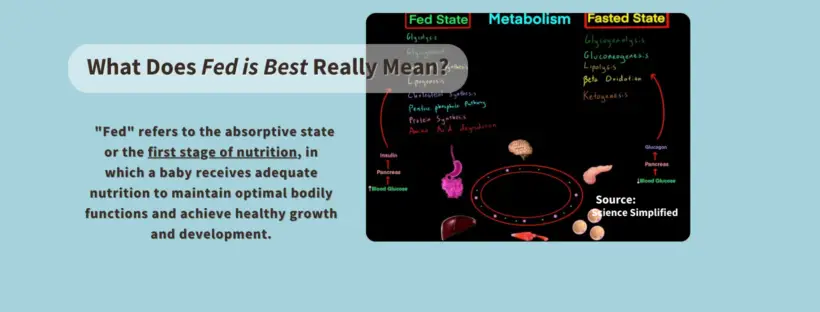
The phraseology of Fed is Best is frequently misinterpreted, and we want to clarify what it means to our readers.Nutritionally speaking, “fed” refers to the absorptive state or the first stage of nutrition, in which a baby receives adequate nutrition to maintain optimal bodily functions and achieve healthy growth and development.
Fed is best means a baby can achieve this fully fed state required to thrive from two clinically-approved sources of nutrition. One is human milk, and the other is infant formula.
Source: Science Simplified, May 13, 2020,Biology/Physiology, Video focused on details of Fed State of Metabolism.
While many babies can exclusively breastfeed, not all babies can thrive on breast milk alone for the WHO/UNICEF-recommended six months since not all mothers produce adequate milk to do so, even with maximum effort and lactation support. In fact, a WHO/UNICEF expert panel gathered in 2002 to determine whether exclusive milk feeding for six months could meet the vast majority of infants’ nutritional needs found that exclusive breastfeeding was rarely practiced in the developing world and rarer still in the developed world. They noted high rates of being unable to meet this goal even among well-nourished and motivated mothers. They found no population study that could tell them how many mothers could not physically meet this requirement. So, despite what many mothers are taught, the idea that nearly all mothers can exclusively breastfeed safely for this duration and that the need for supplementation is rare has never been proven with scientific data. Therefore, all babies in the world can’t befully fed and thrive without the availability of these two important sources of nutrition, especially since it is common not to have enough breast milk to exclusively breastfeed their babies for the first six months of life adequately.
One early study by Neifert et al. found that 15%, or 1 in 7 healthy, motivated mothers, had persistent milk supply problems despite maximal lactation support. The largest study ever done to measure actual breast milk production was done by Kent et al. in 2016. This study found that between days 11 and 13, 2/3rd of the mothers could not produce more than the minimum 440 mL required to feed their infant exclusively, and between 14 and 28 days, nearly 1/3rd could not produce that minimum.
When human milk is not an option, infant formula is vital for a baby’s long-term health outcomes
Some people say being “fed” infant formula is the bare minimum, but that is scientifically false. A fully fed child, whether they are fed with breast milk alone, formula alone, or a combination of both, will have better health outcomes and brain development than an infant that is malnourished from a failed attempt at exclusive breastfeeding without adequate milk supply, which is why we say, “fed is best.” “
Fed is best means that a baby must be fully fed to have the best outcomes, and that can’t always be achieved with breast milk alone. Therefore, parents who choose to feed formula either partially or fully to ensure their child is fully fed, whether out of necessity or choice, are, by definition, providing their child the “best.”
Some have even turned that narrative to suggest that formula is harmful, leading parents to resort to homemade infant formula and informally shared breast milk, which carries the risk of feeding a baby a nutritionally incomplete and/or contaminated source of nutrition.
Infants without access to adequate human milk and/or infant formula who are fed with any other unapproved food sources cannot thrive. They can suffer from complications of malnutrition, including anemia, poor cognitive development, impaired immune function, stunted growth, and, rarely, death.
Even the World Health Organization recognizes the importance of infant formula for babies who do not have access to human milk so they can thrive.

When people say being “fed” infant formula is the bare minimum, they are also trying to shame and ostracize the majority of parents who feed their babies who feed their babies formula at some point in their first year.
How Fed Is Best Began:
In 2015, our Facebook page began titled “Breast is best when you have enough milk.” Our Co-founder, Dr. Christie del-Castillo-Hegyi, an emergency medicine physician, shared her personal story of how her baby didn’t receive enough milk while exclusively breastfeeding under the care of her hospital, pediatrician, and lactation consultants. As a result, he suffered needlessly from starvation complications by the fourth day after birth.
As an emergency medicine physician, she wanted parents to be informed that following the exclusive breastfeeding protocol without adequate colostrum or breast milk supply can result in malnutrition that can cause brain injury and disabilities, as her child experienced. These are well-documented consequences of infant starvation. What is more, she discovered from health professionals that cases like her child were happening several times a week in any hospital that follows the exclusive breastfeeding protocol.
Since no other health organization informs families of the risks of inadequate breastfeeding, she wanted parents to be informed that following exclusive breastfeeding guidelines without adequate guidance on recognizing when breast milk is not enough or when to supplement a baby can result in serious complications, especially in the first days before milk comes in (lactogenesis II).
She believed educating families about delayed lactogenesis II, low milk production, and the need to supplement when they occur was vital to protecting babies from unintentional starvation complications when colostrum/breast milk is insufficient.
