by Christie del Castillo-Hegyi, M.D.
One of the most important duties of the medical profession is to make health recommendations to the public based on verifiable and solid evidence that their recommendations are safe and improve the health of nearly every patient, most especially if the recommendations apply to vulnerable newborns. In order to do this, major health recommendations require extensive research regarding the safety of the real-life application of the recommendation at the minimum.
Multiple health organizations recommend exclusive breastfeeding from birth to 6 months as the ideal form of feeding for all babies under the belief that all but a rare mother can exclusively breastfeed during that time frame without underfeeding or causing fasting or starvation physiology in their baby. In order to suggest that exclusive breastfeeding is ideal for all, if not the majority of babies, one would expect the health organizations to have researched and confirmed that all but a rare mother in fact produce sufficient milk to meet the caloric and fluid requirements of the babies every single day of the 6 months without causing harmful fasting conditions or starvation. There have been few studies on the true daily production of breast milk in breastfeeding mothers. Only two small studies quantified the daily production of exclusively breastfeeding mothers including a study published in 1984, which measured the milk production of 9 mothers, and one in 1988, which measured it in 12 mothers. After extensive review of the scientific literature, it appears the evidence that it is rare for a mother to to not be able to produce enough breast milk to exclusively breastfeed for 6 months is no where to be found. In fact the scientific literature has found quite the opposite.
In November 2016, the largest quantitative study of breast milk production in the first 4 week after birth of term infants was published in the journal Nutrients by human milk scientists, Dr. Jacqueline Kent, Dr. Hazel Gardner and Dr. Donna Geddes from the University of Western Australia. They recruited a convenience sample of 116 breastfeeding mothers with and without breastfeeding problems who agreed to do 24 hour milk measurements through weighed and pumped feedings between days 6 and 28 after birth and were loaned accurate clinical-grade digital scales to measure their milk production at home. The participants test weighed their own infants before and after breastfeeding or supplementary feeds and recorded the amounts of breast milk expressed (1 mL = 1 gram). All breast milk transferred to the baby, all breast milk expressed and all supplementary volumes were recorded as well as the duration of each feed.
These were the results…
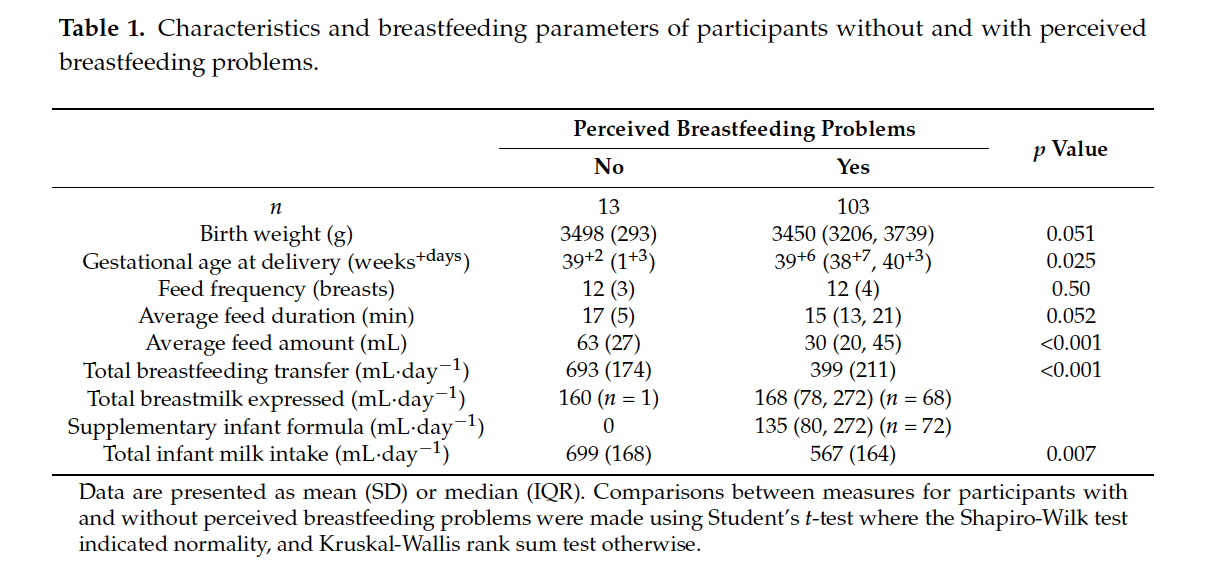
13 mothers perceived no breastfeeding problems while 103 mothers perceived breastfeeding problems. The most common problem was insufficient milk supply (59 mothers) followed by pain (11 mothers), and positioning/attachment (10 participants). 75 mothers with reported breastfeeding problems were supplementing with expressed breast milk and/or infant formula.
