Written by: Allison Stillwell Young, RN, BSN, Graduate Student and Team leader of the fed is best foundation mental health advocacy team
is an oncology nurse at Vanderbilt-Ingram Cancer Center in Nashville, Tennessee. A graduate of Belmont University, she has spent her entire nursing career between research oncology and behavioral health. After the birth of her older son, she developed anxiety and depression directly related to difficulties she experienced with breastfeeding including low supply and feeding judgment. She discovered Fed Is Best during her recovery from PPD/A and found the Foundation to be indispensable when feeding her younger son. As a researcher and mother living with chronic mental illness, she believes that the treatment for perinatal mood disorders should have evidence basis, and she therefore co founded a large, online pro-science peer support group for those experiencing PMADs in 2016. She sits on the board for the Tennessee chapter of Postpartum Support International and functions as one of their state support coordinators for the Midstate.
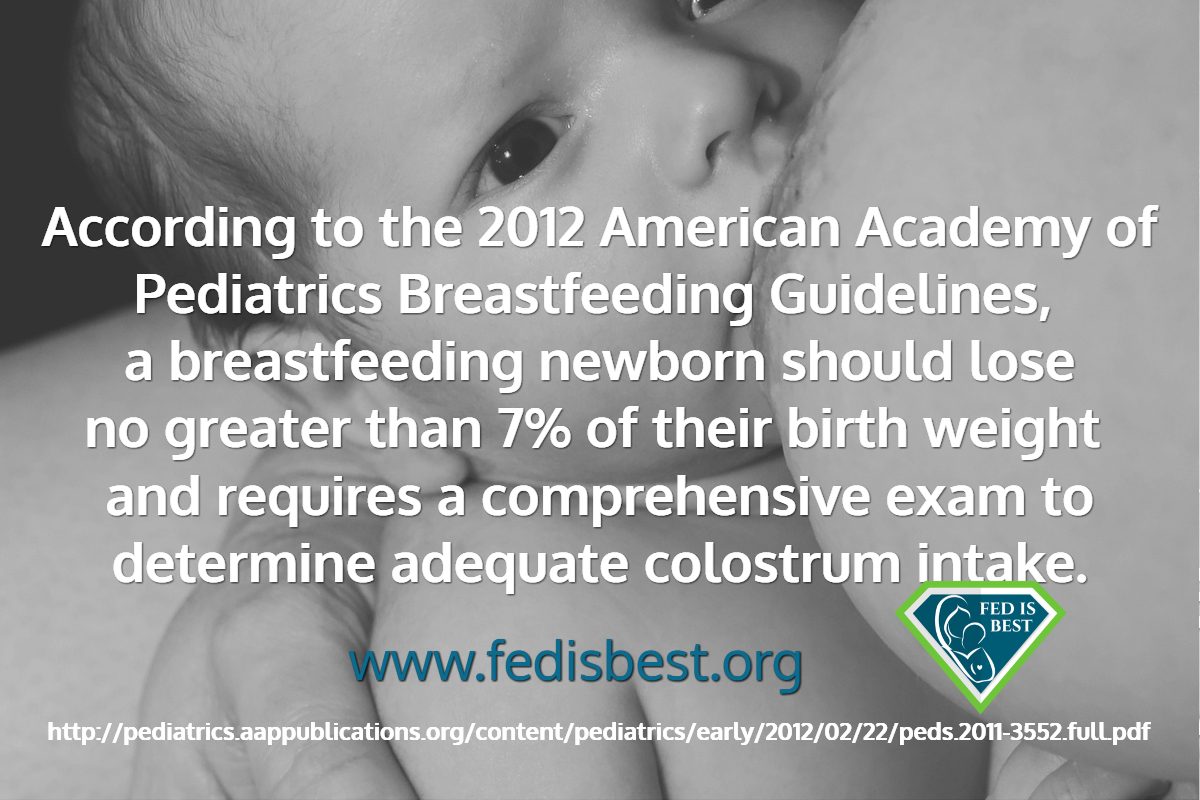
I had our second child last Monday. Since that evening, we’ve been supplementing with formula due to the fact that I have insufficient glandular tissue (IGT) and I am not physically able to exclusively breastfeed. Yesterday, our older son wanted to help feed his baby brother a bottle and, while he was helping, my husband took this picture of them that I loved. I made it my profile picture, and the fact that I felt comfortable posting a picture of my sons with a bottle really shows a sea change in my feelings about infant feeding. Because of that picture, I wanted to post my story about lactivism, which is extremist exclusive breastfeeding advocacy, and how it affected my postpartum mental health after my older son’s birth. It’s pretty long, but I hope my story illuminates how The Fed is Best Foundations provides important support for new mothers. Continue reading