We know everyone’s anxiety level is very high right now because of the uncertainly of delivering your baby during the COVID-19 pandemic. Our goal is to provide real-life experiences of nurses who are taking care of people in labor and postpartum so that parents can have an idea of what to expect when delivering their babies.
The most recent guidelines released by the AAP, CDC, and ACOG apply to babies in the U.S.A.
Since these guidelines are different from the WHO guidelines and parents have been receiving mixed messages and are asking for clarification. We want to clarify the recommendations for parents so they can be fully informed of their choices. Generally speaking, parents who live in developed countries such as the USA have access to breast pumps, clean water, masks, cleaning supplies, and formula. The science-based recommendations are based on these choices.

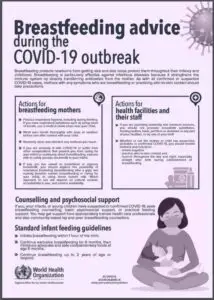
WHO COVID-19 Guidelines
AAP Guidelines: Rooming-in for mothers and well newborns: While difficult, temporary separation minimizes the risk of postnatal infant infection from maternal respiratory secretions. If possible, admit the infant to an area separate from unaffected infants, and wear gowns, gloves, eye protection goggles and standard procedural masks for newborn care.
If the center cannot place the infant in a separate area — or the mother chooses rooming-in despite recommendations — ensure the infant is at least 6 feet from the mother. A curtain or an isolette can help facilitate separation.
AAP Key Points:
• Current evidence is consistent with low rates of peripartum transmission and is
inconclusive about in utero transmission of SARS-CoV-2 from mothers with COVID-19 to their newborns.
• Neonates can acquire SARS-CoV-2 after birth. Their immature immune system leaves newborns vulnerable to other serious respiratory viral infections, raising concern that SARS-CoV-2 may cause severe disease among neonates.
• Airborne, Droplet, and Contact Precautions should be utilized when attending deliveries from women with COVID-19 due to the increased likelihood of maternal virus aerosols .and the potential need to administer newborn resuscitation to infants with COVID-19 infection that can generate virus aerosol
• When the physical environment allows, newborns should be separated at birth from mothers with COVID-19. Families who choose to have their infants room in with the mother should be educated on the potential risk to the newborn of developing COVID-19.
• SARS-CoV-2 has not been detected in breast milk to date. Mothers with COVID-19 can express breast milk to be fed to their infants by uninfected caregivers until specific maternal criteria are met.
• Infants born to mothers with COVID-19 should be tested for SARS-CoV-2 at 24 hours
and, if still in the birth facility, at 48 hours after birth. Centers with limited resources for testing may make individual risk/benefit decisions regarding testing.
• A newborn who has a documented SARS-CoV-2 infection (or who remains at risk for postnatal acquisition of COVID-19 due to inability to test the infant) requires frequent outpatient follow-up via telephone, telemedicine, or in-person assessments through 14 days after discharge.
• After hospital discharge, a mother with COVID-19 is advised to maintain a distance of at least 6 feet from the newborn, and when in closer proximity use a mask and hand-hygiene for newborn care until (a) she is afebrile for 72 hours without use of antipyretics, and (b) at least 7 days have passed since symptoms first appeared.
• A mother with COVID-19 whose newborn requires ongoing hospital care should
maintain separation until (a) she is afebrile for 72 hours without use of antipyretics, and(b) her respiratory symptoms are improved, and (c) negative results are obtained from at least two consecutive SARS-CoV-2 nasopharyngeal swab tests collected ≥24 hours apart.
Nurse Amanda talks about how she took care of a laboring mother who was COVID-19 positive:
“I am pleased to report that the care given to laboring patients with COVID-19 is not much different, except that everyone (including the mother’s support person) is masked with an N95 mask and protected with gowns, goggles, face shields, and gloves; this is to protect ourselves, other patients on the unit, and the baby after birth. This mother was experiencing significant shortness of breath, fatigue, and body aches from COVID-19. After her vaginal birth, the baby was placed in an isolette in the delivery room to stabilize, and parents were able to see their baby the entire time. The baby was then taken to a private special care room in our nursery area, fed donor milk, and bathed. The baby remained there with 1:1 nursing care and was monitored and assessed every three hours. The parents had access to a 24/7 video camera to see their baby, and a tablet was used for constant communication. It was very reassuring to the parents to see that their baby was being well cared for, which reduced their separation anxiety.
The mother desired to breastfeed, and her colostrum was hand expressed by the nurse after cleansing her breasts using sterile technique. It was delivered to her baby in a sealed plastic bag. Since this mother wasn’t producing enough colostrum, the baby was supplemented with donor milk.
The family was discharged home at 36 hours with specific instructions about taking the baby’s temperature every 8 hours, keeping the baby six feet away from the mother, how to pump according to the CDC guidelines and having the father take care of the baby. They were followed daily by a public health nurse and their pediatrician.”
