by Jody Segrave-Daly, Veteran NICU/Nursery nurse, IBCLC retired and Cofounder of the Fed Is Best Foundation
The standard of care for most hospitals, especially those who are Baby-Friendly certified, is that mothers stay with their baby after birth in their room, 24 hours a day, which is known as rooming-in.
Baby Friendly’s recent blog says that mothers have choices about nursery care in their Baby-Friendly certified hospitals; but then they say babies SHOULD stay in the room, no matter how they are being fed. This statement gives parents mixed messages and implies they don’t really have a choice at all. In many hospitals, it is not just implied; nurseries have been eliminated outright.
“Regardless of whether a mother is breastfeeding or formula feeding, they should room-in with their newborn.”
According to the World Health Organization, rooming in began as a way to promote early breastfeeding and to encourage bonding. Step 7 of the Ten Steps to Successful Breastfeeding calls for hospitals to “enable mothers and their infants to remain together and to practice rooming-in 24 hours a day.”
Despite the WHO’s 2017 expert panel’s finding that 24/7 rooming-in was ineffective at promoting sustained breastfeeding after discharge (but recommended it any way) and published tragedies of harmed infants while rooming-in, The World Health Organization and UNICEF continue to include rooming in for healthy newborns in the Ten Steps to Successful Breastfeeding policy.
Since adopting the rooming-in policy, inexcusable consequences such newborn falls from parent beds and near deaths and deaths from accidental suffocation while breastfeeding or doing skin-to-skin care (known as Sudden Unexpected Postnatal Collapse or SUPC) have skyrocketed, highlighting the urgent need for families to have access to nursery care.
What are the risks of rooming-in?
- Bed sharing and accidental suffocation
Mothers who bed share with their newborns and fall asleep have caused unintentional cases of infant near deaths and deaths from accidental suffocation, or SUPC. SUPC and is recognized globally as a serious risk to newborns in the immediate period after delivery. SUPC causes death in half of the cases, the majority of the remaining survivors sustaining oxygen-deprivation-related brain injury that results in long-term disability. Near misses are common; nurses frequently have to wake mothers (and partners) who have fallen asleep holding their babies. While unsafe-sleep-related deaths decreased initially in the 1990s after the Back to Sleep campaign promoted supine (or sleeping on their back) positioning for babies, these deaths have not decreased further. Prominent pediatrician safe sleep advocate Dr. Joel Bass has commented on the relationship between compliance with the Baby-Friendly Hospital Initiative and cases of SUPC. Safe sleep experts have noted that published risk factors for SUPC include the first two hours of life, prone (belly down) position of infant, skin-to-skin care, unsupervised breastfeeding during the first two hours of life, and maternal fatigue. Research tells us on average postpartum parents receive 4.4 hours of sleep a day yet hospitals are expecting them to be responsible for their baby at all times, while recovering from childbirth.
“When rounding, we find moms sleeping with their babies all the time, because the baby is fussy or mom is just exhausted and dozes off.”
– Kelli Arnette, NICU and mother baby nurse
- Accidental infant falls and drops
It has been estimated that 600 to 1,600 newborns in the United States experience an in-hospital fall every year, causing serious harm to the newborn and emotional distress to parents. Exhausted and recovering mothers and partners can fall asleep while holding their baby in bed resulting in unintentional drops to the floor.
- SUPC During Skin to Skin Care (SSC)
Skin to skin care is the practice of holding a mostly unclothed baby (except for their diaper) to the bare chest of the parent, which is thought to promote breastfeeding. There are potential dangers immediately after birth and throughout the postpartum hospital period when parents and babies do SSC while exhausted and not directly observed by a trained health professional to prevent SUPC.
Click here to learn “How to reduce the risk of Sudden and Unexpected Postnatal Collapse”
Repackaging the Rooming-In Policy
There is no other patient in the hospital who has undergone major abdominal surgery and is expected to take care of a new baby, who is another patient in the hospital.
What is unsafe is forcing mothers to keep their baby at the bedside when they are exhausted and in pain, unable to care for themselves, let alone their baby, under the false belief that mother–baby separation causes breastfeeding to fail.
