Christie del Castillo-Hegyi, M.d.
Newborn hypernatremia is a serious complication of early exclusive breastfeeding of newborns caused by insufficient feeding of milk. It is defined as an elevation of blood sodium levels (≥ 145 mEq/L) in response to insufficient fluid intake and most commonly occurs at day 3-4 of life, typically the point of greatest weight loss of a newborn. It is the most severe complication of dehydration and excessive weight loss and increases the risk of brain injury, developmental delay/disability, seizure disorder, vital organ injury and death. Oddie et al. showed that up to 98% of hypernatremia occurs in exclusively or near-exclusively breastfed newborns and the study group found the diagnosis of hypernatremia was rare.[1] However, since blood sodium levels are not universally-screened, which could result in missed cases of hypernatremia, it has been unclear just how common the condition is among newborns.

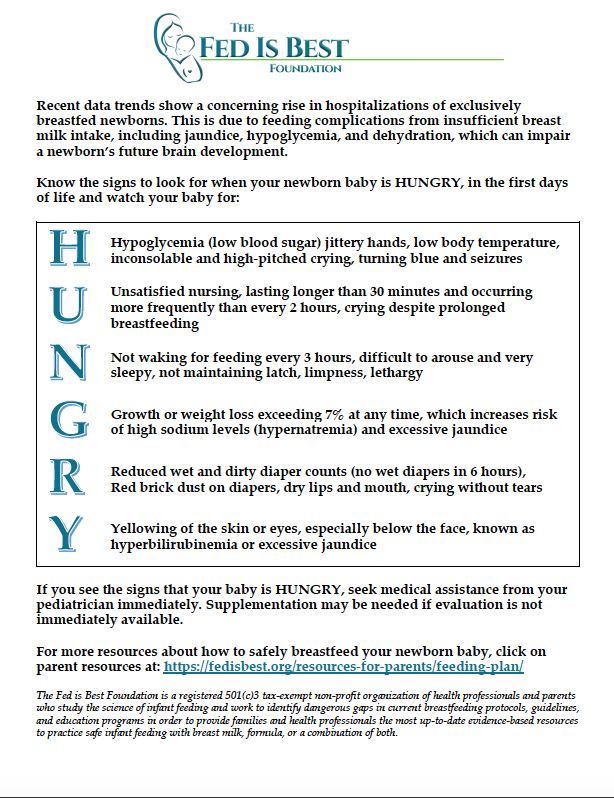
Steph Montgomery’s daughter jaundiced, dehydrated and hypernatremic at day 5 with 20% weight loss due to insufficient breast milk intake from low supply
A recently published prospective study of 165 healthy newborns ≥ 35 weeks gestational age looked at rates of hypernatremia (>145 mEq/L) in the first 3 days of life.[2] They examined multiple variables that predict hypernatremia as well as the threshold weight loss values at which increased hypernatremia risk occurs. The results were astounding.
The study found that out of 165 newborns 51 or 30.9% developed hypernatremia.
The majority of cases occurred by 5% weight loss, the lowest percentage weight loss occurring at 4.77% weight loss, especially for male infants delivered by cesarean delivery to a mother with higher education level.
The study found that the variables that predicted higher odds of developing hypernatremia were the following:
| Risk Factors for Hypernatremia | Increased Odds of Newborn Hypernatremia |
| Greater weight loss (mean 8.6%±2 vs. 6%) |
70% |
| Male gender |
192% |
| Higher maternal education |
86% |
| Multiparity (not being a first-time mom) |
263% |
| Cesarean delivery |
39% |
Hypernatremia is a known complication of newborn weight loss and male newborns may be at higher risk due to a higher metabolic requirements relative to females. Surprisingly, although primiparity (being a first-time mom) is a risk factor for delayed or insufficient lactogenesis II,[3] multiparity in this study was a risk factor. The authors hypothesized that first-time mothers may have received closer monitoring. They also found that high maternal education was a significant risk factor for neonatal hypernatremia as mothers with higher education are more likely to exclusively breastfeed.
Analysis of the data shows that the majority of hypernatremic babies were breastfed or mix-fed. It is unclear whether the volumes of supplementation were restricted in mix-fed newborns or if they started off as exclusively breastfed and subsequently met medical indication for supplementation since the data was collected right before discharge. 96.1% of hypernatremic newborns were breastfed, 74.5% exclusively breastfed, 21.6% mix-fed and 3.9% were exclusively formula-fed. Exclusively breastfed and mix-fed newborns had hypernatremia rates of around 37% while exclusively formula-fed newborns had a rate of 6.25%. This yields a 5.84-fold higher risk of hypernatremia for exclusively breastfed newborns relative to exclusively formula-fed newborns. Mixed-fed newborns (which may have included exclusively breastfed newborns who required supplementation before discharge) were at 6-fold higher risk of hypernatremia.
