My husband and I were the happiest people on earth to have just welcomed our healthy baby boy Ian into the world [born in an Ottawa Baby-Friendly hospital]. We were anxious first time parents. We had taken all the prenatal classes. I read the book “What to Expect When You’re Expecting” and we felt well-informed to approach this new chapter in our lives. We made the decision that I would be breastfeeding as that was the “right” thing to do for our baby. My baby latched on automatically and the nurses were impressed with how he was eating because he fed about every hour and would feed for at least 45 minutes. I was nervous that I was not doing something right, and I continuously asked each and every nurse that came in to check on us if I was doing it right. I even asked them to just watch us while he fed and see if it was going okay. They all consistently replied, “You are doing great.”

Ian at 12 hours old.
The next morning came and I participated in a breastfeeding class held in the hospital by a lactation consultant (LC). The class had about 20 new moms with their babies there and the LC asked us to have our babies latch on and feed while she teaches and does her presentation. Again, Ian automatically latched to me and the LC was impressed and commented that I was like a pro already and that he latched perfectly and was doing well. I brought forward my concern to her as well, saying that he latches on about every hour or so for 45 min or more and she said, “That is great, he is a good eater!” About 30 min into the 1 hour class, all the other moms were sitting with their babies resting in their laps as they had all finished their feeding, but Ian was still latched onto me until the end of the class. The LC never brought anything up about the fact that if a baby is feeding for more than 30 minutes that means that they are probably not satisfied. Furthermore, I asked the LC if I could start pumping and she told me “no,” that I had to wait 6 weeks before pumping and giving him a bottle because otherwise he wouldn’t want to breastfeed anymore and it would disrupt our breastfeeding. So I kept my pump away as I was told, but this meant I had no idea how much milk I was producing (which later I found out was almost nothing).
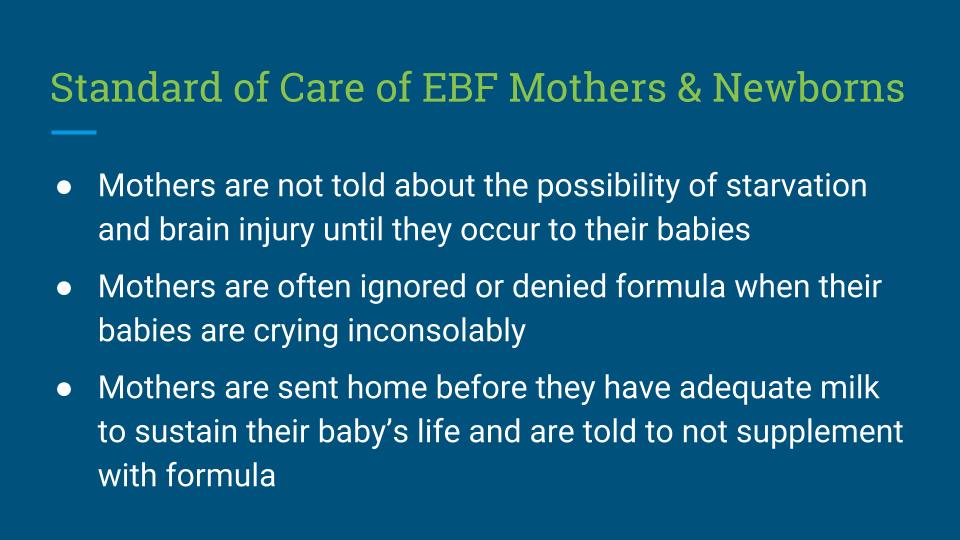
At 1 day old, I started to notice orange crystallization in his diaper, I panicked and right away asked the doctor what is happening. He told me, “Everything is normal; that is normal.” I kept exclusively breastfeeding and asked a nurse how I know he is getting enough milk from me, she replied “Don’t worry, their stomach is the size of a pea, they don’t need a lot.”