– Kelli Arnette, NICU and mother baby nurse
In the blog, Dr. Feldman-Winter goes on to state that:
“[S]ome mothers have a ‘misperception of aloneness,’ believing incorrectly that they’ll need to fend for themselves and figure it all out on their own without support.” [our emphasis]
To counter this, Feldman-Winter argues,
“The reality is that the hospital staff is there to help the mom care for the baby in the room as much as needed. And if the mom is not able to care for the baby, including feeding, then a nurse can provide this care without separation.”
This quote demonstrates just how disconnected Baby-Friendly USA and Dr. Feldman-Winter are from the hospital stays that parents experience. With nurses sometimes taking care of four to six mother–baby dyads (in other words, 8–12 patients), this is absolutely not “the reality.” The reality is staffing ratios determined by hospitals severely limits the amount of time nurses can spend with each patient, which makes it impossible for a nurse to be available at every moment families need them. They are taking care of other families, too.
This places an unnecessary burden on new mothers who are recovering from childbirth. A person without continuous support from their partner or family, especially overnight, is vulnerable. Those who support them are exhausted themselves.
This framing of maternal reports of inadequate support under current rooming-in guidelines as a misperception is a perfect example of the gaslighting women often endure in the health care system. When are Baby-Friendly advocates going to stop accusing mothers of “misperceptions” and take seriously their feelings and accounts of their own experiences? An overwhelming number of mothers have said they feel alone in caring for their new baby while recovering from birth, often exhausted and in pain. Nurses widely validate their accounts since they are witnessing the same thing. Mothers aren’t misperceiving their experience. They feel alone because they often are alone, unless they have the privilege of 24/7 help from a family member. If they ask for nursery care, they are first “counseled” on the benefits of rooming-in before being given this service she has already deemed necessary. This counseling can come with veiled warnings that something biologically undesirable will occur as a result of her request like nipple confusion or breastfeeding failure. Take for instance, this quote:
“Moms are not supposed to be separated from their babies. It’s unnatural for mammals,” says Feldman-Winter. “When you remove a baby whale from its mother, for example, the mother whale emits a horrible guttural sound as though she’s dying.”
