by Christie del Castillo-Hegyi, M.D., Co-Founder of the Fed is Best Foundation
On September 22, 2017, senior members of the Fed is Best Foundation met with the top officials of the World Health Organization (WHO) Breastfeeding Program. We learned that the WHO has never studied the complications of the WHO Ten Steps to Successful Breastfeeding and the Baby-Friendly Hospital Initiative (BFHI). We learned they have no studies commissioned to monitor the complications. Despite being presented data on the complications caused by allowing newborns to fast for days to achieve exclusive breastfeeding, they declined our offer to help make the guidelines safer and more ethical. To watch the presentation given to the WHO officials, please go to this link. We learned that they have known about the risks of brain injury from exclusive breastfeeding and yet refuse to inform the public and health professionals. We learned that their provision for preventing brain injury consisted of telling health professionals to look out for “convulsions, lethargy and being unable to feed,” which are late signs of newborn brain injury. As a result, the WHO Ten Steps and the BFHI has created to an epidemic of infant feeding complications, hospitalizations, brain injury and disability in the developed and developing world. This constitutes one of the largest and most egregious violations of patient and human rights in the history of public health. They have asked for comments from the public regarding their draft revision of the breastfeeding guidelines, which make no changes to the recommendation, “give infants no food or drink other than breastmilk unless medically indicated,” while providing patients no information on the risks of avoiding supplementation. This is the official response of the Fed is Best Foundation to their request.
The Academy of Breastfeeding Medicine (ABM) recently published a revision of their supplementation protocol, which provides the criteria of the WHO’s BFHI to protect exclusive breastfeeding rates at discharge while providing guidelines for “medically-indicated” supplementation to prevent the known brain-threatening complications of underfeeding exclusively breastfed (EBF) newborns. The updated version of the guidelines unfortunately does not protect exclusively breastfed newborns from these complications as they in fact allow newborns to go past what is developmentally safe. They provide inadequate monitoring and prevention of hypoglycemia (low blood glucose), hyperbilirubinemia (excessive jaundice) and hypernatremia (high sodium from severe dehydration) and wait until late signs that herald the onset of brain injury to occur before testing for the conditions. They fail to fulfill the basic ethical obligation required of physicians and health care professionals to provide balanced and honest information on the common and serious complications associated with exclusive breastfeeding of newborns before copious milk production (lactogenesis II). In addition, many of the assumptions made by the ABM guidelines are based on logical fallacies that plague breastfeeding medicine. The entire system of feeding is based on the belief that babies can wait to be fully fed for days without consequence to their brain and vital organs and that supplementation is the cause of lactation failure rather than a reflection of a mother’s biological tendency to produce less milk and need to supplement. Unfortunately, it is not evident that experts in neonatal and pediatric neurology, neonatology nor pediatric endocrinology have been consulted in producing these guidelines as they appear to ignore the basic tenets of those disciplines. By denying much of the basic science of neonatal feeding and brain physiology, the ABM guidelines and the Baby-Friendly Hospital Initiative, which uses their guidelines, are operating blind to the dangerous conditions they allow newborns to be exposed to for the purpose of increasing rates of exclusive breastfeeding at discharge.
The Most Unsafe Aspects of the 2017 ABM Supplementation Criteria
- The guidelines operate with no awareness of the caloric content of colostrum nor the caloric requirements of newborns to prevent starvation and serious injury to the brain and vital organs.
- The ABM guidelines exclude healthy, term appropriately-sized exclusively breastfed newborns from being monitored for brain-threatening hypoglycemia when the scientific literature shows they are in fact at high risk for developing it.
- The ABM guidelines allow newborns with hypoglycemia as low as 40-45 mg/dL to remain uncorrected with IV glucose and supplementation despite the known risks of brain injury and reduced long-term academic achievement associated with those glucose levels. Their hypoglycemia guidelines even suggest that a glucose as low as 28 mg/dL may be tolerable within the first 2 hours of life.
- They state that 10% weight loss is not an automatic cause of supplementation without providing any research on what weight loss is in fact safe for a newborn. They allow a weight loss of 8-10% and suggest allowing greater than 10% weight loss at the same time that other research shows that brain-threatening complications occur by 7% weight loss. The guidelines require a newborn to exhibit signs of “significant dehydration including high sodium [hypernatremia], poor feeding and lethargy” to be supplemented, which are late signs of newborn starvation and brain injury.
- The threshold for supplementation to treat hyperbilirubinemia increases a child’s risk for brain injury and developmental disability.
- The ABM protocol and the BFHI guidelines recommend informing mothers of the risks of formula supplementation while making no mention of the risks of underfeeding, brain injury and disability from avoiding supplementation, a significant part of the protocol. Mothers are typically sent home before they have adequate milk supply to prevent feeding complications and are given no advice on how supplementation can prevent brain injury. For babies who are underfed, parents often find them lethargic or underweight, possibly brain-injured needing emergent hospitalization shortly after discharge.
- Even when babies develop brain-threatening complications that meet their criteria for “medical indication” for supplementation, they recommend restricted feeding volumes meant to emulate exclusive colostrum feeding, even when those restricted volumes are what typically lead to the child’s starvation-related complications.
The guidelines operate with no awareness of the caloric content of colostrum nor the caloric requirements of newborns to prevent starvation and serious injury to the brain and vital organs.
The ABM guidelines suggest that even if a mother has scant colostrum and suspects that it is insufficient to feed her one-day-old newborn, supplementation is not indicated.
“Careful attention to an infant’s early feeding cues, keeping the infant safely skin-to-skin with mother when she is awake, gently rousing the infant to attempt frequent breastfeeds, and teaching the mother hand expression of drops of colostrum, may be more appropriate than automatic supplementation after 6, 8, 12, or even 24 hours.”[1]
The guidelines arbitrarily believe that exclusively breastfed newborns can sustain up to 24 hours of being fed “drops” of colostrum before they experience starvation physiology and the associated brain injury without any way to monitor which baby will develop these complications, i.e. glucose monitoring. In fact, lactation consultants are commonly taught that it is acceptable for a healthy, term appropriately-sized newborns to go without a drop of milk for a full 24 hours without any data on safety. It appears that the ABM may not be aware of the number of calories contained in those drops of colostrum and how many calories are required to keep a newborn from starving and developing brain injury. The number of calories required to prevent newborn starvation is their basal metabolic rate, which is the number of calories required to keep all their living cells alive, including brain cells, over 24 hours. This daily caloric requirement is 100-120 Cal/kg/day.[2] This is the same requirement for every newborn whether they are breastfed or formula-fed from the first day of life throughout the newborn period. The protocol operates with no awareness of this caloric requirement nor the caloric content of the colostrum, which is 54 Cal/dL, which is in fact lower than the caloric content of mature breast milk (66-77 Cal/dL) and formula (66 Cal/dL), despite the widely perpetuated myth that it in fact has more calories.[3] The guidelines therefore operate with no awareness of the caloric yield of an average mother’s colostrum and arbitrarily declares virtually all colostrum to be enough without scientific evidence. In fact, the average mother produces about 55 mL of colostrum on the 1st day, then 185 mL on the 2nd day and 380 mL on the 3rd day.[4] This provides about 10%, then 33% then 66% of a 3 kg (6.5 lb) newborn’s daily caloric requirement, not meeting the full requirement until day 4 of life (see figures below).