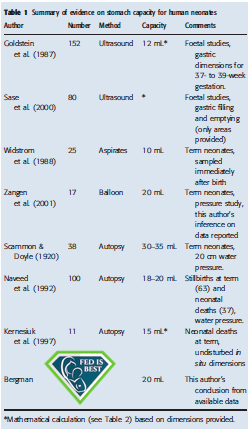
The newborn stomach is 20 mL or 2/3rds an ounce and empties during feeding to accommodate more milk.

Example of orange/red brick dust in a diaper, which is a sign of dehydration.
My baby was now 2 days old, and we were ready to be discharged. His coloring was becoming a little yellow, and the doctor told us that it was normal and it will pass. The diapers continued to have more orange crystallization; we were told that too would pass and was completely normal. I was asked if he had been having the correct number of diapers and he did have the correct number of diapers, but no one told me that the diaper had to be quite heavy for that to be applicable to normal health. There was no information on what a “normal” diaper means. As a new mom I had no experience with diaper changes or any idea of what to look for. All I could see is the orange crystallization in his diapers.
Upon discharge, they recorded his stats and it was not what we expected; his birth weight was 3962 grams and at discharge his weight was 3656 – we were concerned at the decrease in his weight and the doctor reassured us that this is normal and that up to 10% of weight loss in the first few days is normal and to just see a pediatrician within 3 days. We continued as we were advised and I continued to exclusively breastfeed.
At 5 days old we had our visit to the pediatrician, he checked Ian and advised me to start supplementing immediately as Ian had lost 17% of his birth weight and was jaundiced. I left that appointment heartbroken and feeling guilty that I was to blame for my baby’s suffering. We immediately rushed out, bought formula, and started to give it to him and he took it very well and became, what appeared to us, satisfied and sleepy. Thankfully to the dedication of his amazing pediatrician, he gave me a follow-up call that afternoon and asked how Ian was doing. He asked questions like, “Is he very sleepy? Almost lethargic?” I answered “Yes, Ian was sleepy and lethargic.” He asked if he had been given formula and I also answered yes to that. He very nicely and calmly advised me that he was quite concerned with the amount of weight that Ian had lost and that we should go right away to the nearest hospital to have him looked at again. I thanked him and we left immediately to get to the hospital.
He was admitted urgently for dehydration. This moment was the scariest time of my life, the doctor supplied 2 more bottles of formula (we were not allowed to give what we had, he had to have what the hospital supplied). I was holding him in my arms and he drank the one bottle while the doctor was present and then she left me to give him the second one and advised me to give him as much as he wanted.
After the doctor left, he finished the second bottle and was sleeping, but something was not right as he had this unusual rhythmic breathing pattern/hiccupping. I tried to wake him up, but his eyes did not open. Then all of a sudden his breathing stopped. I ran to the front desk area where I told a nurse, please help me – my baby is not breathing, and showed her how I lifted his hand and it just flopped down.
She automatically got on the phone and paged the doctors to come help. She ran him back to the room and laid him down on the bed. She tried to hit the bed beside him to wake him up and was shouting “baby wake up, baby wake up,” at which point my husband and I were in a frenzy of emotion and sadness as our child was not responding.
She gave him CPR and no response, then she started to cry! At this moment I thought everything was lost! It seemed like forever until the doctors came but then 5 doctors entered the room, they examined him and were whispering among themselves and we were just on the side watching our son not respond. He had to be put on life support and transferred to another hospital specializing in critical care for babies.
From Ian’s medical chart: Initial blood work showed a picture consistent with hypernatremic dehydration with a sodium of 158 mEq/L, chloride of 123 and glucose of 4.1 mmol/L (or 71 mg/dL). It was noted that Ian lost 17 percent of his birth weight. Baby developed multiple episodes where he stopped breathing with associated oxygen desaturations and therefore was intubated and put on mechanical ventilation. He had a partial septic work up and was started on IV antibiotics. A lumbar puncture or spinal tap was not done as the patient was felt to be too unstable. He was started on IV fluids with glucose.
