Paced bottle feeding is a wildly popular bottle feeding technique that is promoted as the best way to feed babies who are breastfed. When I did a google search for paced bottle feeding, there were a whopping 572,000,000 results! What’s more, definitions of paced bottle feeding techniques varied significantly, often contradicting each other, and there were many unproven claims to promoting paced feeding.
As a 31-year NICU nurse and lactation consultant, I’m mystified why paced feeding for healthy term babies has become the norm. Pace feeding is a therapeutic feeding technique primarily used for medically complex and premature babies whose suck, swallow, and breathe (SSB) reflex is not coordinated or matured, which is essential to bottle-feed without aspirating milk into the lungs.
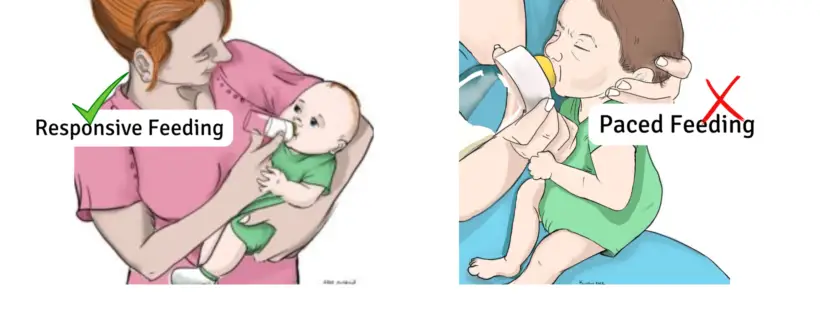
The American Academy of Pediatrics (AAP) and global infant feeding guidelines advocate and promote responsive feeding, which is uniquely different from paced feeding. Full-term, healthy babies are born with their SSB coordination fully developed and can responsive bottle feed safely.
The importance of educating parents about responsive bottle-feeding techniques cannot be glossed over when in the US; at least 75-85 percent of babies are bottle-fed using human milk or infant formula. To clarify the misinformation about the differences and similarities between responsive and paced feeding, I decided to delve into the research and write an educational blog for parents to practice responsive bottle-feeding for their babies.
How Did Paced Feeding Evolve to Become The Bottle-Feeding Technique Promoted For Healthy Term Babies?
In 2002, lactation consultant, Dee Kassing, wrote about a technique she was using in the clinical setting for term babies who were bottle-fed when separated from their breastfeeding mothers in the Journal of Human Lactation. Her goal was to develop a method of bottle-feeding that would mimic breastfeeding and prevent nipple confusion. However, the Kassing method is based on outdated research from the early 1980s, and current research debunks her theory about nipple confusion and pace feeding being similar to breastfeeding.
The selection of bottle nipples 20 years ago was limited, and the flow rate was very fast, despite being labeled a slow flow nipple. I remember using those nipples, which were challenging to feed babies with. The only way to control the fast flow was by using gravity to slow the milk flow and removing the nipple out of the mouth so the baby could swallow without choking until they mastered the flow. Through no fault of her own, Kassing’s method evolved into paced feeding over the years, despite the current recommendations for responsive feeding.
Significant technological design advancements have been made over the past 20 years with nipple flow, nipple types, and bottles, and the improvements provide many options that help parents select the right nipple flow according to their baby’s age, so they can self-regulate their milk intake when practicing responsive feeding.
What exactly is responsive feeding?
Responsive feeding is a learned feeding behavior that involves back-and-forth communication between the baby and the parent/caregiver during the bottle feeding process. Responsive feeding allows the baby to set and regulate their sucking pace while signaling their hunger and fullness cues to the parent. The parent then responds to their feeding cues.

Responsive feeding is baby-led and is a nurturing and bonding experience.
Pace feeding is the opposite in that the parent controls the sucking pace and stops the feeding in a controlled fashion, which doesn’t allow the baby to learn self-regulation of their milk intake. Sometimes the goal is to limit the milk intake set by the parent and make the baby ‘work harder” for their milk, which is not evidence-based feeding practice.