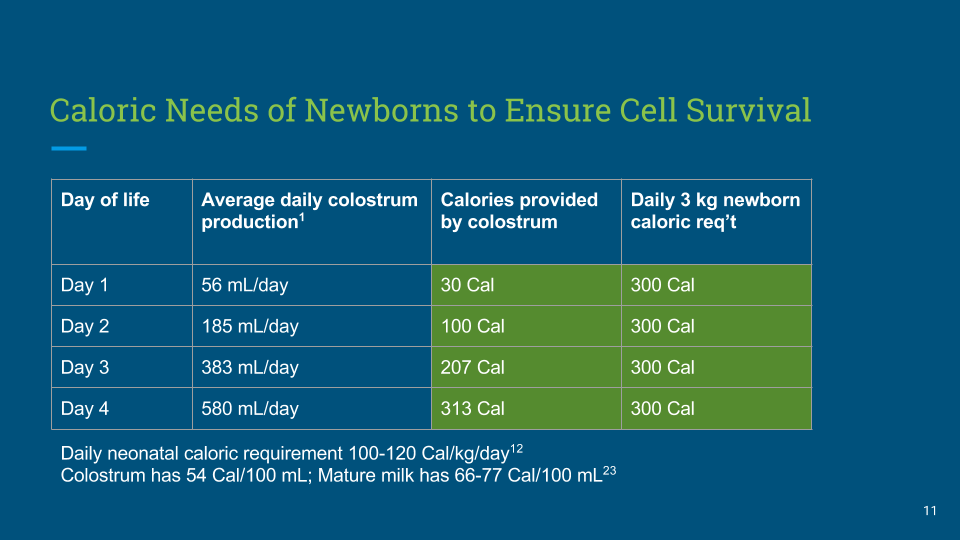
Figure 1. The average daily caloric yield of colostrum vs. the daily caloric requirement of a 3 kg (6.5 lb) newborn
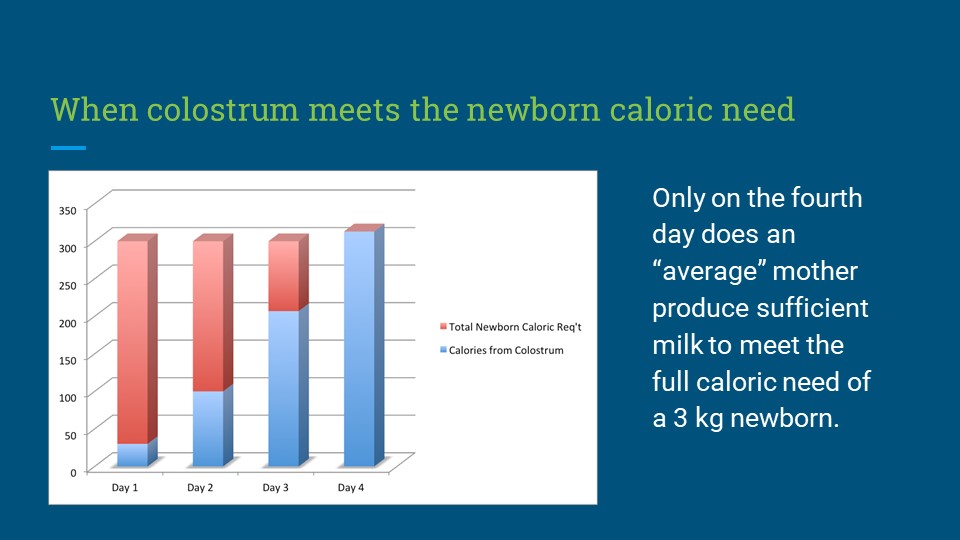
Figure 2. The caloric yield of exclusive colostrum feeding requires a newborn to fast for 3 days until a mother’s milk comes in. This is the reason why they experience “The Second Night Syndrome,” or severe hunger and thirst from the fasting conditions. This explains the rationale for near-universal supplementation in the first days of life by breastfeeding mothers prior to the WHO guidelines, even in the most remote locations.
This means that an average exclusively breastfed newborn is in fact fasting for first 3 days of life, which is the reason why they lose weight. It is also the reason why they cry and breastfeed non-stop and why mothers typically express concern about their babies not receiving enough milk in those first few days. The ABM states that small feedings as small as 2 mL per feed is sufficient to feed a one-day old newborn citing outdated and incorrect data that the one-day-old newborn stomach is 5-7 mL when in fact it is 20 mL+ by ultrasound and autopsy studies with an even larger capacity considering that the stomach empties into the intestines during feeds.[1,5] A ten-fold growth in stomach size and cellular metabolism over the course of 2-3 days is anatomically and physiologically impossible yet the BFHI has taught this to parents and health professionals while again providing no scientific evidence. In reality, only the newborn knows how depleted they are of calories and how many calories they require to prevent starvation. Newborns who are freely offered milk are known to easily take 30-60 mL per feeding regardless of the type of milk they receive every 2-3 hours, even on the first day of life, while rarely allowing themselves to lose greater than 7-8% of their birth weight when given free access to milk.[6] 30-60 mL feedings every 2-3 hours meets the full daily caloric requirement of most newborns of 2.7 oz/lb or 6 oz/kg, which is determined by the metabolism of their living cells, not the volume of colostrum their mother happens to produce.[2] If a mother’s colostrum volume is lower than average or her child has higher metabolic needs or has trouble extracting milk, her exclusively breastfed newborn will lose weight more rapidly. The fasting conditions imposed by the protocol quickly leads to catabolism, weight loss, extreme hunger and thirst in newborns and can lead to the starvation-related complications of hyperbilirubinemia, hypernatremia, dehydration and hypoglycemia if the child’s nutritional requirements are not met by the mother’s colostrum. The sooner her copious milk production arrives, the sooner her newborn is rescued from this fasting state. If a mother’s milk comes late (which happens to 22% of all mothers and 42% of first-time mothers) or comes in insufficient quantities, her baby is exposed to the brain-threatening complications of starvation if not supplemented.[7,8]
Normalizing Newborn Hunger and Distress
As a newborn’s glucose reserves decline, a newborn will exhibit distress through non-stop crying and nursing when breastfeeding is the only source of calories and fluid provided. These signs typically found in exclusively breastfed newborns by the second night of life is so common that the breastfeeding industry calls it, “The Second Night Syndrome,” the second night of fasting where babies are experiencing severe hunger and thirst while they still have enough reserve energy to cry.[9]
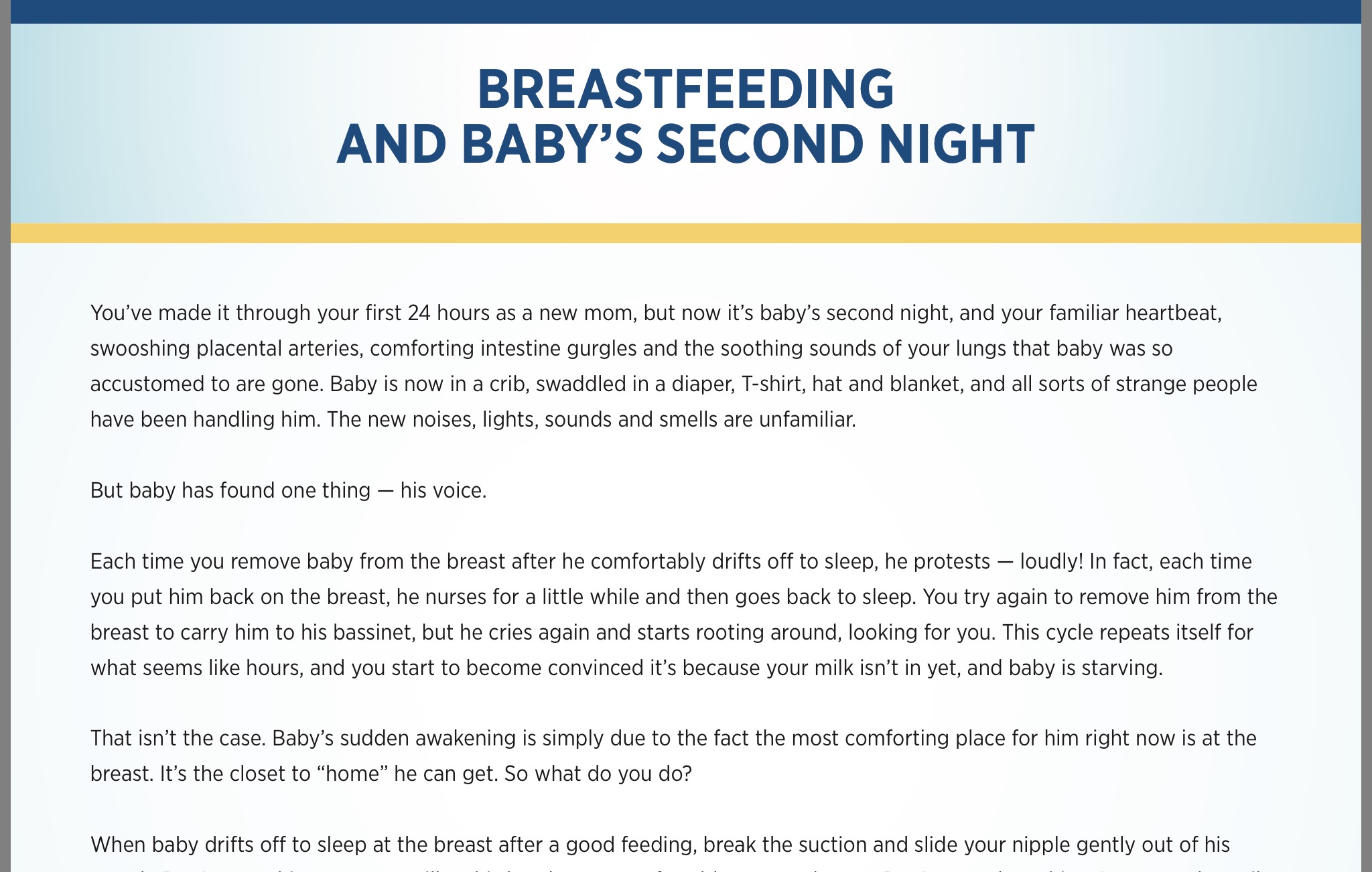
Figure 3. Patient information on the Second Night Syndrome from Lutheran Children’s Hospital.
