Written by Fed is Best Co-Founder, Christie del Castillo-Hegyi, M.D.
Professionals in the medical community and parents have asked questions regarding whether or not newborn starvation from insufficient exclusive breastfeeding is linked to Autism Spectrum Disorder (ASD) in children and what research has been done regarding a possible connection.
The short answer is no. There is no definitive linkage, and we don’t have clear answers when we’re queried about this fact – because in fact, the science is not entirely clear on this point.
Formally, Autism Spectrum Disorder is the name for a group of developmental disorders, which you can read more about here. Although, it can look very differently from person to person, ASD is currently defined as a person with 1) ongoing social problems that include difficulty communicating and interacting with others and 2) repetitive behaviors as well as limited interests or activities. When presented to a diagnosing physician, the combination of these two factors will typically result in an ASD diagnosis. The diagnosis describes a constellation of developmental characteristics but do not describe the cause of the disorder. There is plenty of discussion about whether autism rates are increasing or if the disorder is simply being diagnosed more frequently, neither of which we will address here as it is outside of the scope of our Foundation’s work.
At this time, science cannot tell us precisely why ASD occurs. Scientists have found positive associations between genetic and environmental variables and an individual’s eventual diagnosis. While a small percentage of individuals with ASD have a purely genetic origin, the vast majority of individuals with ASD do not have an identified genetic cause. Also at this time, there is no one definitive answer as to what is triggering the disorder, just a series of risk factors gleaned from data analysis of children with ASD.
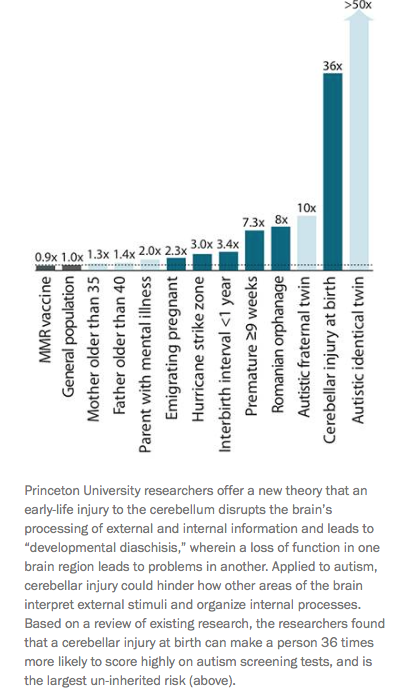
Among the risk factors that have been strongly associated with an autism diagnosis is injury to a part of the brain called the cerebellum around the time of birth. A review article published in 2014 in the neuroscience journal Neuron stated the following, “Based on a review of existing research, the researchers found that a cerebellar injury at birth can make a person 36 times more likely to score highly on autism screening tests, and is the largest uninherited risk.” In a review published in Seminars in Fetal and Neonatal Medicine on bilirubin-induced brain injury, the cerebellum was noted to be the most vulnerable region to injury in severe hyperbilirubinemia and is in fact the definitive lesion found in animal models of kernicterus, the brain injury caused by high bilirubin levels. In this same issue, leading neonatal hyperbilirubinemia investigator, Dr. Vinod Bhutani, who developed the bilirubin nomogram used by pediatricians to manage neonatal jaundice, noted that the areas affected in schizophrenia and autism were similar to the areas affected in infants experiencing Bilirubin Induced Neurologic Disorder (BIND), the more subtle form of kernicterus. He wrote, “Thus, in terms of brain volumetrics, schizophrenia and autism spectrum disorders have a clear degree of overlap that may reflect shared etiological mechanisms. Overlap with injuries observed in infants with BIND raises the question about how these lesions are arrived at in the context of the impact of common etiologies.”
Whether babies who develop bilirubin-induced brain injury go on to develop the condition we know as ASD or simply look like they have ASD, we can’t say for certain. Without the appropriately controlled animal models that show poor feeding leads to hyperbilirubinemia (which is a known correlation) and then to an autism diagnosis, no one can say or claim that brain injury from poor feeding and autism are the same thing. As previously stated, there’s a lot that science does not know about the exact pathology of autism, and the autism spectrum is understood to include a wide range of individuals with a very wide range of cognitive skills and abilities. The same can be said about individuals who have sustained brain injury, but that does not mean that they are one in the same.
What we can tell you is that science does say that there is a causal relationship between newborn hypoglycemia and brain injury, and this brain injury can result in developmental disabilities. The latest article published in the Hospital Pediatrics Journal on underfed lethargic breastfed newborns who develop hypoglycemia suggests that by the time they have reached this stage of lethargy, there is evidence that they may have experienced brain injury to a third to almost the entire brain. These children went on to have long-term neurological disabilities including epilepsy, visual impairment and feeding difficulties. Every brain cell including those in the cerebellum is susceptible to brain injury from caloric deprivation caused by hypoglycemia. The number of insufficiently breastfed babies who develop hypoglycemia and subsequently receive brain MRIs is exceedingly low because it is not widely offered to hypoglycemic breastfed babies. Therefore, we do not know the number of babies experiencing this phenomenon. What we do know now, from a study published in the Journal of Clinical Diagnostic Research, that 10% of healthy, term exclusively breastfed newborns are hypoglycemic to <40 mg/dL by 6 hours of life when monitored up to 48 hours. The rate of hypoglycemia was even higher among first-born exclusively breastfed newborns as 23% developed hypoglycemia. The levels of hypoglycemia experienced by these newborns were to a level that has been shown in another study published in JAMA Pediatrics, to be associated with a 50% reduction in their ability to pass the 4th grade proficiency test in literacy and math, even with the hypoglycemia corrected. This is consistent with what the basic science of hypoglycemic brain injury says about hypoglycemia. Even short episodes of hypoglycemia can result in brain injury that is irreversible and can have long-lasting effects on a child’s cognitive development.