Nurse Katie SAYS:
“In our hospital, every mother who is COVID-19 positive will have their own specific needs according to her unique circumstances. We practice according to the AAP/CDC guidelines for the best outcome, while supporting the mother’s wishes. The COVID-19 positive mother I took care of had mild symptoms, and she wanted to breastfeed. We discussed how to directly breastfeed while protecting her baby. After her baby was born, she wanted the baby placed on a warm blanket that was placed on her chest to protect her from droplets on her skin while pushing. She wore an N95 mask and also wanted to wear gloves while breastfeeding. After the baby was fed, she was bathed and kept in the mother’s room; however, she was placed on the other side of the room with her father caring for her. “
Nurse Monica says:
“If an asymptomatic mother comes in, she is allowed one support person. We keep the support person in the room and provide them with meals. The entire staff wears surgical masks during the entire shift. If those patients/support persons leave the room, they must wear masks. If they leave the hospital, they won’t be readmitted. We are discharging mothers who had vaginal births at 24 hours and c-sections at 36–48 hours, as long as they have good follow-up care scheduled for the baby. For COVID-19 positive or PUIs [persons under investigation who may be positive], unfortunately, no support person is allowed. We are wearing full PPE with N95s with all contact. We keep the IV pump outside the door and communicate mostly through telephone. Epidurals are given early. Mother and baby are separated at birth. We encourage pumping. Neonatologists determine when babies will be discharged. The mother goes to the COVID floor if she needs medical management after delivery. “
Nurse Miranda says:
“I took care of a COVID-19 positive mother who was readmitted 2 days after her delivery because she required intensive respiratory support. She was able to pump to manage her engorgement and she dumped her milk. She did not want to take any chances with contamination during collection and storage while in the hospital environment. Her intention was to protect her milk supply while she recovered so that she could breastfeed her baby. Her partner was at home caring for their baby.”
ACOG Breastfeeding and formula feeding— It is unknown whether the virus can be transmitted through breast milk. The only report of testing found no virus in the maternal milk of six patients [48]. However, droplet transmission could occur through close contact during breastfeeding. A potential benefit of breast milk is that it may be a passive source of antibody protection for the infant.
In mothers with confirmed COVID-19 or symptomatic mothers with suspected COVID-19, to minimize direct contact, ideally, the infant is fed expressed breast milk by another caregiver until the mother has recovered or has been proven uninfected, provided that the other caregiver is healthy and follows hygiene precautions. In such cases, the mother should use strict handwashing before pumping and wear a mask during pumping. The CDC has issued guidance about cleaning breast pumps and parts. If possible, the pumping equipment should be thoroughly cleaned by a healthy person.
If feeding by a healthy caregiver is not possible, mothers with confirmed COVID-19 or symptomatic mothers with suspected COVID-19 should take precautions to prevent transmission to the infant during breastfeeding (including assiduous hand hygiene and use of a face mask) [47,49,50].
Women who choose not to breastfeed must take similar precautions to prevent transmission through close contact when feeding the infant formula.
Every day new information is published, and we will keep all of the resources updated and available to keep parents informed. Please remember you have the final say about the way you want to feed your baby and will receive the appropriate support. If you are infected you will be making antibodies that will be in your breastmilk, but we don’t know how long it will take for the full passive antibody response to take effect. In the meantime, it’s imperative that you follow the guidelines described above when breastfeeding your baby.
Resources:
Guidelines for Pregnant and Breastfeeding Mothers During the Coronavirus Pandemic
AAP management of infants born to COVID-19 mothers
Up to date Coronavirus disease 2019 (COVID-19): Pregnancy Issues
https://pediatrics.aappublications.org/content/pediatrics/early/2020/03/16/peds.2020-0702.full.pdf?fbclid=IwAR1ms0J9bN42r0heQJvu1uCPwUzUOhPQ6U4T40Vs2xdTh-bZB81cBU8jjk8 Epidemiological Characteristics of 2143 Pediatric Patients With 2019 Coronavirus Disease in China
https://obgyn.onlinelibrary.wiley.com/doi/pdf/10.1002/ijgo.13146?fbclid=IwAR0nIVUfZ_HAMWQZUlCjjqQinnAJuaLNRldNub7yyW9FLGsfcMZbnBMR36c Expert consensus for managing pregnant women and neonates born to mothers with suspected or confirmed novel coronavirus (COVID-19) infection
WHO Q&A on COVID-19, pregnancy, childbirth and breastfeeding
https://www.nature.com/articles/s41591-020-0843-2?fbclid=IwAR14RqyqrRtEeZgQCYNT8IM3bNGQ6j0uF9y_EkBbBium5Jt_QWhKYehMD2w Brief CommunicationRespiratory virus shedding in exhaled breath and efficacy of face masks
https://jamanetwork.com/journals/jama/fullarticle/2763854?utm_source=facebook&fbclid=IwAR2KTOPf4HvYGvl_-ie2MDNrcnEnW5ga7Y01wjzpKZfrP4fWJGxMqRzlkAw Antibodies in Infants Born to Mothers With COVID-19 Pneumonia
https://www.nejm.org/doi/full/10.1056/NEJMc2007605?query=TOC&fbclid=IwAR0omwQoUwDNQBZO8cXa8BZU0dmy-M_NPFaqtLHSjroEo28KMGUVXbY8FkE Outcome of Coronavirus spectrum infections (SARS, MERS, COVID 1 -19) during pregnancy: a systematic review and meta-analysis
https://www.aappublications.org/news/2020/04/02/infantcovidguidance040220?fbclid=IwAR00V2zvgO4h6HCIzuLV0BCfgVh_-hKyuohD6wO5ZQzCFOPaOrw6XduWH4Q Care of the COVID mother/baby that follows AAP guidelines, including recommending separation of mother and baby.