The Baby-Friendly Hospital Initiative, through the ABM guidelines, up until this recent revision published after the widely publicized death of an exclusively breastfed newborn at a Baby-Friendly hospital, has taught health professionals and mothers that fussing and constantly nursing for hours are not reasons or supplementation.[1,10] These hours of fussing and nursing are obvious signs of hunger and distress present before the development of brain-threatening levels of hypoglycemia, dehydration and jaundice.[11,12,13] The 2017 guidelines made revisions to this section given that fussing and “constantly feeding for several hours” leading to maternal fatigue and newborn lethargy have led to newborn starvation-related complications, hospitalizations and rare deaths from severe dehydration and accidental suffocation.[14,15]
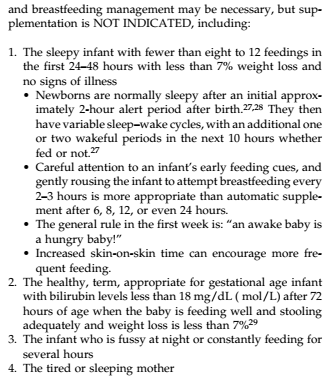
Figure 4. Academy Breastfeeding Medicine 2009 for when supplementation is NOT indicated. “Constantly feeding for several hours” leading to a “tired or sleeping mother” have led to newborn hospitalizations and deaths from accidental starvation and suffocation.
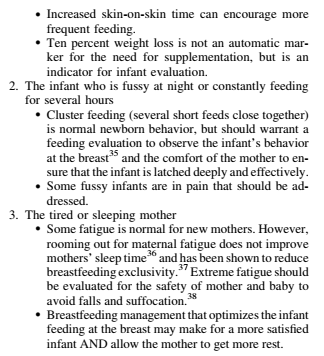
Figure 5. 2017 ABM BFHI guidelines revision on when supplementation is NOT indicated. “Constantly feeding for several hours” is still included as a reason to NOT supplement. However, cluster feeding has been defined as several short feeds and now they recommend evaluation of infant behavior at the breast and latch before recommending supplementation. Fussy infants are noted to possibly be in pain but not noted to possibly be hungry.
For decades, the Baby-Friendly Hospital Initiative has actively taught health professionals through their in-hospital training that this non-stop “fussing” and nursing is the biological norm and that it is to be tolerated as a necessary step in getting a mother’s milk to come in on the misguided premise that making a newborn subsist on a fraction of their caloric requirement through exclusive colostrum feeding is a requirement for successful breastfeeding. [16] Therefore a newborn’s only way to communicate distress through crying is no longer biologically protective because his mother and health professionals are told that the crying does not mean hunger or that breast milk is insufficient. In reality, if a mother’s breasts do not produce sufficient milk to rescue the child from their fasting state, the child will develop dehydration, hypoglycemia, hyperbilirubinemia and hypernatremia, which can cause injury to the brain and vital organs.[17,18,19] While a mother is told that the signs of hunger and starvation are normal, she is not told about the risks of the brain-threatening complications of starvation if her child does not in fact receive enough milk.[20] Once the child is sufficiently depleted of calories and fluid, the child will stop crying and may in fact look sleepy and satisfied to sleep-deprived parents or well-meaning health professionals, when in fact, the child is experiencing abnormal brain function from these abnormalities.[21] Within hours, if a child does not receive sufficient milk, the child will become lethargic and unresponsive and soon thereafter, vitals signs will begin to fail.[22] By the time a child is lethargic or unresponsive, the scientific literature has shown that they have already likely sustained devastating levels of brain injury that lead to long-term disability.[23] These complications would have been prevented had the mother been told the whole truth about the risks of exclusively breastfeeding newborns, the signs of starvation and its consequences.
The Baby-Friendly Hospital Initiative’s policy to hide these common and dangerous complications of early exclusive breastfeeding hospitalizes thousands of babies a year in the U.S. alone, and millions more in the rest of the world, complications that can result in long-term developmental disability that cannot be reversed once the child reaches a critical threshold.[24,25]
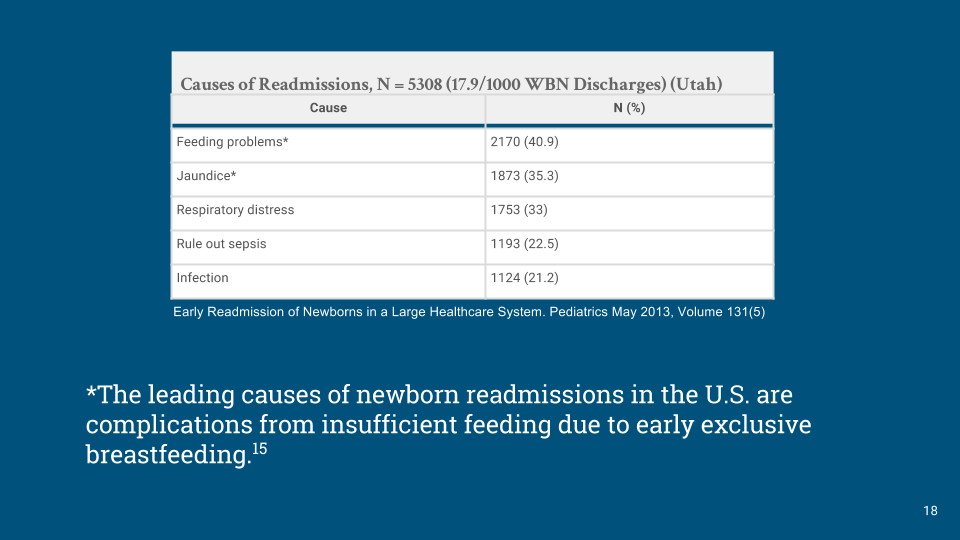
Figure 6. Data from a large Utah Healthcare System showing the leading causes of newborn readmissions were for feeding complications and jaundice.[26]
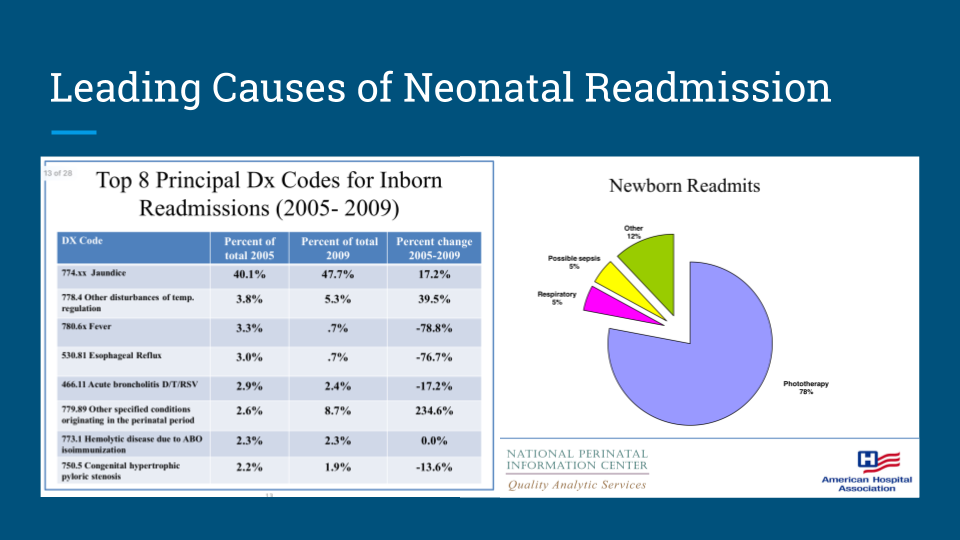
Figure 7. Data from the American Hospital Association showing the leading cause of neonatal readmissions were for jaundice and that among all neonatal readmitted patients, 78% received phototherapy.[27]
