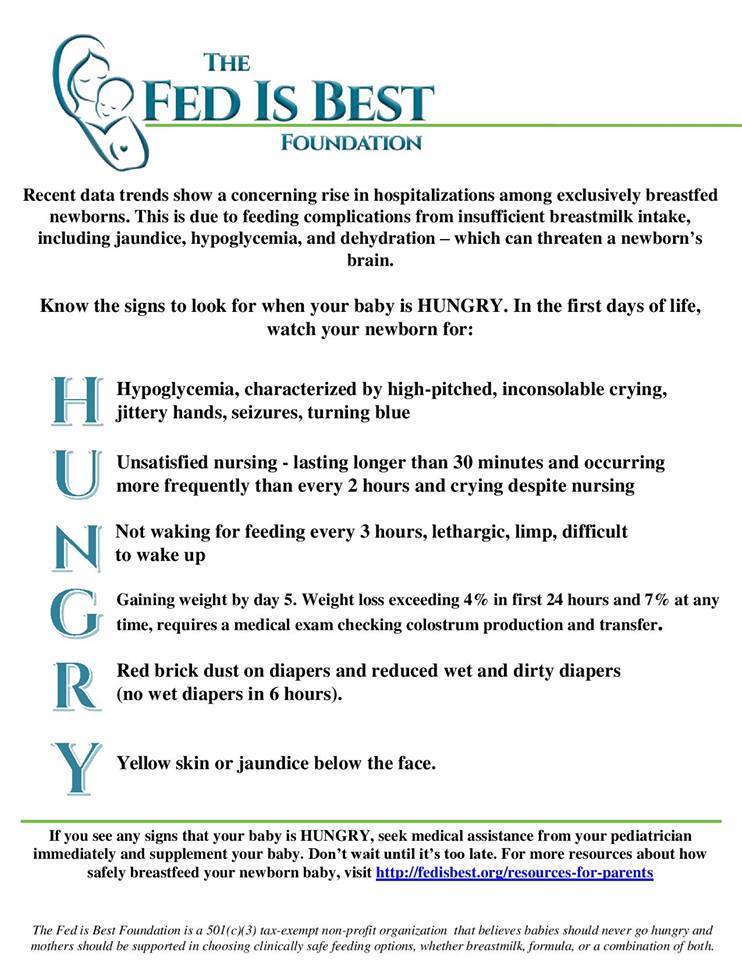
The current guidelines by the American Academy of Pediatrics (AAP) now recommends a weight loss threshold of 7%, as the weight at which the feeding of the baby should be evaluated in order to ensure that they do not lose more weight. Weight loss is associated with dangerous conditions like pathological hyperbilirubinemia (jaundice), dehydration, hypoglycemia (low glucose) and hypernatremia (high sodium). All of those markers can be signs of underfeeding and hunger in the newborn.
I nursed her as soon as we got home and we both slept for three hours. When I woke up, I went to check on her and tried to wake her up to nurse. But she just screamed and would not latch. I broke down and sent my husband to the store to buy formula as I knew she needed to eat.
Not even ten minutes later, my precious, three-day-old baby went limp and turned blue. My mom started trying to revive her as I panicked and called 911. Thankfully as my mom tilted her chin back, she let out a wail. The ambulance arrived a few minutes (but felt like hours) later.
She was rushed back to her birth hospital not even 24 hours after we left. Her blood sugar was only 22, which is dangerously low, and I almost lost my sweet girl. When I heard her blood sugar, guilt and grief overwhelmed me. I could not believe my baby girl was starving. I felt like the worst mom ever knowing I hadn’t been sufficient enough.
She was then transferred to a larger hospital where she spent three days in the NICU getting her blood sugar and electrolytes stabilized. My heart broke to see my baby hooked up to IVs and monitors in the intensive care when only two days earlier she was born perfect.

Everyone kept telling me I was all she needed. I thought I failed her. Instead, the BFHI protocol failed us.
There, in the Children’s Hospital NICU while her health providers were fighting to stabilize her, I learned how common it was for the unit to get accidental starvation admissions of exclusively breastfed babies, just like mine. These babies do not get enough colostrum. The doctors and nurses in the NICU told me over and over that it wasn’t my fault. They showed me how to pump; they had us take an infant CPR class. My milk finally came in on the day we were being discharged—a full six days after my baby was born.