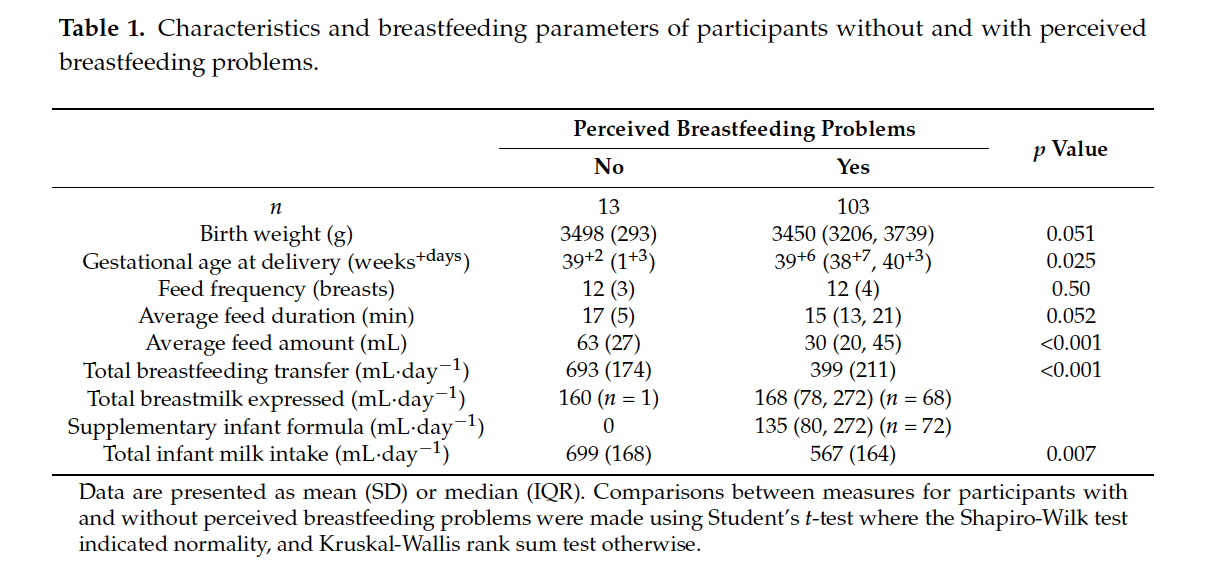
Of the mothers with reported breastfeeding problems, their average weighed feeding volumes were statistically lower than the mothers who did not report breastfeeding problems with an average feed volume of 30 mL vs. 63 mL in the mothers who reported no breastfeeding problems (p<0.001). The daily total volume of breast milk they were able to transfer (or feed directly through breastfeeding) were also statistically lower than those who did not report breastfeeding problems. The moms without breastfeeding problems transferred an average of 693 mL/day while those that reported breastfeeding problems transferred an average of 399 mL/day (p<0.001). The study defined 440 mL of breast milk a day as the minimum required to safely exclusively breastfeed. This is the amount of breast milk that, on average, would be just enough to meet the daily caloric requirement of a 3 kg newborn (at 70 Cal/dL and 100 Cal/kg/day). Babies of mothers with no reported breastfeeding problems were statistically fed more milk than those with breastfeeding problems, 699 mL vs. 567 mL per day (p = 0.007). All 13 mothers who perceived no breastfeeding problems produced and transferred more than the study’s 440 mL cut-off as the volume required to be able to exclusively breastfeed. What this data shows is that a mother’s perception of breastfeeding problems is associated with actual insufficient volume of breast milk fed to her child.
Based on the 440 mL cut-off for “sufficient” breast milk production, some mothers who report their babies not getting enough in fact produced more than 440 mL. However, since 440 mL is the amount of milk that is needed to meet the minimum caloric requirement of a 3 kg newborn, if the mother had a newborn weighing > 3 kg as they would expect to be past the first days of life if growing appropriately, many of the mothers reporting breastfeeding problems may be producing more than 440 mL but are still in fact producing less than the amount to keep their child satisfied and fed enough to grow. A supply of 440 mL would actually be just enough milk to cause a 3 kg newborn to be diagnosed to fail to thrive at 1 month since they would not gain any weight if fed this volume of milk. Failure to thrive has known long-term consequences including lower IQ at 8 years of age. So their conclusion that some mother’s perception of insufficient breast milk may in fact be inaccurate as a volume of 440 mL is in fact “not enough” for most newborns weighing > 3 kg.
Continue reading →