The Baby-Friendly Hospital Initiative is based on the inconclusive belief that the ideal, most advantageous form of feeding for all babies is what Western breastfeeding advocates have idealized as absolute exclusive breastfeeding from birth, when in fact the historical world breastfeeding data shows that breastfeeding mothers, even in the most remote locations of the world, near-universally supplemented breastfeeding, particularly in the first days of life to prevent starvation and death. Pre-BFHI data showed that doctors in the developing world also understood this important physiology as they supplemented breastfeeding to prevent the complications of dehydration, hypoglycemia and jaundice, which now are among the leading causes of newborn hospitalizations in the world.[71]
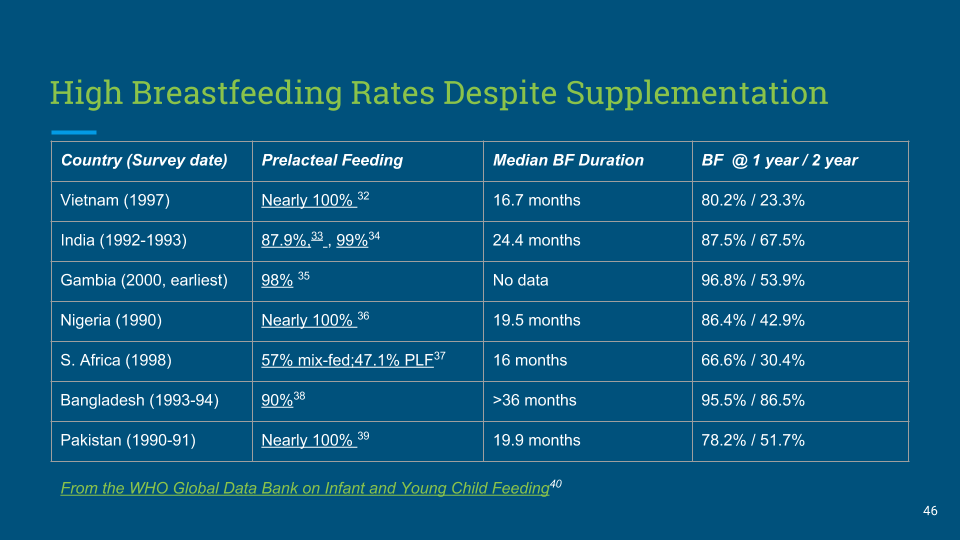
Figure 8. Pre-lacteal feeding was used near-universally by breastfeeding mothers before the WHO guidelines to prevent starvation-related complications in the first days of life. Despite that, babies were commonly breastfed to 1-2 years of age.[34-43]
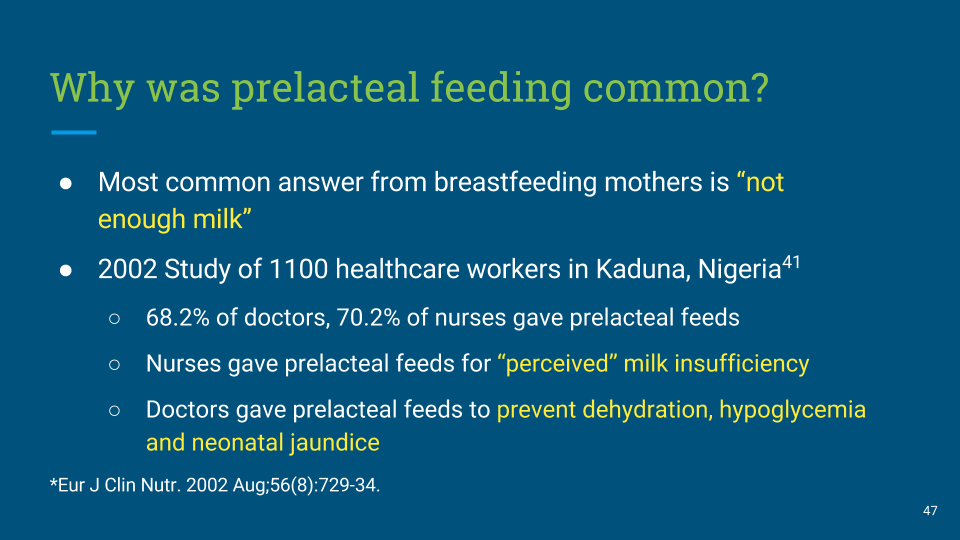
Figure 9. Pre-lacteal feeding or supplementation before full breast milk production were commonly used by mothers and nurses because breast milk was not enough. Doctors gave these supplemental feeds to prevent dehydration, hypoglycemia and jaundice, the most common complications of early exclusive breastfeeding.[71]

Figure 10. Jaundiced newborns requiring phototherapy in Vietnam. Provided by Firefly. [44] Hospitalizations for newborn jaundice have risen steadily since the 1991 introduction of the Baby-Friendly Hospital Initiative. 1.1 million newborns a year develop severe jaundice (>20 mg/dL), the majority caused by “dehydration” or underfeeding from early exclusive breastfeeding.[24,30] 114,000 of those newborns will die from their severe jaundice, the majority in resource-poor countries with insufficient health care resources to monitor the complications of exclusive breastfeeding. As a result excessive jaundice or hyperbilirubinemia, the majority from dehydration related to exclusively breastfeeding, is now the leading cause of newborn hospitalization and perinatal disability in the world.[25]
The ABM guidelines exclude healthy, term appropriately-sized exclusively breastfed newborns as not “at risk” for hypoglycemia when the scientific literature shows they are in fact at high risk.
‘Small quantities of colostrum are appropriate for the size of a newborn’s stomach, to prevent hypoglycemia in a healthy, term, appropriate for gestational age infant”[1]
The calculated caloric yield of exclusive colostrum feeding makes the above statement written by the ABM an incorrect and impossible statement. A child who receives a fraction of their caloric requirement though exclusive colostrum feeding for days while burning extra calories from hours of crying and nursing tolerated by the Baby-Friendly protocol is necessarily going to become hypoglycemic. In fact a recent study published from the U.K.’s National Health Service data showed that exclusive breastfeeding is an independent variable that predicts hospitalization for neonatal hypoglycemia.[45]
In a recent study of healthy, term well-latched exclusively breastfed (EBF) newborns strictly following the BFHI protocol showed that 10% experience hypoglycemia < 40 mg/dL by 6 hours of life when screened for 48 hours, the most affected being first-born babies, affecting 23%.[46] Babies are commonly born depleted of calories as they are often born to fasted mothers and can experience stressful deliveries that deplete their caloric reserve further. In addition, an average mother’s colostrum does not actually meet their full caloric requirement (see Figures 1 and 2). In fact, in a study of newborns without symptoms universally screened within 3 hours of life for low blood sugar or hypoglycemia, a marker of depleted caloric reserve, 19% developed developmentally deleterious low glucose levels of < 45 mg/dL and 10% developed glucoses < 40 mg/dL, including healthy, term, appropriately-sized newborns.[47] A glucose of < 45 mg/dL in these babies with no symptoms despite aggressive correction was associated with 38% declines in passing the standardized test in literacy at 10 years of age. This same study showed that a glucose of < 40 mg/dL was associated with 50% declines in passing the literacy and math test..