Let’s stop insulting women’s intelligence and stop using hyperbole (and natural fallacy) when framing a new mother’s plea for assistance when she is at highest risk of falling asleep with her new baby. Is a few hours of uninterrupted sleep too much to ask? When the science shows 24/7 rooming in has virtually no measurable effect on long-term breastfeeding, why are we torturing new mothers and putting newborn babies at risk? Furthermore, parents aren’t even given informed consent on the risks of infant falls, suffocation, brain injury and death that can result if an exhausted new mother is encouraged to room in and accidentally falls asleep with her new baby.
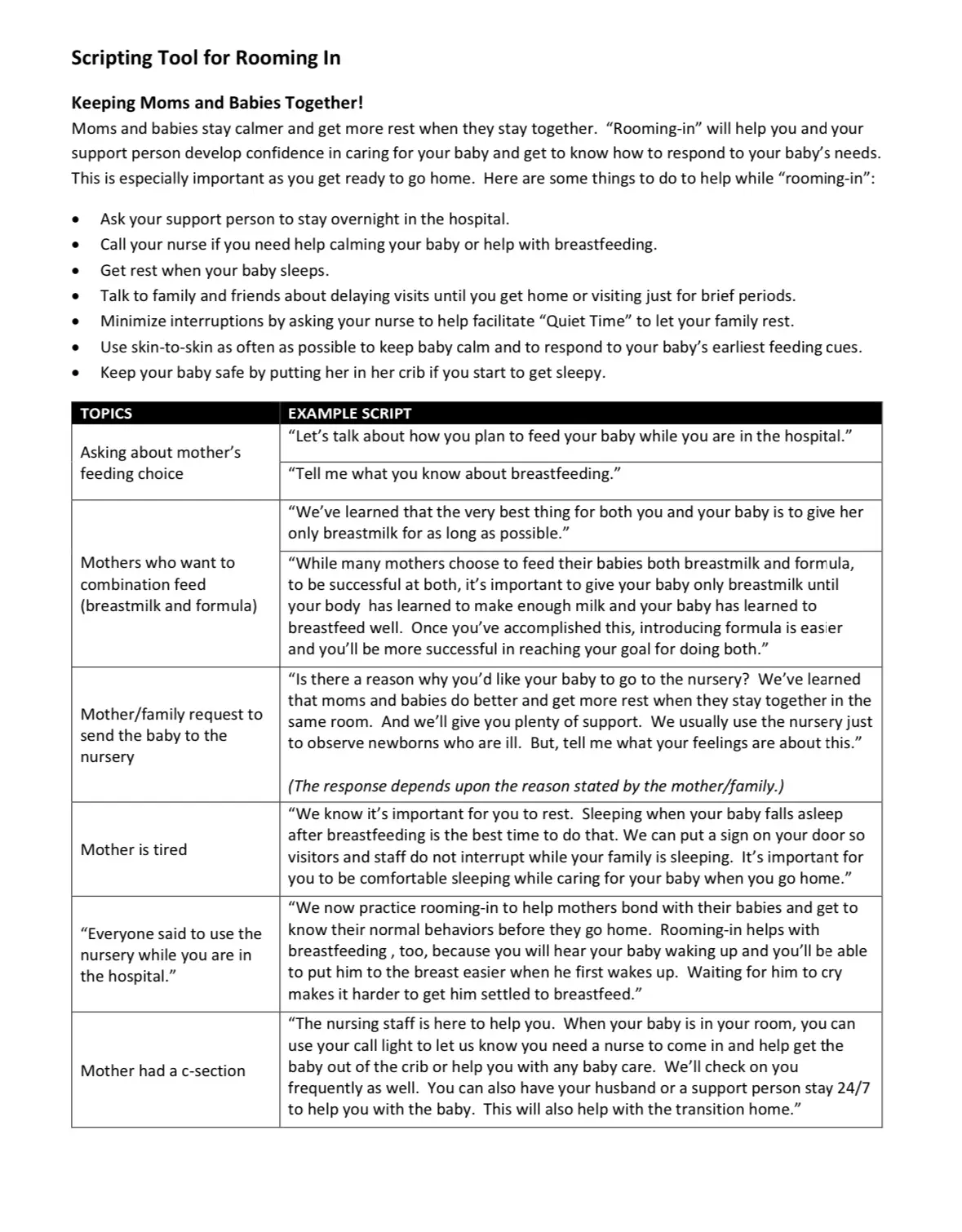
Sample of scripting taught to health professionals to discourage nursery care for babies. From mass.gov
“I routinely see post-op single parents (or ones whose partners need to work) struggling to even lift their babies or change their diapers. Even getting out of bed can be very painful, and short walks to facilitate healing can be exhausting. Taking care of new mothers is one of the keys to successful breastfeeding; sleep reduces cortisol and increases prolactin, facilitating milk production. Learning a new skill like breastfeeding—and being motivated to continue—requires a person to be physically and emotionally well. There is absolutely zero reason why short periods of nursery care to enable sleep would negatively impact breastfeeding. In fact, in some cases it may even help!”
— Lynnette Hafken, MA, IBCLC, Director of Support Services for the Fed is Best Foundation
Now this does not mean we should force or encourage parents and babies to be separated. Rooming in can be beneficial for many families who are trying to establish breastfeeding or just learning how to be new parents however they feed their babies. In fact, the wording of Step 7 is that hospitals should “enable” rooming in, which we agree with. However, it is important to pay attention to the nuances of how this policy is carried out. Even if on paper, parents can choose not to, are families being shamed into rooming in 24/7 even when they are exhausted? Is nursery care being framed as a poor choice that only second rate parents opt for because they don’t care enough to push through physical and mental exhaustion? These messages can be conveyed to parents even if those exact words aren’t used. Messages that say their choice to get help is not the “best” option communicates the same sentiment.