| Feeding Method (FM) | FM among hypernatremic newborns (% of total) n = 51 | Risk of hypernatremia per FM: hypernatremia cases/total (%) |
| Exclusively breastfed |
38 (74.5%) |
38/104 (36.5%) |
| Mixed-fed (upon discharge) |
11 (21.6) |
11/29 (37.9%) |
| Exclusively formula fed |
2 (3.9%) |
2/32 (6.25%) |
This is the first study done to show the true incidence of hypernatremic dehydration among healthy term and near-term newborns. This is alarming data as prior studies have concluded that hypernatremic dehydration is rare occurring to less than 2% of admitted newborns.[4] Other studies have shown abnormal developmental scores among newborns who develop hypernatremia even with appropriate correction. Among them include a study showing newborns who developed hypernatremia ≥ 150 mEq/L, over half had abnormal developmental scores at 12 months of age.[5] Another showed 25% percent of newborns with hypernatremia had developmental delay at 6 months, 21% at 12 months, 19% at 18 months and 12% at 24 months of age compared to a rate of 0.3% for non-hypernatremic infants.[6]
The largest study to date of weight loss in healthy, term exclusively breastfed newborns at a large Baby-Friendly-certified health system showed that greater than half lost > 7% of birth weight.[7] Ten percent weight loss is still commonly viewed as “normal” and “safe” for newborns to lose with little to no data supporting it. Among hypernatremic newborns, the mean weight loss was 8.6% +/- 2.7. Given that blood sodium levels are not universally-screened, a true hypernatremia incidence of 31% (36-38% among breastfed newborns) predicts that many more cases of hypernatremia are left undiagnosed and untreated potentially resulting in occult brain injury. The signs of hypernatremic dehydration predicting poor outcomes are poor feeding, seizures, fever and lethargy.[6] Given that the signs of poor feeding can be subtle and commonly missed among health professionals (or even normalized by the BFHI guidelines)[8] and given that parents are given little to no education on the signs and consequences of hypernatremic dehydration, there are likely many cases of hypernatremia among breastfed newborns that are being missed resulting in cases of brain injury that could go undetected for several years until a child begins to miss developmental milestones.
Summary
The recommendation of the author was to screen for hypernatremia at weight loss cut-offs depending on a newborn’s risk factors. For the highest risk category of males born by c-section to a multiparous, highly educated mother, it was recommended to begin screening for hypernatremia at 4.77% weight loss.
Hypernatremic dehydration is a devastating unintended consequence of current initiatives aimed at increasing exclusive breastfeeding rates at discharge, the quality metric of the Baby-Friendly Hospital Initiative. Given the high incidence of hypernatremia among healthy, term and near-term newborns, particularly among exclusively or near-exclusively breastfed newborns before copious milk production, we recommend screening for hypernatremia above 5% weight loss and sooner among high-risk newborns who are exhibiting signs of persistent hunger and distress. Unrestricted supplementation for mild hypernatremia (145-146 meQ/L) can prevent need for hospitalization and the negative consequences on subsequent brain development.
References
- Oddie, S. J., Craven, V., Deakin, K., Westman, J. & Scally, A. Severe neonatal hypernatraemia: a population based study. Arch. Dis. Child. Fetal Neonatal Ed. 98, F384-387 (2013).
- Ferrández-González, M. et al. Weight loss thresholds to detect early hypernatremia in newborns. J Pediatr (Rio J) (2018).
- Dewey, K. G., Nommsen-Rivers, L. A., Heinig, M. J. & Cohen, R. J. Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics 112, 607–619 (2003).
- Moritz, M. L., Manole, M. D., Bogen, D. L. & Ayus, J. C. Breastfeeding-associated hypernatremia: are we missing the diagnosis? Pediatrics 116, e343-347 (2005).
- Koklu, E. et al. A review of 116 cases of breastfeeding-associated hypernatremia in rural area of central Turkey. J. Trop. Pediatr. 53, 347–350 (2007).
- Boskabadi, H. et al. Long-Term Neurodevelopmental Outcome of Neonates with Hypernatremic Dehydration. Breastfeed Med (2017). doi:10.1089/bfm.2016.0054
- Flaherman, V. J. et al. Early Weight Loss Nomograms for Exclusively Breastfed Newborns. PEDIATRICS 135, e16–e23 (2015).
- Kellams, A., Harrel, C., Omage, S., Gregory, C. & Rosen-Carole, C. ABM Clinical Protocol #3: Supplementary Feedings in the Healthy Term Breastfed Neonate, Revised 2017. Breastfeed Med 12, 188–198 (2017).
- Ben, X.-M. Nutritional management of newborn infants: Practical guidelines. World Journal of Gastroenterology 14, 6133 (2008).

One thought on “Hypernatremic Dehydration is Common and Occurs to a Third of Healthy Newborns”