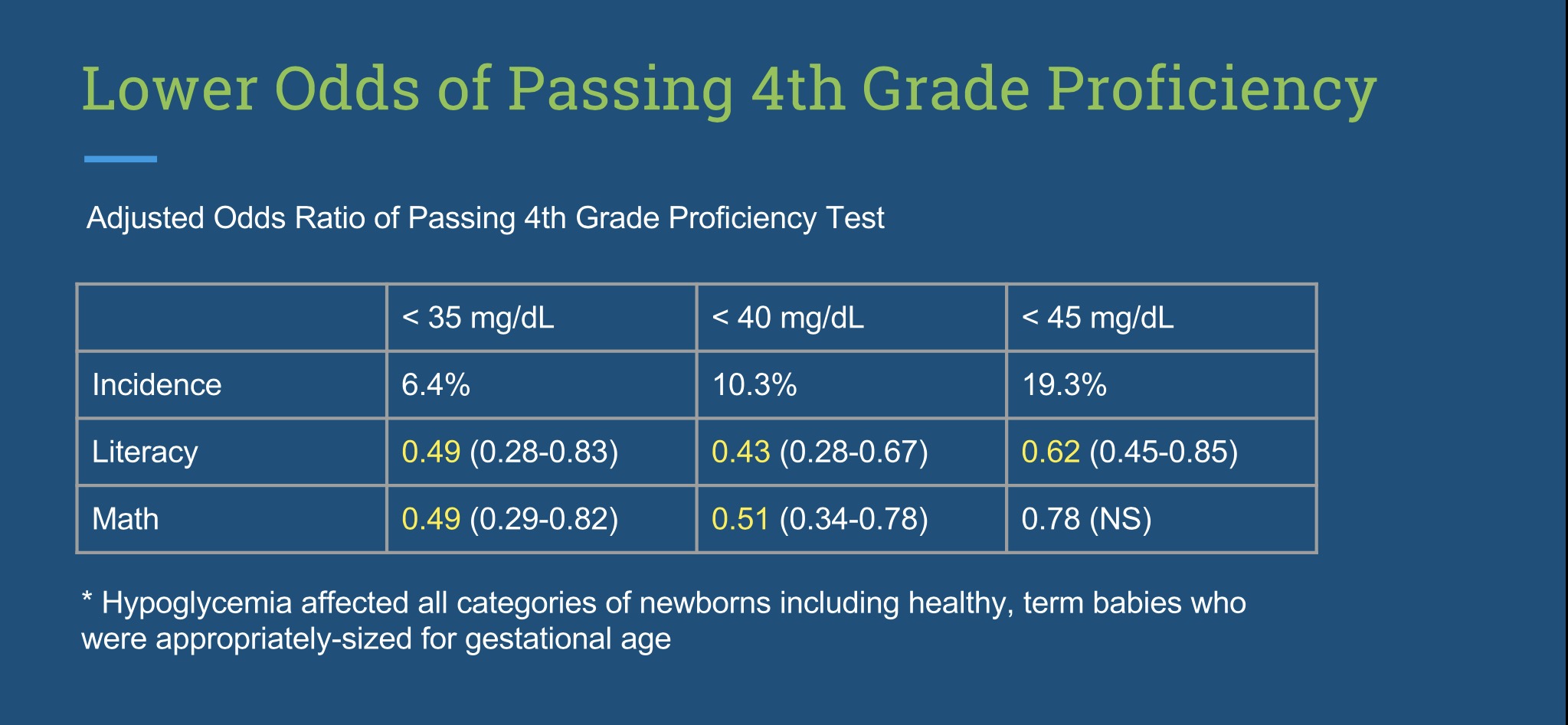
Figure 11. Decreased rates of passing 4th grade (10-year-old) literacy and math tests among hypoglycemic newborns and relative incidences of hypoglycemia among universally-screened newborns without symptoms.[49]
At this time, the standard of care allows at least 10% of healthy EBF newborns to be exposed to hypoglycemia that will reduce their lifetime academic achievement because they receive no glucose monitoring and therefore no protection from this dangerous condition until it is too late.[49] They may go days experiencing hypoglycemic brain injury while waiting for their mother’s milk to arrive in the hospital and at home until they are finally hypoglycemic enough to exhibit lethargy or seizures. This recent data on the long-term outcomes of babies who experience hypoglycemia in the first hours of life appears to be absent from the ABM guidelines.[1,49]
Furthermore, even if a child is rapidly diagnosed with hypoglycemia with a bedside glucose monitor, they require laboratory confirmation to allow supplementation.[1,49] When hypoglycemia kills thousands of brain cells within minutes of diagnosis, to allow a child’s glucose to remain uncorrected for the 30 minutes minimum it takes to confirm hypoglycemia with a laboratory test, the policy exposes newborns to lifelong disability that can easily be prevented or minimized with immediate correction. A newborn can easily lose their vital signs from hypoglycemia within this time frame. The belief that supplementation with formula is more dangerous than hypoglycemia is misguided, unsafe and negligent.
The ABM guidelines allow newborns with hypoglycemia as low as 40-45 mg/dL to remain uncorrected with IV glucose and supplementation despite the known risks of brain injury and reduced long-term academic achievement associated with those glucose levels. They suggest glucose levels as low as 28 mg/dl may also be acceptable.
According the 2017 ABM guidelines indications to supplement:
“Asymptomatic hypoglycemia, documented by laboratory blood glucose measurement (not bedside screening methods) that is unresponsive to appropriate frequent breastfeeding [defined in the ABM Hypoglycemia guidelines as <40 mg/dL]. Note that 40% dextrose gel applied to the side of the infant’s cheek is effective in increasing blood glucose levels in this scenario and improves the rate of exclusive breastfeeding after discharge with no evidence of adverse effects. Symptomatic infants or infants with glucose <1.4 mmol/L (<25 mg/dL) in the first 4 hours or <2.0 mmol/L (<35 mg/dL) after 4 hours should be treated with intravenous glucose.”[1]
The ABM Hypoglycemia Protocol suggests that hypoglycemia as low as 28 mg/dL in the first 2 hours may not require correction:[49]
“…given the known lower plasma glucose levels in healthy term breastfed infants as compared with formula-fed infants, the low thresholds [for hypoglycemia] for exclusively breastfed infants might even be lower. Table 1 gives recommendations for this timed threshold approach.”
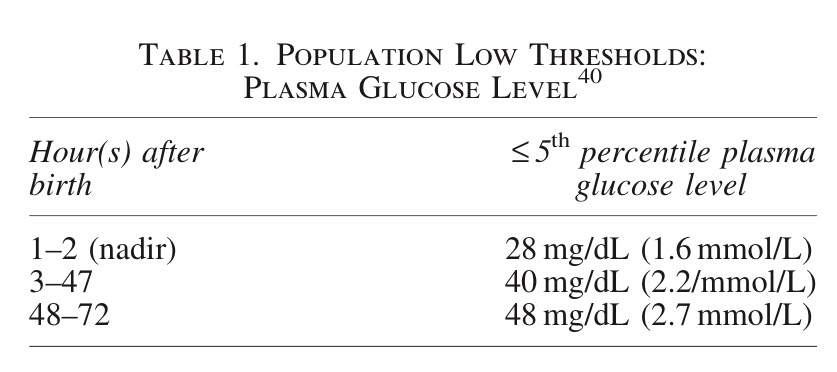
Figure 12: Suggested acceptable levels of hypoglycemia for breastfed newborns increase the risk of permanent brain injury and lower academic achievement.[49]
The ABM supplementation guidelines also suggest that oral dextrose is sufficient to correct hypoglycemia when stabilization of hypoglycemia typically requires ad lib supplementation of milk, either formula or safe, tested donor milk as well as IV glucose.[1] Babies with significant hypoglycemia are depleted of caloric reserve and will not only need enough calories to meet the minimum metabolic need but also enough glucose, protein and fat to restore the fuel reserves that were depleted from the fasting conditions commonly found after delivery and during early exclusive breastfeeding. Furthermore, if an already starved newborn is developing excessive jaundice, the protein and fat in milk are required to remove bilirubin, which would not be provided by oral dextrose.[33,52]
Unless the ABM believes that exclusive breastfeeding at discharge is more important than a child’s long-term cognitive potential, we advise they change these recommendations immediately. In fact, the most educated experts in hypoglycemia, the Pediatric Endocrine Society, recommends a glucose of no lower than 50 mg/dL in the first 48 hours and no lower than 60 mg/dL thereafter.[52] The brain begins to signal the body to increased glucose levels between 50 and 60 mg/dL in order to protect itself from injury. Since injury to the brain has devastating effects to a child’s future potential, the brain’s preference should be honored. In fact keeping a child’s glucose as far away from the hypoglycemic threshold within the normal range is the most important way we can protect the newborn brain. We do that by making sure a newborn is adequately fed. Nature has designed a nearly perfect mechanism for ensuring that the brain experiences no interruptions in fuel delivery–a newborn’s cry and a mother’s instinct to feed her child in whatever way she can to prevent her child from suffering hunger and thirst. The entire purpose of the BFHI protocol is to prevent this protective phenomenon from occurring and it has harmed and hospitalized millions of babies for the 26 years it has defined the standard of care.
They state that 10% weight loss is not an automatic cause of supplementation without providing any research on what weight loss is in fact safe for a newborn. The threshold for supplementation requires a newborn to exhibit signs of significant dehydration including high sodium, poor feeding and lethargy.
According to the 2017 ABM guidelines on supplementation:
Indications NOT TO SUPPLEMENT:
“The infant who is fussy at night or constantly feeding for several hours. Cluster feeding (several short feeds close together) is normal newborn behavior, but should warrant a feeding evaluation to observe the infant’s behavior at the breast and the comfort of the mother to ensure that the infant is latched deeply and effectively. Some fussy infants are in pain that should be addressed.”
“Weight loss of ‡8–10% (day 5 [120 hours] or later), or weight loss greater than 75th percentile for age. 1. Although weight loss in the range of 8–10% may be within normal limits if all else is going well and the physical examination is normal, it is an indication for careful assessment and possible breastfeeding assistance. Weight loss in excess of this may be an indication of inadequate milk transfer or low milk production, but a thorough evaluation is required before automatically ordering supplementation.”