From the minute we entered the new hospital, they offered me a pump and said that a lactation consultant would help me. I was very upset and sad and I explained that I did not want to breastfeed anymore, that breastfeeding is what brought my son here and he is now on life support because of it. They tried to reassure me and tell me that it was not my fault but I should still pump to keep my milk coming in. I was so hurt and confused, I wanted to provide ‘the best’ for my baby so I did try to pump that night! In a way it was good that I did, because that is the only way I really found out that I was starving my baby! I only had 2 mL of breast milk that had blood in it because my breasts were so raw from constant feeding (which I was told was normal). The next day, we made it clear that we did not want to have anything to do with breastfeeding anymore and we kindly asked that they do not bring it up again. Well, the nurses insisted! They kept harping on the fact that it is the best for the baby and that this is not my fault, etc.
It came to the point we had to yell at them to stop and to understand we want formula for our baby because attempting to exclusively breastfeeding pretty much killed him. They finally backed off from the breastfeeding comments!
Ian was continuously monitored in the NICU and the doctor who was in charge of him told us we need to wait and see how he responds to intensive care and medical treatments, and that we were lucky we went to the hospital when we did, otherwise Ian would not have survived. Thankfully, the wonderful medical professionals worked hard on bringing Ian’s health to a stable state after 5 days in NICU. This was a terrifying experience for us, it’s the worst thing to have to watch your child suffer knowing that you could have prevented it if we had just been given the correct information about exclusive breastfeeding risks!

Ian in the hospital after extubation (removal of his breathing tube), stabilized with intensive care.
I did write to the Ministry of Health in Ottawa, as well as to the CEO of the hospital in which Ian was born about what we went through in hopes of addressing the grave issues breastfeeding can cause. But their reply was all about breastfeeding support and the resources that are available regarding breastfeeding.
Our son is 4 years old now and growing well. That part of his life still haunts me, but I am grateful for each day I see his handsome smile, and I wish that no mom will ever have to go through something like I did. With our second child we were more experienced and fed her the way we felt was best for her, which was formula and now she is almost 2 years old. We are a happy family and thankful we were able to overcome that terrible time. We are grateful that our son was spared his life, but saddened that such situations are not as rare as we were led to believe and that still, babies are continuing to suffer.
My husband and I are looking forward to work for change in order to protect innocent babies from being victims of accidental starvation from restrictive breastfeeding policies. We are strong advocates and are working with the Fed Is Best Foundation. PLEASE join us and thousands of other families. 
For resources to safely breastfeed your baby : http://fedisbest.org/resources-for-parents/feeding-plan/
To donate to our non-profit Foundation : http://fedisbest.org/donate/
To join our world wide Fed Is Best Foundation Team: [email protected]


This is a very captivating and emotional story. I would have reacted the same where it one of my little girls. Thank you for sharing<3
I’m reading these nightmare stories from mothers and I can’t BELIEVE the nurses and doctors can be so ignorant !! It makes me so upset. I’m a nurse and I can’t imagine telling these moms that it’s ok and not give them formula!
Thank God I never experienced this because heads would be rolling by day one!
God bless all of you brave moms.
There’s nothing better than motherly instinct. You know your baby and when something just doesn’t seem right.
Thank you for your supportive words and encouragement (-:
I applaud you for sticking to your position and not continuing to breastfeed. I wish I’d done the same. I had no instinct telling me my baby was starving, but when he was readmitted to the hospital with dehydration and excessive weight loss, something told me this wasn’t going to go well and we’d be better off switching to full-time formula. I regret to this day letting the hospital staff talk me into “triple-feeding” and trying to ramp up my supply for the next two months. It made us all miserable and served no real purpose. Good for you for keeping the bullies out.
I gave birth at the civic 2 months ago, and when my baby lost 10% of birthweight in 24 hrs they had me pump and see an LC, but they also brought me formula to top up her next feed. After that I’d just page the nurse whenever she seemed to still be hungry. The nurses I had were very much on board with supporting breastfeeding but ultimately that fed is best. I was there 3 days and never denied or lectured on formula – I’m sure it’s partially staff dependent but at least one Ottawa hospital seems to be doing better, so your efforts are doing something !
Wonderful! We hope our campaign had something to do with that! We are so glad that your baby was safely fed!