As a result of my traumatizing breastfeeding experience, I became an IBCLC. My goal as an RN and IBCLC is to help moms reach their feeding goals in a safe and evidence-based way and, most importantly, to ensure that babies are fed, not forced to go hungry, and to listen and believe moms when they say they are not making enough milk! After all, the number 1 rule in lactation is to feed the baby, but that rule no longer applies. The rule is to breastfeed exclusively, at all costs. That was the price my baby had to pay, and I am determined to change that.
I was just beginning my career as a labor and delivery nurse when I became pregnant with my first child. According to our standard breastfeeding policies, all our patients were encouraged to breastfeed. It was common for patients to complain that they didn’t have enough milk, but we were taught this was “rare” as babies have small stomachs and need little colostrum. Because of this, I assured my patients that everything was fine.
There is a myth regarding a newborn’s stomach size that perpetuates the underfeeding of EBF babies, and now it is beginning to infiltrate formula-fed babies as well. The myth is found in every hospital and is not supported by current research. According to seven research articles, the stomach size of a term 7-pound baby ranges between 20 and 35 ml.

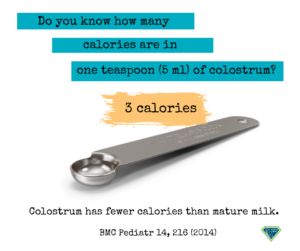
Another myth is that colostrum is all your baby needs. Note: One teaspoon of colostrum contains three calories. Feeding a newborn baby drops of colostrum is never enough for adequate feeding and fluids.
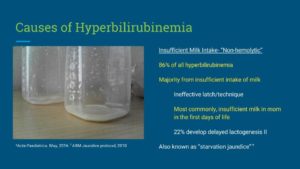
There is also a myth that low milk supply is rare.
Scientific Studies SHOW THAT DELAYED ONSET OF LACTOGENESIS II (DOLII), LACTATION DYSFUNCTION, AND LOW MILK SUPPLY (LMS) ARE COMMON.
After my first baby was born, I immediately began breastfeeding her, and everything seemed to be going well with latching and nursing, but she cried a lot, which was unsettling to me as I couldn’t comfort her. However, excessive crying was considered normal. (Note: Excessive crying is not normal) Gradually, my baby developed excessive jaundice, and the neonatologist was so concerned he recommended supplementing her with formula after nursing before we could be discharged. I tried to hand express, and all I could get was the tiniest clear drop, but the IBCLC said I probably didn’t respond to hand expression and told me I didn’t need to supplement because my baby’s bilirubin level wasn’t “too high.” Sadly, I followed the advice of the IBCLC. (Note: The IBCLC violated her Code of Professional Conduct and Scope of Practice, putting this baby in unsafe conditions without adequate nutrition and fluids and increasing bilirubin levels.)
That night, my baby did not sleep at all because she was crying. As I slept, my husband tried latching her onto my breasts as I was exhausted and falling asleep. In the morning, she was re-examined, and her bilirubin levels got worse, and she also lost a whopping 10 ounces! I was told by the neonatologist that I needed to supplement urgently.
With terror in my heart, I trembled, and I began supplementing right away. My baby finally stopped crying and slept for the first time.
I nursed and supplemented her every 2 hours because she was so hungry. However, another IBCLC and the breastfeeding support group I was in told me that supplementing my baby would hurt my supply, so I slowly eased her off the formula and began EBF again at one month old. (Note: supplementing does not decrease milk supply if adequate breast stimulation and milk removal are provided with every supplemental feeding.)
Even though I was finally exclusively breastfeeding, my baby would nurse every 15 minutes, and I would have maybe one 15-minute break all day when my husband took care of her. She would cry the whole time. Whenever she fed, I told myself it was “cluster feeding.” Her continuous feeding was good for my supply; I should keep it up.