Indications for possible supplementation include:
“Clinical or laboratory evidence of significant dehydration (e.g., high sodium, poor feeding, lethargy, etc.) that is not improved after skilled assessment and proper management of breastfeeding.”[1]
All three brain-injuring complications of hypoglycemia, hypernatremia and hyperbilirubinemia have been documented to occur before 10% weight loss.[53,54,55] In fact, they seem to be unaware that the original research done that established 10% weight loss as “normal” and presumably “safe” was done on 7 exclusively breastfeed newborns showing the maximum weight loss experienced was 10%.[56] A study this small would not be sufficient to prove “safety” of 10% weight loss. This study failed to report on the glucose, sodium or bilirubin levels of those babies and failed to perform evaluation of long-term neurological outcomes to see if any of them experienced brain injury from the fasting conditions of early exclusive breastfeeding. No research since has been done using standardized developmental testing to prove that 10% weight loss is in fact safe. In fact the only such research on the neurological outcomes of babies who lost > 12%, while showing no differences in the overall developmental score between dehydrated and non-dehydrated newborns, the study did show evidence of increased rates of developmental delay in the dehydrated babies developing lower fine motor coordination, higher parental concerns for speech delay, shyness, allergies and disabilities.[57]
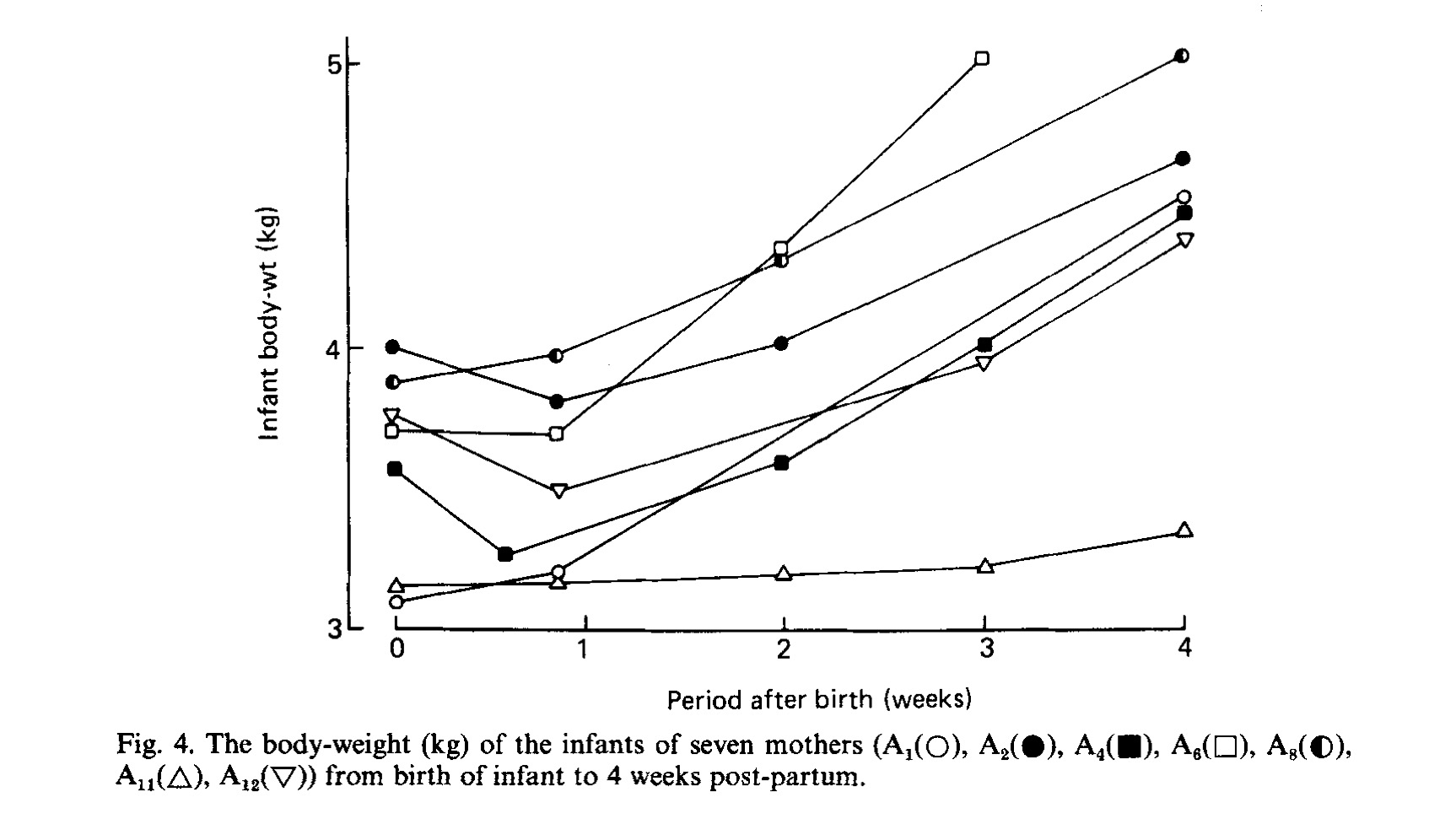
Figure 13. Weight loss patterns of 7 exclusively breastfed babies that originally established the 10% weight loss threshold as “safe.”[57]
At this time, the scientific literature has shown that exclusively breastfed newborns can develop developmentally unsafe levels of bilirubin and hypernatremia by a weight loss percent of 7%, which became the updated maximum recommended weight loss of the American Academy of Pediatrics in their 2013 breastfeeding guidelines.
More than 50% of babies experiencing hypernatremia of > 150 mEq/dL have abnormal development by 12 months of age and 95% of hypernatremia of > 145 mEq/dL occurs by 7% weight loss.[58,59] In addition, developing 4% weight loss by 24 hours and 7% weight loss by 48 hours predicts the development of high bilirubin of > 15 mg/dl, which has been shown in multiple studies to increase the risk of developmental disabilities.[60-65] According to the largest study of weight loss patterns of exclusively breastfed newborns (or nomogram) from a large Baby-Friendly hospital system, which included over 100,000 babies, more than half of all exclusively breastfed newborns experience greater than 7% weight loss,[66] which means more than half are at risk for developmentally unsafe hyperbilirubinemia or hypernatremia.[28] The ABM refers to the recently developed Newborn Weight Loss Tool, which is a useful tool to pick up excessive or accelerated weight loss in an exclusively breastfed newborn.[66] The ABM suggests an arbitrary threshold of > 75% percentile weight loss for age on this nomogram as “excessive” weight loss when we in fact have no data from that research at what percentile weight loss newborns are experiencing developmentally deleterious conditions that result in brain injury. The data is not tied to information on newborn bilirubin, sodium or glucose levels nor long-term neurological outcomes. We have no way of telling whether the threat of brain injury begins at the 75th or 50th or 85th percentile. In fact, it is not possible for science and statistics to know the precise moment when an individual child goes from hungry to starving and brain injured as that threshold is different for every baby. Since every child is born with different caloric reserve, percent weight loss is in fact an imprecise way of detecting and preventing starvation. Only the baby knows how close they are to empty and the data on the incidence of newborn hypoglycemia suggests that they can reach “empty” at any weight loss percent.[24,46,47]
The recent article documenting brain injury from hypoglycemia showed that hypoglycemia in healthy, term exclusively breastfed newborns occurred at ANY weight loss, from 0-16%.[23] The most sensitive system that nature has created to detect and prevent starvation is the cry of a newborn and the maternal instinct to feed her baby to prevent distress. When that instinct is suppressed by policies aimed at preventing supplementation, the least-fed exclusively breastfed babies will cross the starvation threshold and can be found lethargic from caloric and fluid deprivation. The consequences of crossing that threshold is permanent and devastating to that child and family.
The threshold for supplementation to treat hyperbilirubinemia or jaundice increases a child’s risk for brain injury and developmental disability
From the 2017 ABM Supplementation Protocol:
“Indications for supplementation:
- Jaundice of the newborn associated with poor breast milk intake despite appropriate intervention. This characteristically begins at 2–5 days and is marked by ongoing weight loss, limited stooling and voiding with uric acid crystals [“red brick dust” in diapers].
- Breast milk jaundice when levels reach 340–425 lmol/L (20–25 mg/dL) in an otherwise thriving infant and where a diagnostic and/or therapeutic interruption of breastfeeding may be under consideration. First line diagnostic management should include laboratory evaluation, instead of interruption of breastfeeding.”[1]
From the ABM Jaundice protocol:
“Supplementation with expressed breast milk, banked human milk, or formula (in that order of preference) should be limited to infants with at least one of the following:
- A clear indication of inadequate intake as defined by weight loss in excess of 10% after attempts to correct breastfeeding problems.