It was as simple as that.
It would be an understatement to say we weren’t prepared for the growth of our Facebook page. Messages began pouring in from mothers worldwide, telling us how their babies also suffered from hunger and thirst when their milk did not arrive on time. They falsely believed infant formula would harm their babies and end their breastfeeding journey.
We promote safe breastfeeding because no other health organization informs parents about the risks and how easy they are to prevent.
They were falsely told the same thing: to ‘believe’ in their bodies, that all mothers make enough milk, that exclusive breastfeeding was best; their crying, hungry babies were just ‘cluster feeding,’ and it was necessary to bring in their milk. Their lived reality wasn’t validated, leaving them feeling alone and confused. Most importantly, they were not believed, and their babies suffered.
Parents also told us they desperately needed to hear a more inclusive infant feeding message and needed support for their infant feeding journey because not every parent can make enough milk or chooses not to for VALID reasons.
We took to heart the thousands of letters from families asking us to change our phraseology from “Breast is best if you have enough milk” to Fed is Best, and in 2016, The Fed Is Best Foundation was officially born.
Considering that the #1 rule of lactation is to feed the baby, Fed is Best was an obvious choice for our new name, and we launched the Fed Is Best Foundation to make it official.
We Want To Be Clear About What The Fed Is Best Foundation Stands For:
- We are fiercely passionate about educating parents about how to breastfeed safely because no other healthcare organization does. The facts don’t lie. 1 in 71 exclusively breastfed babies is rehospitalized for health- and brain-threatening complications of insufficient breastfeeding.
- We do not dispute the health benefits of breastfeeding or pumped human milk for parents or babies found in well-controlled trials, like lower rates of gastrointestinal and respiratory infections, eczema, as well as life-threatening necrotizing enterocolitis in premature infants. It would be unethical to do so as healthcare professionals.
- We believe that to receive those benefits, an infant must receive enough milk to meet their full nutritional requirement.
- We believe that you don’t have to exaggerate the benefits of breastfeeding or tell parents they are harming their infants by giving them formula to support breastfeeding.
- We believe parents should be informed of the risks and benefits of all infant feeding methods to ensure optimal feeding outcomes for all babies, nursing parents, and their families.
- We believe families should get equal and unbiased infant feeding support without pressure, shame, or judgment, whether they are breast, combination, expressed milk, formula, or tube feeding.
- We respect formula-feeding families and infant formula itself. Doing so is not anti-breastfeeding; it’s responsible, inclusive, and pro-safe infant feeding.
- We believe parents get to decide the best way to feed their babies; they are the experts in their own lives.
What we oppose is the way breastfeeding is promoted because:
- The Baby-Friendly protocol teaches the benefits of breastfeeding but fails to educate parents about the risks associated with inadequate feeding during the first few days of life when breastfeeding exclusively. In doing so, parents are denied vital health information to protect their babies, violating their rights as patients.
- The pressure to exclusively breastfeed is associated with the onset of mental health conditions. It implies inadequacy in the role of a parent when exclusive breastfeeding is not possible for biological or other reasons, leading to depression, anxiety, and other mental health conditions.
- No one should have to disclose their reasons for not breastfeeding to get immediate access to food for their baby.
- The promotion of breastfeeding has moralized parenthood and created a social hierarchy that casts breastfeeding parents as “better” than formula-feeding parents.
- It perpetuates fear, pressure, shame, guilt, blame, and judgment if a family cannot exclusively breastfeed or chooses another method.
- It inflates or misinforms parents about the benefits of breastfeeding and human milk.
- It falsely instills fear about infant formula feeding.
- It leads parents to normalize signs of underfeeding to maintain their baby’s exclusive breastfeeding status, leading to tragic, preventable hospitalizations of babies to correct brain-threatening complications.
- It does not adequately consider the needs of families who have maternal mental health conditions or disabilities as the priority.
- It does not validate the fact that 1 in 4 parents in the United States return to work two weeks after delivery for survival and that often, this makes breastfeeding difficult or impossible to maintain for some nursing mothers.
Please remember this:
Breast/chestfeeding, combo feeding, banked donor milk, expressed human milk feeding, formula feeding, fortified milk, tube feeding, and TPN (intravenous feeding) are all best options parents have to meet their babies’ nutritional needs.
Your best version may not be another parent’s best way to feed their baby. Therefore, each family gets to decide with their healthcare professional which type of milk and feeding method will nourish their baby in the best way possible, given their unique situation.
We hope our message will provide support, compassion, education, and optimal outcomes for all families, not just some families. We hope our advocacy will change breastfeeding promotion and policies to prioritize infant feeding safety and mental health outcomes.
Meanwhile, we need to fiercely advocate for paid family leave so that those who want to breastfeed can do so. It is also vital to protecting perinatal mental health, a solid win for families and society.
*Note: The phrase Fed Is Best is trademarked to prevent others, including formula companies, from profiting from our advocacy work. Please contact us if you see Fed Is Best used by others inappropriately. Thank you!
Christie, Jody, and Lynette

Lynette is the director of Support Services at the Fed Is Best Foundation.
Contact us: [email protected]
FAQs Part 1: The Most Common Questions Answered At The Fed Is Best Foundation
Weight Loss is Not Caused by IV Fluids: The Dangerous Obsession with Exclusivity in Breastfeeding:
If I Had Given Him Just One Bottle, He Would Still Be Alive.