Paced bottle feeding is a wildly popular bottle feeding technique that is promoted as the best way to feed babies who are breastfed. When I did a google search for paced bottle feeding, there were a whopping 572,000,000 results! What’s more, definitions of paced bottle feeding techniques varied significantly, often contradicting each other, and there were many unproven claims to promoting paced feeding.
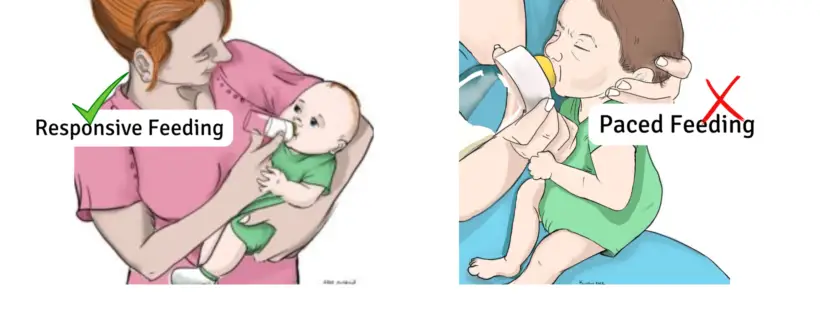
As a 31-year NICU nurse and lactation consultant, I’m mystified why paced feeding for healthy term babies has become the norm. Pace feeding is a therapeutic feeding technique primarily used for medically complex and premature babies whose suck, swallow, and breathe (SSB) reflex is not coordinated or matured, which is essential to bottle-feed without aspirating milk into the lungs.
The American Academy of Pediatrics (AAP) and global infant feeding guidelines advocate and promote responsive feeding, which is uniquely different from paced feeding. Full-term, healthy babies are born with their SSB coordination fully developed and can responsive bottle feed safely.
Continue reading →