Now my daughter is two-weeks old and over her birth weight. We tried breastfeeding again, but she refuses to latch. I’m coming to terms with that. A fed baby is the best baby. She is a different baby now, and she hardly ever fusses. We adore her so much.

However, I’m still struggling with the guilt and the feeling of failure.
- I regret not self expressing or pumping in the hospital to see if I was making any colostrum (the BFHI hospital discouraged me from doing so).
- I regret not noticing sooner that she was starving.
- I regret being so anxious to leave the hospital after my c-section; if we had stayed one more night, maybe this wouldn’t have happened.
- The greatest feeling I have, though, is betrayal; accidential starvation while attempting to exclusively breastfeed is “common”, and I was not told this, nor was I given any warning signs to watch for.
- It is not talked about and families are not educated about the signs at the hospital. Breastfeeding advocates and BFHI-hospitals are so determined to portray breastfeeding as “perfect” and “natural” that they deny life saving information to families.
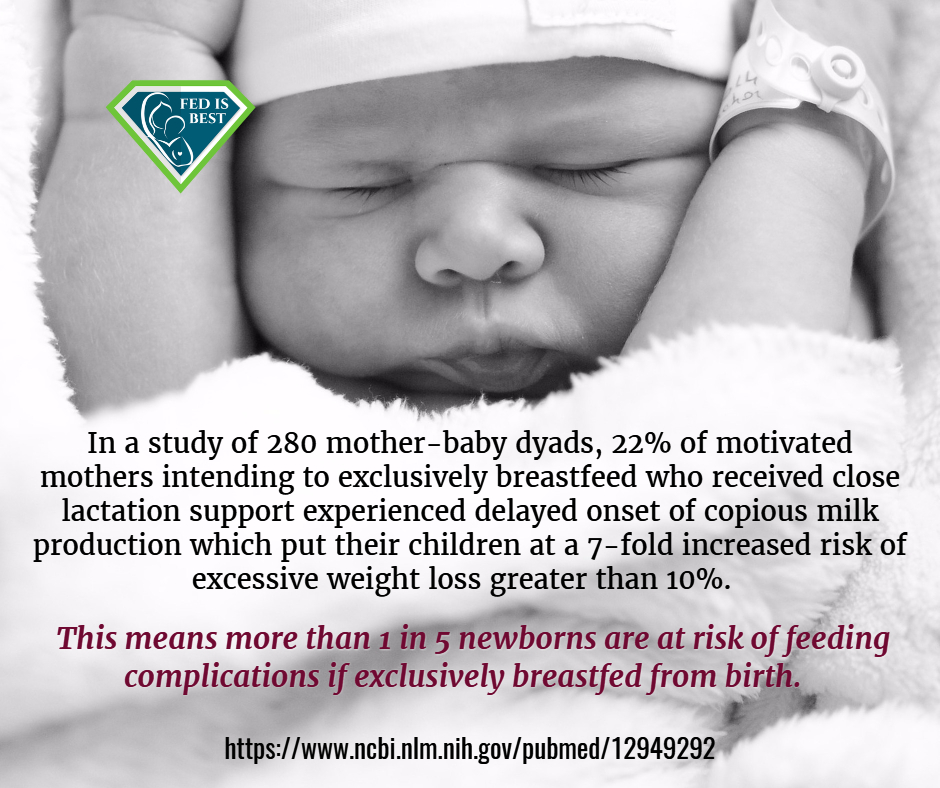
I am haunted still by the moment when she turned blue in my lap. Sharing my story helps me to cope. I don’t want any other parent to watch their newborn suffer and almost die from hypoglycemia. I wish every EBF baby would be required to get a glucose check before they leave the hospital and at their first appointment, especially when losing too much weight. Being a first-time mom, I wanted to do everything right. Now I know the public health policy of breastfeeding being “right” isn’t best for everyone, and my daughter was the victim of a flawed public health policy.

HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and every thing in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going. Thank you for your advocacy!

2 thoughts on “My Three Day Old Baby Went Limp And Turned Blue; She Was Starving And I Almost Lost Her”