Is that some kind of sick joke? Infant formula is safe nutrition—scientifically created to replace human milk and thus consists of fluids and nutrients necessary to nourish a baby. Brain damage is irreversible. That should be glaringly obvious, but it looks like the AAP Breastfeeding Section responsible for the recently released “Breastfeeding and the Use of Human Milk” (June 2022) has lost sight of this critical fact.
Let’s focus on this appalling statement:
“The need for phototherapy in an otherwise healthy infant without signs of dehydration and/or insufficient intake is not an indication for supplementation with formula unless the levels are approaching exchange transfusion levels.”
Hyperbilirubinemia (excessive jaundice) and Phototherapy
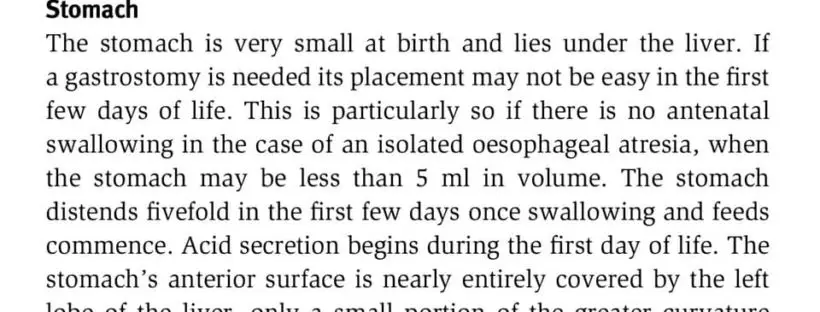
To explain why we are horrified, let’s look carefully at what the statement means. Jaundice is a common and usually benign condition experienced by about 60% of healthy newborns. It is caused by a substance called bilirubin, a breakdown product of fetal red blood cells after birth to transition to mature red blood cells. However, if a baby’s bilirubin levels are greater than a certain level and continue to climb, the risk for brain damage increases.