Pace feeding is the parent controlling the sucking pattern, which inhibits the development of self-regulation of milk intake by the baby.
What does the research say about responsive feeding?
Responsive feeding is supported by ample research and is considered an important factor in developing lifelong eating habits. According to the AAP, “You can practice responsive feeding when breastfeeding, bottle feeding, and when providing solid foods.”
What are the benefits of responsive feeding?
- Helps your child develop healthy eating habits by learning how to self-regulate their nutritional intake and setting their own pace for feeding.
- Develops parental trust when responding to your baby’s hunger or fullness feeding cues.
- Supports the development of a close and loving relationship with your baby while holding them close and interacting and responding to their feeding cues during the feeding.
- May lower your child’s risk of becoming overweight as he gets older because of learning how to self-regulate their nutritional intake and satiety/fullness cues.
- The upright position when responsive feeding can help reduce ear infections.
How do I practice responsive bottle feeding?
There are three principles to follow when responsive bottle feeding your baby.

Research published in 2020 found bottle feeding is a 3 part system of milk intake, milk delivery, and feeding interactions, enabling the baby’s ability to regulate their milk intake according to their hunger and fullness cues.
1. Responding to hunger cues

- Respond to your baby’s early hunger cues by picking them up and placing them in an upright feeding position. Crying is a late sign, and it’s helpful to be fed before they become HANGRY. However, there are some babies whose cry is the first sign of hunger.
- Position them upright at a 45-degree angle (or more when possible) for feeding and hold your baby close to your body, with their head supported in the crook of your arm, so they feel secure. *Feeding your baby upright at least at a 45-degree angle has reduced the risk of ear and respiratory infections.
2. The Milk Delivery
Selecting the correct slow nipple flow and positioning of the bottle while feeding is the foundation for responsive bottle feeding.
- Term newborns can self-regulate and remove milk using the right nipple flow and positioning of the bottle while feeding. Infants struggle with their sucking-swallow-breathe reflex if the nipple flow is too fast. Term healthy newborns can instinctively change their sucking rate and strength to manage the milk flow from the right slow flow nipple.
- When offering the nipple, hold the bottle angled just so the milk completely covers the nipple; that way, your baby isn’t swallowing extra air, which may contribute to gas pains and upset tummies.

According to research tilting a bottle vertically does not indicate an accurate nipple flow.
3. Parent and baby interaction during the feeding
- Interacting with your baby during the entire feeding is essential. Responding to the verbal and non-verbal hunger and fullness cues assists your baby in practicing and achieving self-regulation of their milk intake.

- Provide feeding breaks when signaled, and respond to their fullness cues by stopping the feeding. Do not encourage them to finish their bottle. It’s important to respect their fullness cues.
- When responsive feeding, babies can feed smaller and larger amounts of milk at each feeding throughout the 24-hour period.
- The goal is to allow the baby to practice self-regulation of their nutritional intake and recognize their satiety/fullness cues.
- What’s important is the total 24-hour volume intake that meets your baby’s caloric intake needs for optimal growth.
How to select the right slow-flow nipple for your baby
There are many bottle nipples and systems available for parents to choose from, and they all say similar things such as “slow flow,” “most like breastfeeding,” “anti-colic,” or “prevents gas,” all in hopes that parents will buy them. Unfortunately, the claims made are simply marketing strategies, and there are no set standards. Thankfully, research can help narrow down what nipple flow may work best for your baby.
Which bottle nipples are genuinely “slow flow?”
Below are the results of a study that measured the nipple brand and flow rates, ranging from extra-slow flow to very fast flow. This information can help parents find the right slow-flow nipple.

