Written by: Jody Segrave-Daly, MS, RN, IBCLC
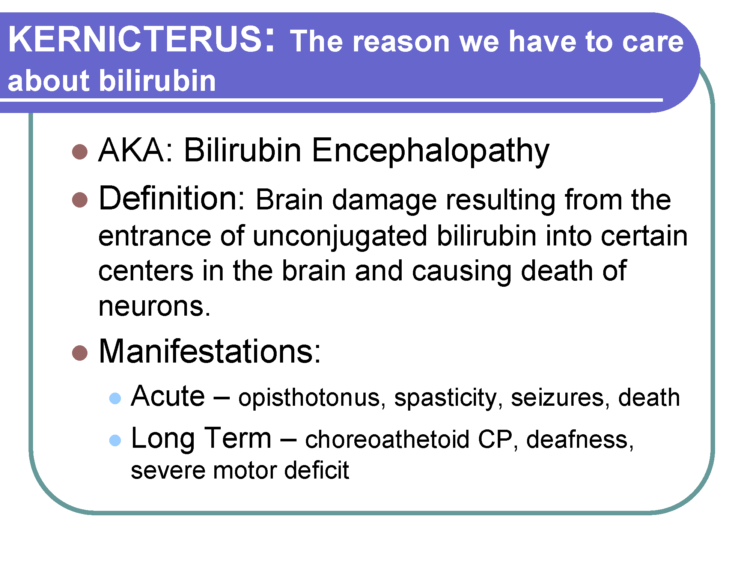
Cluster feeding is a phrase that is used to describe infant feeding behavior(s). Generally, it’s breastfeeding or bottle feeding that is in a different pattern from your baby’s typical feeding pattern. It is described as breastfeeding sessions or bottle-feeding sessions that are much shorter and more frequent, for 3-4 hours of the day. It often happens during a baby’s fussy period of the day. The Academy Of Breastfeeding Medicine defines cluster feeding as “several short feedings close together.” However, new mothers are being told constant and prolonged feeding around the clock in the hospital is “cluster feeding,” and this is where confusion that can result in harm begins. There is a point when cluster feeding becomes a clear sign of insufficient breast milk and/or insufficient transfer of milk, and those signs must be taken seriously for the health and safety of the infant. Mothers tell us they receive conflicting information and as a result, they become very frustrated, lose confidence and want to stop breastfeeding. Or, they persist with exclusive breastfeeding due to incorrect advice, and negative outcomes occur.
Cluster feeding is also a phrase that sometimes is also called “comfort-feeding.” As parents, we react to infant cries and feeding cues, so naturally, we will assume a baby is hungry and when we feed them, they will be satisfied. But some babies will snack and will not take a full feeding during their cluster-feeding time; this is normal. Some babies simply want to suckle on a pacifier after nursing or bottle feeding. This is because their bellies are full, but they want to suckle for soothing and not for feeding of milk. Some breastfeeding babies will suckle, using non-nutritive sucking patterns for soothing only. Some babies will also want to be held and snuggled or may want to be carried or want movement while suckling too!
Cluster feeding can also happen during growth spurts as well, but babies generally take in more milk during this time. It can also happen during times when a baby is not feeling well, teething or is tired or cranky. And it’s true—some babies don’t cluster feed at all. My exclusively breastfed babies never did and preferred sucking on a pacifier, after nursing for comfort.
When is cluster feeding considered normal?
- It happens after a mother’s full milk supply is in, after birth.
- It is during a limited time period of 3-4 hours in 24 hours.
- The breastfeeding mother has adequate milk supply.
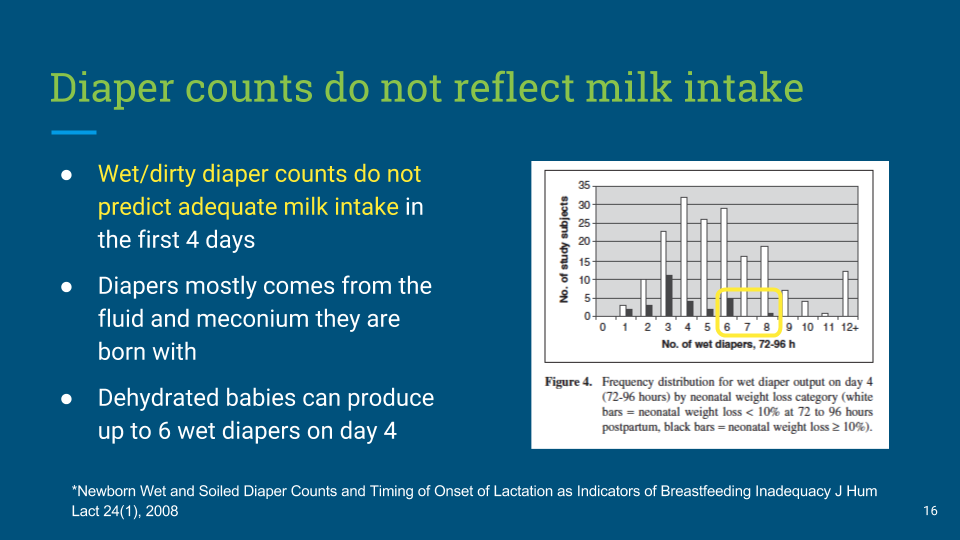
- Baby is having plenty of dirty and wet diapers.
- The baby is gaining enough weight.
If you are concerned that you are not making enough breast milk, or your baby isn’t transferring enough milk, you can do a simple check to see if you are.