We have known for decades that perinatal brain injury is the leading cause of language, motor and cognitive disability in children, so while we can speculate that it is possible that starvation-related brain injury could be interpreted as ASD, as practitioners of evidence-based medicine with a lack of comprehensive evidence to officially support that, we cannot draw any formal conclusions associating these two concepts.
Although the links between poor feeding and autism have not been fully elucidated, the causal relationship between poor feeding and brain injury should prompt mothers and health providers to learn about and adopt safe breastfeeding or safe formula-feeding practices. Likewise, it is not a reason to avoid exclusively breastfeeding a newborn if that is indeed something that a mother’s supply allows and it is her preferred choice of infant feeding. We also do not support mothers avoiding vaccinations for their children who cite the same insult-to-ASD claim, as that claim, along with the since-debunked study that suggested it, have long been used as a method to dissuade parents from getting their children vaccinated. While some parents believe that vaccines can cause autism because of alleged injury, the wide body of scientific literature shows that this is simply untrue.
Most recently, a large-scale study out of California published in the September issue of the journal Pediatrics looked into the possibility of a relationship between infant hyperbilirubinemia (excessive jaundice) or phototherapy treatment for hyperbilirubinemia and ASD diagnosis. Why would there be a study of this nature?
Because, per the authors “It is hypothesized that environmental insults occurring during early brain development can lead to ASD among infants who are genetically vulnerable,” and jaundice is well-known to cause brain injury when it is severe and sustained. The study showed there was an increased risk of autism in the children who developed hyperbilirubinemia and those that required phototherapy. But when looking at the relationship between multiple variables, it appeared that it wasn’t the high bilirubin or need for phototherapy that increased the risk for autism diagnosis. What this means, is that the factor that lead to the development of autism is another factor possibly occurring in the babies that developed hyperbilirubinemia. The factors they did find were factors that we have found to be risk factors for feeding problems related to breast milk supply and hypoglycemia in newborns, including older parental age, higher parental education and having a small or large baby.
Our bottom line is, as it relates to unintentional infant starvation, that it does not matter what the diagnosis is or could be. We want to protect our children through safe infant feeding practices regardless. We want to support mothers in making empowered feeding choices that keep their babies safe and well-fed. There is nothing wrong with children of any developmental category!
Ultimately, in order to protect the brains of every baby, we believe that #FedIsBest.
For more information on autism from the National Institutes of Mental Health, go to https://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd/index.shtml
Another article: https://www.thebabbleout.com/autism/
In a situation whereby u fed ur baby early stage of life then stop when the breast milk start to flow very well, will u still say the baby is starving ? . mean while the baby is responding to the breast milk very well I mean his healthy the weight is normal ..thanks
We support mothers who want to supplement their breastfeeding in the first days of life and then stop supplementation once breast milk supply is enough. It is actually how the majority of babies were fed before the WHO breastfeeding guidelines were published in 1991. Because of the guidelines, millions of babies have suffered starvation-related complications that they were protected from by supplementation in the first days of life.
I wonder though in response to the reply seen above- these moms who start supplementing formula (immediately following birth) in place of nursing, because she is thinking it isn’t enough for her baby… what do you do when they fall victim to the “top up trap”… many moms don’t get the pump education needed to encourage or sufficiently establish their breastmilk supply. Instead they are taught how to allow baby to establish their supply. If they supplement instead then the supply isn’t being demanded and
these moms would just struggle with lack of milk supply… forever.
In the beginning of lactogenesis it’s imperative to demand the supply in order to increase the prolactin receptor sites, which will in turn, establish a good supply later on in the breastfeeding journey- if this isn’t being done or educated- then breastfeeding will eventually become obsolete (much like it did…)
I agree FedIsBest- absolutely.
I just don’t want the benefits of breastmilk or our natural biology to be overshadowed or dismissed.
Similar to formula being better for an infant than cows milk- breastmilk is better for an infant than formula…
being fed period though is better than starvation…
it’s a tricky thing…
I will admit though- reading some of the things here has me sad and happy at the same time….
The randomized controlled studies on early supplementation for underfed babies shows that supplementation after breastfeeding doubles exclusive breastfeeding at 3 months. There is no evidence that failures in breastfeeding are not caused by a mother’s biological limitation to produce milk. The “top up trap” idea is exactly the same evidence-less teaching from the lactation community that causes mothers to accidentally starve their newborns. The downside of not supplementing is starving a newborn and disabling them for life. You cannot simply teach mothers that “Just One Bottle” will harm their baby without teaching them the harm of letting their babies go hungry.