by Jody Segrave-Daly, Veteran NICU/Nursery nurse, IBCLC retired and Cofounder of the Fed Is Best Foundation
The standard of care for most hospitals, especially those who are Baby-Friendly certified, is that mothers stay with their baby after birth in their room, 24 hours a day, which is known as rooming-in.
Baby Friendly’s recent blog says that mothers have choices about nursery care in their Baby-Friendly certified hospitals; but then they say babies SHOULD stay in the room, no matter how they are being fed. This statement gives parents mixed messages and implies they don’t really have a choice at all. In many hospitals, it is not just implied; nurseries have been eliminated outright.
“Regardless of whether a mother is breastfeeding or formula feeding, they should room-in with their newborn.”
According to the World Health Organization, rooming in began as a way to promote early breastfeeding and to encourage bonding. Step 7 of the Ten Steps to Successful Breastfeeding calls for hospitals to “enable mothers and their infants to remain together and to practice rooming-in 24 hours a day.”
Despite the WHO’s 2017 expert panel’s finding that 24/7 rooming-in was ineffective at promoting sustained breastfeeding after discharge (but recommended it any way) and published tragedies of harmed infants while rooming-in, The World Health Organization and UNICEF continue to include rooming in for healthy newborns in the Ten Steps to Successful Breastfeeding policy.
Since adopting the rooming-in policy, inexcusable consequences such newborn falls from parent beds and near deaths and deaths from accidental suffocation while breastfeeding or doing skin-to-skin care (known as Sudden Unexpected Postnatal Collapse or SUPC) have skyrocketed, highlighting the urgent need for families to have access to nursery care.

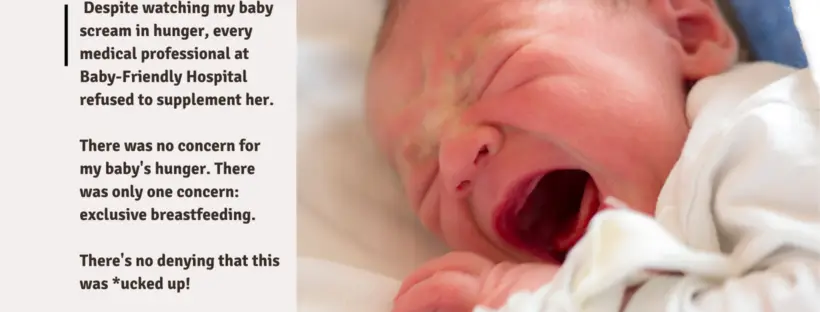
 My husband and I cried a lot during the first 24 hours at home. We fought to wake our sleepy newborn up, but we were rarely successful, and when we were, we couldn’t get him to eat. I kept on refusing to allow my husband to give our son any formula because I didn’t want it to ruin our breastfeeding relationship. We went to his newborn appointment when he was four days old. I knew at that point things weren’t going well but wasn’t prepared for the realities we were about to face. Our son had lost 13% of his body weight, he was hypothermic with a body temperature of 94.9, he was hypoglycemic, and had lost his reflexes. Our pediatrician looked at us with very sad eyes and kindly but firmly, explained our son was very sick and needed to eat now.
My husband and I cried a lot during the first 24 hours at home. We fought to wake our sleepy newborn up, but we were rarely successful, and when we were, we couldn’t get him to eat. I kept on refusing to allow my husband to give our son any formula because I didn’t want it to ruin our breastfeeding relationship. We went to his newborn appointment when he was four days old. I knew at that point things weren’t going well but wasn’t prepared for the realities we were about to face. Our son had lost 13% of his body weight, he was hypothermic with a body temperature of 94.9, he was hypoglycemic, and had lost his reflexes. Our pediatrician looked at us with very sad eyes and kindly but firmly, explained our son was very sick and needed to eat now.