Photo credit from Know the Flow: Milk Flow Rates From Bottle Nipples Used in the Hospital and After Discharge
Let’s review The dos and don’ts of responsive bottle feeding
| What Responsive Bottle-Feeding Is | What Responsive Bottle-Feeding Is Not |
| RF responds to hunger cues by offering milk and allowing the baby to suck and swallow at their own pace to develop self-regulation of milk. | Responds to hunger cues by offering milk but is parent-controlled, which impedes the baby’s ability to self-regulate milk on their own. |
| RF responds to fullness cues and stops the feeding when the baby signals they are finished or pauses the feeding if the baby signals they want a break from sucking. | Responsive feeding does not require babies to stop sucking, suck on an empty teat, or be unlatched from the bottle intermittently throughout the feeding. This parent-controlled feeding style will impede the baby’s ability to self-regulate and prevent signaling their own hunger or fullness cues. |
| RF is when the caregiver provides a positive feeding experience by cradling the baby upright and holding them close, which assists infants in being interactive participants in the process of bottle-feeding. | RF does not place a baby in a position that does not allow close interaction and participation in the feeding process, such as sitting straight up on the lap or side-lying position while feeding. |
| RF interactively feeds a baby with the desired amount, always following their hunger cues. No more and no less. | RF should not be used to withhold or minimize milk intake.
RF should not use food to calm or soothe a baby when they are not hungry. RF should not force a baby to finish the bottle; it honors their fullness cues. RF is not propping a bottle. |
| Responsive feeding allows the baby to self-pace and regulates their intake. Term newborns have a normal, rhythmic suck/burst cycle, normal sensations of fullness, and do not need pacing. | RF does not regulate sucking and volume intake, which often leads to parent and infant feeding frustration because pacing is not the norm for feeding healthy babies. Babies instinctively want to suckle at their own pace. |
Lynnette Hafken, MA, IBCLC, writes, “It is stressful for parents to be told they must bottle-feed in a complicated way to preserve breastfeeding. Following a prescribed set of rules overmedicalizes feeding and puts even more of a burden on a person learning to breastfeed. There is also the unspoken implication that bottle-feeding threatens their breastfeeding success if not done exactly right. In my experience, after 20 years of helping mothers breastfeed, it is better to allow both breastfeeding and bottle-feeding to be an intuitive, pleasant, and bonding experience for both parent and baby. Bottle-feeding does not have to be a threat to breastfeeding—it is simply a tool that can even be helpful to breastfeeding when used appropriately. “
There are responsive feeding exceptions for healthy newborns.
Some term newborns will require additional feeding interventions such as external pacing until responsive feeding is mastered. Early term babies (37 weeks through 38 weeks, six days) often need temporary interventions with bottle feeding during the first days of life. Babies who are transitioning from the NICU have low muscle tone or any other medical concerns.
This video below depicts responsive bottle feeding practices
 Jody Segrave-Daly is the co-founder of the Fed Is Best Foundation. She is a registered nurse, and her 31-year nursing career has been dedicated to caring for healthy and medically fragile babies in the nursery and NICU. She is frequently referred to by parents as “the baby whisperer” because of her extensive career working with newborns. She has been an international board-certified lactation consultant since 2010, who recently placed her credential in retirement status to pursue an advanced nurse practice degree. She is the founder of The Momivist; Evidence-Based Infant Feeding Education, an infant feeding education writer, and has taught parents how to safely breastfeed healthy and medically complex babies for over 31 years.
Jody Segrave-Daly is the co-founder of the Fed Is Best Foundation. She is a registered nurse, and her 31-year nursing career has been dedicated to caring for healthy and medically fragile babies in the nursery and NICU. She is frequently referred to by parents as “the baby whisperer” because of her extensive career working with newborns. She has been an international board-certified lactation consultant since 2010, who recently placed her credential in retirement status to pursue an advanced nurse practice degree. She is the founder of The Momivist; Evidence-Based Infant Feeding Education, an infant feeding education writer, and has taught parents how to safely breastfeed healthy and medically complex babies for over 31 years.
As a mother of three children, her breastfeeding experiences were uniquely different but were rewarding and positive experiences that she cherishes. Her mission is to ensure that every family has a safe and positive feeding experience, no matter how their baby is fed. Positive infant-feeding relationships are the core of parenthood, building trust, bonding, and love, and must be protected.
Resources
Clarifying nipple confusion – PubMed (nih.gov)
Exploring Correlates of Infant Clarity of Cues During Early Feeding Interactions – PubMed (nih.gov)

One thought on “Why it’s Time to Stop Teaching Parents Paced Bottle Feeding and Teach Responsive Feeding As Recommended by the AAP”