- Failure in milk production or transfer adjusted for duration of breastfeeding and documented by pre- and post feeding weights after attempts to increase milk production and milk transfer.
iii. Evidence of dehydration defined by significant alterations in serum electrolytes, especially hypernatremia, and/or clinical evidence of significant dehydration (poor skin turgor, sunken fontanelle, dry mouth, etc.).”[32]
A newborn child has to be starving to meet medical indication for supplementation according to the ABM guidelines. Furthermore, the guidelines allow a newborn to reach a bilirubin of 20-25 mg/dL in cases of breast milk jaundice before supplementation is offered when the peer-reviewed literature on newborn hyperbilirubinemia bilirubin levels has shown increased levels of markers of brain injury present in the blood by a bilirubin level of greater than 17 mg/dL, which accelerates at a bilirubin of 19 mg/dL.[67,69] In fact, bilirubin levels of above 15 mg/dL has been used as the cut-off for moderate hyperbilirubinemia and has been shown to increase the risk of multiple long-term developmental disabilities including ADHD, seizure disorders, cerebral palsy, long-term declines in academic achievement and abnormalities in language, motor, sensory, behavioral and cognitive development associated with Bilirubin-Induced Neurological Disorder (BIND).[60-65] Allowing a child’s bilirubin to reach a level of 20 mg/dL is unsafe as the hyperbilirubinemia literature has not differentiated between newborns who experience breast milk jaundice versus starvation jaundice. In fact, a 30-year follow-up study on severely jaundiced newborns showed that newborns with bilirubin above 19.9 mg/dL showed that 45% of those newborns had long-term neurobehavioral problems, had higher rates of ADHD, difficulty with math and reading, inability to complete high school and college, joblessness and alcoholism compared to non-jaundiced newborns.[70] The ABM has again ignored the scientific data in order to protect its primary objective, achieving high EBF rates at discharge, a quality marker which, in itself, has inconclusive benefit to long-term breastfeeding success, while having known harms to exclusively breastfed newborns.
The ABM protocol and the BFHI guidelines recommends informing mothers of the risks of formula supplementation while excluding discussion of the risks of brain injury and disability from avoiding supplementation.
“Hospitals should strongly consider formulating and instituting policies to require a medical provider’s order when supplements are medically indicated and informed consent of the mother when supplements are not medically indicated. It is the responsibility of the healthcare provider to fully inform parents of the benefits and risks of supplementation, document parental decisions, and support the parents after they have made a decision.”[1]
The guidelines thoroughly inform mothers of the risks of formula based on conflicting data riddled with confounding variables and make no mention of the brain- and life-threatening complications associated with early exclusive breastfeeding in order to gain compliance from mothers. In fact, the ABM does not even discuss the risks brain injury and disability from avoidance of supplementation in their own document intended to inform health providers.[1] Therefore, health professionals, particularly those with less medical training, are left to enforce the guidelines oblivious to the risks of leaving a crying exclusively breastfed newborn underfed. Similarly, by hiding the risks of avoiding supplementation and only discussing the risks of formula, mothers are coerced to accept the risks of the Baby-Friendly protocol by agreeing to exclusively breastfeed. They are left with no information on the signs of newborn starvation, which are normalized by the protocol, and no awareness of the increased risk of brain injury caused by avoiding supplementation when attempting to exclusively breastfeed until the complications occur to their babies. Health providers are ethically mandated to provide complete information on risks associated with health decisions, regardless of how rare, so that a patient may have full autonomy to decide for their child in order to reduce risk of harm. The risks of early exclusive breastfeeding are well-known and make up the leading causes of newborn hospitalizations, which health professionals have been witnessing for decades.[24-28] These health professionals are commonly reprimanded for defying the Baby-Friendly rules when they offer supplementation even if it can save a child from suffering and from hospitalization. They literally have to wait for the complications to occur. For a child to suffer complications and permanent injury due to underfeeding in our modern era, even in the most privileged of settings, is a catastrophic evolution of infant feeding.
Even babies that meet medical indication for supplementation are given restricted feedings meant to emulate what limited calories are provided by colostrum not the metabolic requirements of the newborn to prevent and correct starvation.
Even when a newborn meets medical indication for supplementation, a point at which a newborn is at risk for brain injury if not freely supplemented, the ABM’s focus is still on restricting formula feeding so that breastfed infants get as little formula as possible, even if that formula can save their brain and life. The calories allotted by what they consider as “normal” feeding volumes provide as little as 4 to 66% of a 3 kg newborn’s daily caloric requirement the first 3 days of life.[1]
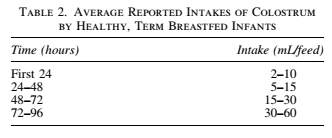
Figure 14. Recommended volumes of supplementation for when medical indication for supplementation exists. Medical indication occurs when a newborn become depleted of calories and fluid and are experiencing life-threatening metabolic abnormalities consistent with starvation. This “normal” intake provides 4-66% of an average 3 kg newborn’s caloric requirement (based on the know caloric content of colostrum of 54 Cal/100 mL) and therefore will perpetuate and worsen a newborn’s fasting state.
They recommend these same volumes for already starved newborns even if those volumes led to the starvation-related complications the newborn developed. So for babies who are already experiencing brain-threatening complications that could be quickly reversed with ad lib feeding, if health professionals follow the guidelines for formula supplementation volumes, they are in fact perpetuating the fasting physiology that resulted in the complications. It appears that no one at the ABM looked at how many calories colostrum actually feeds a child and therefore they are unable to consider that colostrum may not in fact be enough for the majority of newborns. Because they are unable to consider the possibility that they were incorrect in their estimation of colostrum, which nearly all experienced breastfeeding mothers in the developing world felt was insufficient [72] before the La Leche League and the WHO declared it as “enough,” exclusively breastfed babies are enduring days of hunger and thirst in hospitals and at home while the least-fed are experiencing life-long disability and even death.
1.1 million newborns a year experience severe jaundice, one of the leading causes of preventable long-term disability in the world, the majority caused by underfeeding.[25] 114,000 newborns die form that severe jaundice every year.[26] The majority occur in South Asia and Sub-Saharan Africa where few hospital services exist to monitor and treat hyperbilirubinemia in exclusively breastfed newborns, which was previously prevented by mother-led supplementation. The Baby-Friendly protocol in settings where breastfeeding is the only viable option for infant feeding and breastfeeding rates are already high has done nothing to promote breastfeeding. It has only made it more perilous by teaching mothers that there is no such thing as not enough breast milk and no consequences to allowing a child to wait to be fully fed.
In conclusion
The Fed is Best Foundation is appalled by the lack of concern that the WHO has shown for the millions of newborns and infants that have been hospitalized for jaundice, dehydration, hypoglycemia and failure to thrive, many of whom have suffered permanent declines in cognitive development, disability and death. It is shameful that a health organization would prioritize their policy over human lives and withhold information from parents that can save their child’s life and future. (The full account of this meeting reported here.)
We hope that health professionals and parents all over the world reject and protest the WHO’s recommendation to prioritize exclusive breastfeeding over infant safety and instead support and encourage Safe Breastfeeding. Safe Breastfeeding is the breastfeeding that generations of mothers practiced before the WHO BFHI. Safe Breastfeeding prioritized feeding over exclusivity in breastfeeding. Safe Breastfeeding fed babies breast milk to the best of each mother’s ability then supplemented freely until every baby was satisfied to prevent suffering and harm. Safe Breastfeeding breastfed and supplemented generations of babies and allowed them to reach their full potential by making sure their body and brains were fed enough calories and fluid to remain intact. Safe Breastfeeding did not exclude babies of mothers with insufficient breast milk from reaching their full potential because they could be protected from starvation as well. Safe Breastfeeding mostly required common sense and compassion along with a little wisdom passed on from experienced parents on breastfeeding and recognizing a hungry baby. Before the BFHI, breastfeeding did not require millions of dollars in breastfeeding goods and services, laboratory monitoring, office visits, phototherapy or neonatal ICUs to make it safe because exclusive breastfeeding was not the goal. Having a safely fed baby was the goal. At one point, mothers knew the dangers of infant starvation as every living creature has known from the dawn of time. The BFHI has erased that knowledge from the collective knowledge of breastfeeding mothers and continues to do so every day that it spreads across the globe. In the developed and developing world, the least-fed exclusively breastfed babies continue to suffer serious harm because the WHO has chosen to hide the realities of starvation to promote its objective of making formula the enemy of infant feeding. Meanwhile, mothers and their babies are left defenseless against the true threat to a newborn’s health and future potential, hunger and thirst.
Celebrate Safe Breastfeeding and all Safe Infant Feeding as all safe infant feeding sustains life and preserves human potential. Support every mother to feed her child the best way she can as only she and her baby can know.
#FedisBest
The WHO is accepting comments on these draft guideline revisions until October 24, 2017. The Foundation urges health care providers, parents, and the public to demand that the WHO not place exclusive breastfeeding before infant safety in their guidelines and commit to informing parents of the real risks of insufficient feeding. Comments can be made on the WHO BFHI comments page or emailed to contact@fedisbest.org, to be forwarded to the WHO.