Cluster feeding is another myth parents are taught when babies feed non-stop in the hospital. Find out what “cluster-feeding” really is here: cluster-feeding
I went to see another IBCLC, and she did a weighted feed. After feeding her, the weight didn’t change at all. The IBCLC said a mistake must have occurred, “that never happens.” She suggested I come back after another weighted feeding when my breasts were painfully full. At this weighted feeding, my baby had only gained one ounce, but I was only encouraged to continue exclusive breastfeeding because her weight was slowly going up. (Note: The IBCLC violated the Code of Professional Conduct and scope of practice. The baby was placed in unsafe conditions because of inadequate feeding. The baby should have been supplemented, and a feeding plan should have been implemented to improve milk supply while supplementing. Her pediatrician should have been notified; follow-up lactation appointments to monitor weight gain were essential.
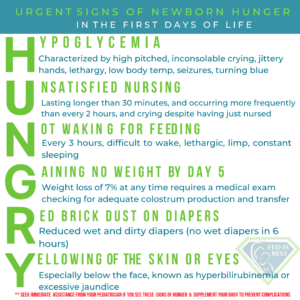
At nine weeks old, despite me constantly nursing her, her weight percentile dropped from the 76th percentile at birth to 7th. She had gone ten days without pooping; she even had a few brick dust diapers during the month of exclusive breastfeeding. At this point, I was at my breaking point. Both my baby and I were not thriving. I vividly remember reading the signs of HUNGRY on the Fed Is Best website in the middle of the night. I burst into tears knowing my baby had some of the symptoms and realized she was hungry!
There was no way to describe the guilt I felt. The truth is no mother can believe she wasn’t giving her baby enough milk when she was doing the “right” thing by exclusively breastfeeding. The result was that I had to suffer through the depths of the worst mom guilt hell.
The fact that she ate all the time was not normal. Still, many breastfeeding support groups said it was all normal (cluster feeding, baby can go two weeks without pooping, percentile charts are not accurate for breastfed babies, and some babies are just smaller, etc.).
These breastfeeding support groups are harming babies every day, and I shudder to think about how many babies are suffering from hunger or worse.
My pediatrician recommended I begin supplementing with formula again, and I finally decided I needed my baby to be happy and healthy. I began following the Fed’s Best Supplementation Guide and supplemented with 15cc at a time after breastfeeding both sides and using a slow-flow nipple when supplementing her. She gained five ozs in two days, was finally content and happy, and began sleeping better. Her weight gain percentiles began CLIMBING rapidly, and I was so relieved.
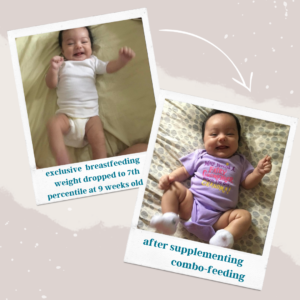
I am here to tell you it’s possible to successfully combo-feed your baby; I successfully combo-fed my baby until she was a year old, with 1/3 of the milk from my breasts, and the rest was life-saving infant formula.
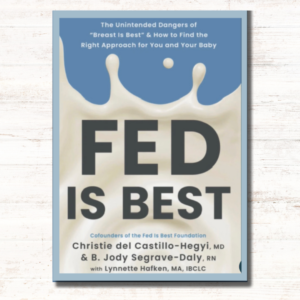
She has grown into a healthy, intelligent, beautiful girl in four years. I have since had two more children, and I have combined breastmilk with formula from the start. I still sometimes feel a pit in my stomach, wondering what would happen if I continued exclusively breastfeeding. I am so grateful to Fed is Best Foundation for helping me see the evidence that my baby was hungry.
Sarah F., RN, IBCLC
Dec 12, 2018 — The aim of this Scope of Practice is to protect the public by promoting that all IBCLC certificants provide safe, competent and evidence-based care
IBCLC Assessment, Diagnosis, and Referral
IBCLC Code of Professional Conduct
How can you help?
Send us your stories. Share with us your successes, your struggles, and everything in between. Every story saves another child from experiencing the same and teaches another mom how to feed her baby safely. Every voice contributes to change.