I had a beautiful, healthy pregnancy with Bryson, with the help of Clomid (a fertility drug), like my first pregnancy with my daughter. After about 31 hours of induced labor, Bryson was here. Seven pounds, twelve ounces, and seemingly healthy! He latched like a champ immediately, and we had zero complications of any sort while in the hospital. He had wet and dirty diapers and was breastfeeding well, every 2–3 hours. His discharge weight was 7 lbs, and I had a follow-up appointment scheduled for two days later.
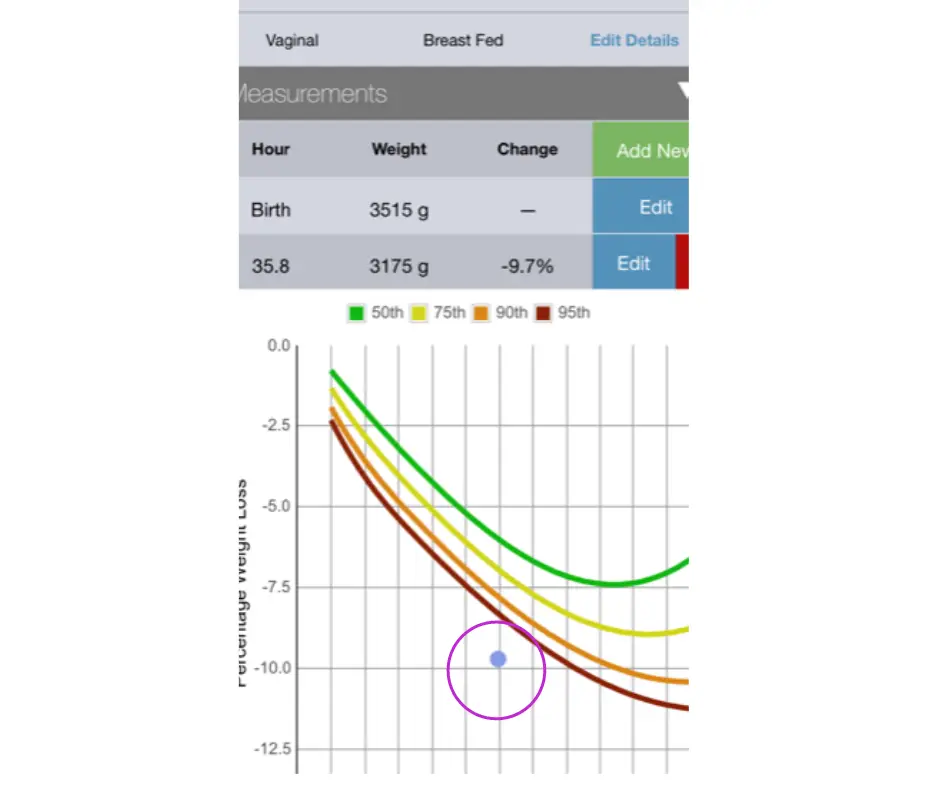
NEWT is the first tool that allows pediatric healthcare providers and parents to see how a newborn’s weight during the first days and weeks following childbirth compares with a large sample of newborns, which can help with early identification of weight loss and weight gain issues. Bryson was discharged with a weight loss of 9.7 percent at 36 hours of age. The NEWT graph indicates his weight loss was excessive.