We believe that parents know how to best care for their babies and that the science shows neither their breastfeeding nor their babies will suffer as a result of their request for a few hours of rest. For others, having the option of nursery care is essential for infant safety and maternal recovery.
“Sometimes just 2 or 3 hours of uninterrupted sleep makes mothers feel so much better. What is unsafe is forcing mothers to keep their baby at the bedside when they are exhausted and in pain. We find moms sleeping with their babies all the time, because the baby is fussy, or mom is just exhausted and dozes off. We find babies sleeping in bed with mom all of the time.”
— Kelli Arnette, NICU and Mother–Baby Nurse
Dr. Feldman-Winter goes on to say in the blog, “This idea of an idealized place where babies are separated from their moms as the norm in our culture is actually unsafe,” she says. “I would like to see the whole concept replaced with a new paradigm.” For her part, Feldman-Winter “would like to eradicate the term ‘nursery.’” Let’s not lose sight of what is truly unsafe, which is an environment where mothers feel ashamed of asking for help, where they are given help grudgingly or flat out denied it under the false pretense of guiding her to choose what is best.
Ironically, all of the risks of parental exhaustion from rooming in can be mitigated with nursery care under direct supervision of maternity nurses. The modern-day nursery is a safety net to help families to avoid these risks, NOT as a place that sabotages breastfeeding! Nurseries save lives, but the choice has been taken away in many hospitals, whether or not the Baby-Friendly Hospital Initiative policy endorsed it. Regardless of the Initiative’s intent, the rooming-in policy has made it easier for hospitals to close nurseries (with the added benefit of cutting hospital costs) under the guise of promoting breastfeeding. Nurses moved by compassion to give exhausted parents a few hours of relief often have to keep babies parked in their bassinets at nurses stations rather than keeping them in a far safer nursery with a dedicated nurse to watch over them. This phenomenon ultimately fails mothers and babies.
As a 32-year veteran NICU, nursery nurse and lactation consultant, I want parents to know families can successfully breastfeed while also using the nursery to rest and recover.
- Some can express colostrum prenatally, freeze it and bring it along to have their nurse supplement their baby in the nursery, while the mother is recovering without interruptions.
- Some hospitals have donor milk available for supplementing in the nursery until the mother is alert enough at the next nursing session.
- Supplemental infant formula is also a healthy choice for those who request it.
The Fed is Best Foundation believes successful breastfeeding, hospital support for maternal recovery, and nursery care can all coexist to provide the best possible care for birthing mothers and infants. Respecting patient autonomy also means respecting a parent’s choice to get the help and rest they deserve by giving that service willingly without unnecessary lectures on what is “best.”
Jody Segrave-Daly’s entire 32-year nursing career has been dedicated to caring for healthy and medically fragile babies in the nursery and NICU. When she began her community-based infant feeding practice 6 years ago, she was not prepared to see the significant numbers of babies who were suffering from accidental starvation complications. The stories she heard were the same —distressed mothers were being told to never supplement their crying, sleepy, jaundiced, and dehydrated babies — or risk ruining their breastfeeding relationship and milk supply. She has comforted countless mothers all over the world who believed it was rare to under-produce breast milk and often felt betrayed by their healthcare teams, their own bodies, and the social pressure that insisted “Breast Is Best.” Now a staunch advocate for the Fed Is Best movement, Jody now works to debunk those myths while supporting mothers to breastfeed, mix-feed, pumped-milk-feed, formula-feed and tube-feed their babies. She has her own Facebook page and blog at the Momivist where she uses science and her years of clinical experience to support infant feeding. Read about her journey as a lactation consultant at Why I’m a Momivist.
Another Blog Post:
How Do Misogyny and Feminism Impact the Breast is Best Narrative? – Fed Is Best
Resources:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6353266/
https://www.thebump.com/a/rooming-in-vs-nursery-care
https://www.frontiersin.org/articles/10.3389/fped.2020.00053/full
https://www.sciencedirect.com/topics/nursing-and-health-professions/rooming-in

One thought on “The Illusion of Choice: Baby Friendly USA Says Newborns “Should” Room In With Their Mothers”