Send Comments to WHO before Oct 24
Please sign this petition to demand that the WHO make preventing newborn brain injury and death from their breastfeeding guidelines a priority.
Sign Our WHO PetitionWe believe all babies deserve to be protected from hunger and thirst every single day of their life and we believe that education on Safe Infant Feeding should be free. If you would like to make a donation to support the Fed is Best Foundation’s mission to teach every parent Safe Infant Feeding, please consider making a one-time or recurring donation to our organization.
Thank you from the Fed is Best Foundation.
References
- Kellams, A., Harrel, C., Omage, S., Gregory, C. & Rosen-Carole, C. ABM Clinical Protocol #3: Supplementary Feedings in the Healthy Term Breastfed Neonate, Revised 2017. Breastfeed Med 12, 188–198 (2017).
- Ben, X.-M. Nutritional management of newborn infants: Practical guidelines. World Journal of Gastroenterology 14, 6133 (2008).
- Gidrewicz, D. A. & Fenton, T. R. A systematic review and meta-analysis of the nutrient content of preterm and term breast milk. BMC Pediatrics 14, 216 (2014).
- Neville, M. C. et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am. J. Clin. Nutr. 48, 1375–1386 (1988).
- Bergman, N. J. Neonatal stomach volume and physiology suggest feeding at 1-h intervals. Acta Paediatr. 102, 773–777 (2013).
- Miller JR, Flaherman VJ, Schaefer EW, Kuzniewicz MW, Li SX, Walsh EM, Paul IM. Early weight loss nomograms for formula fed newborns. Hosp Pediatr. 2015 May;5(5):263-8. doi: 10.1542/hpeds.2014-0143. PubMed PMID: 25934810.
- Dewey, K. G., Nommsen-Rivers, L. A., Heinig, M. J. & Cohen, R. J. Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics 112, 607–619 (2003).
- Chantry, C. J., Nommsen-Rivers, L. A., Peerson, J. M., Cohen, R. J. & Dewey, K. G. Excess weight loss in first-born breastfed newborns relates to maternal intrapartum fluid balance. Pediatrics 127, e171-179 (2011).
- Second night syndrome by kellymom: https://kellymom.com/ages/newborn/bf-basics/second-night/
- Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol #3: hospital guidelines for the use of supplementary feedings in the healthy term breastfed neonate, revised 2009. Breastfeed Med 4, 175–182 (2009).
- Committee on Fetus and Newborn & Adamkin, D. H. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics 127, 575–579 (2011).
- Unal, S., Arhan, E., Kara, N., Uncu, N. & Aliefendioğlu, D. Breast-feeding-associated hypernatremia: retrospective analysis of 169 term newborns. Pediatr Int 50, 29–34 (2008).
- Gourley, G. R. Breast-feeding, neonatal jaundice and kernicterus. Semin Neonatol 7, 135–141 (2002).
- Boskabadi, H. et al. Long-Term Neurodevelopmental Outcome of Neonates with Hypernatremic Dehydration. Breastfeed Med (2017). doi:10.1089/bfm.2016.0054
- Becher, J.-C., Bhushan, S. S. & Lyon, A. J. Unexpected collapse in apparently healthy newborns–a prospective national study of a missing cohort of neonatal deaths and near-death events. Arch. Dis. Child. Fetal Neonatal Ed. 97, F30-34 (2012).
- Baby Friendly Hospital Initiative Guidelines: https://www.ncbi.nlm.nih.gov/books/NBK153487/
- Burns, C. M., Rutherford, M. A., Boardman, J. P. & Cowan, F. M. Patterns of cerebral injury and neurodevelopmental outcomes after symptomatic neonatal hypoglycemia. Pediatrics 122, 65–74 (2008).
- Wisnowski, J. L., Panigrahy, A., Painter, M. J. & Watchko, J. F. Magnetic resonance imaging of bilirubin encephalopathy: current limitations and future promise. Semin. Perinatol. 38, 422–428 (2014).
- Ünver Korğalı, E., Cihan, M. K., Oğuzalp, T., Şahinbaş, A. & Ekici, M. Hypernatremic Dehydration in Breastfed Term Infants: Retrospective Evaluation of 159 Cases. Breastfeed Med 12, 5–11 (2017).
- Steube, A. Of goldilocks and neonatal hypernatremia. https://bfmed.wordpress.com/2016/01/31/of-goldilocks-and-neonatal-hypernatremia/
- JUST ONE BOTTLE WOULD HAVE KEPT MY BABY OFF LIFE SUPPORT: THE FAILURE OF BABY-FRIENDLY (BFHI) CARE IN CANADA. http://fedisbest.org/2017/03/just-one-bottle-would-have-kept-my-baby-off-life-support-the-failure-of-bfhi-care-in-canada/
- IF I HAD GIVEN HIM JUST ONE BOTTLE, HE WOULD STILL BE ALIVE.By Jillian Johnson. http://fedisbest.org/2017/02/given-just-one-bottle-still-alive/
- Seske, L. M., Merhar, S. L. & Haberman, B. E. Late-Onset Hypoglycemia in Term Newborns With Poor Breastfeeding. Hosp Pediatr 5, 501–504 (2015).
- Olusanya BO, Osibanjo FB, Mabogunje CA, Slusher TM, Olowe SA. The burden and management of neonatal jaundice in Nigeria: A scoping review of the literature. Niger J Clin Pract. 2016 Jan-Feb;19(1):1-17.
- Olusanya BO, Ogunlesi TA, Kumar P, Boo NY, Iskander IF, de Almeida MF, Vaucher YE, Slusher TM. Management of late-preterm and term infants with hyperbilirubinaemia in resource-constrained settings. BMC Pediatr. 2015 Apr 12;15:39.
- Young PC, Korgenski K, Buchi KF. Early readmission of newborns in a large health care system. Pediatrics. 2013 May;131(5):e1538-44. doi: 10.1542/peds.2012-2634. Epub 2013 Apr 8. PubMed PMID:23569092
- Janet H. Muri, Nancy Crawford, Bonnie Connors Jellen, Director Maternal and Child Health American Hospital Association, Washington, DC. Reducing Avoidable Obstetrical and Neonatal Readmissions. http://www.aha.org/content/11/PerinatalReadmissionscall1.pdf
- Flaherman, V. J. et al. Early Weight Loss Nomograms for Exclusively Breastfed Newborns. PEDIATRICS 135, e16–e23 (2015).
- Kuzniewicz MW, Greene DN, Walsh EM, McCulloch CE, Newman TB. Association
Between Laboratory Calibration of a Serum Bilirubin Assay, Neonatal Bilirubin
Levels, and Phototherapy Use. JAMA Pediatr. 2016 Jun 1;170(6):557-61. - Lee BK, Le Ray I, Sun JY, Wikman A, Reilly M, Johansson S5. Haemolytic and nonhaemolytic neonatal jaundice have different risk factor profiles. Acta Paediatr. 2016 Dec;105(12):1444-1450.
- Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol #22: guidelines for management of jaundice in the breastfeeding infant equal to or greater than 35 weeks’ gestation. Breastfeed Med. 2010 Apr;5(2):87-93.
- Sarici D, Gunes T, Yazici C, Akin MA, Korkmaz L, Memur S, Kurtoglu S, Ozturk
MA, Sarici SU. Investigation on malondialdehyde, S100B, and advanced oxidation
protein product levels in significant hyperbilirubinemia and the effect of
intensive phototherapy on these parameters. Pediatr Neonatol. 2015
Apr;56(2):95-100. - American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 114, 297–316 (2004).
- Hoa DP, Thanh HT, Höjer B, Persson LA. Young child feeding in a rural area in the Red River delta, Vietnam. Acta Paediatr. 1995 Sep;84(9):1045-9. PubMed PMID: 8652957.
- Srivastava SP, Sharma VK, Kumar V. Breastfeeding pattern in neonates. Indian Pediatr. 1994 Sep;31(9):1079-82. PubMed PMID: 7883365.
- Hasan J, Khan Z, Sinha SN. Socio-cultural factors influencing nutritional status of infants — a longitudinal study. Indian J Matern Child Health. 1991;2(3):84-6. PubMed PMID: 12346054.
- Semega-Janneh IJ, Bøhler E, Holm H, Matheson I, Holmboe-Ottesen G. Promoting breastfeeding in rural Gambia: combining traditional and modern knowledge. Health Policy Plan. 2001 Jun;16(2):199-205. PubMed PMID: 11358922.
- Davies-Adetugbo AA. Sociocultural factors and the promotion of exclusive breastfeeding in rural Yoruba communities of Osun State, Nigeria. Soc Sci Med. 1997 Jul;45(1):113-25. PubMed PMID: 9203276.
- Delport SD, Bergh AM, Hay IT. Breast-feeding practices in a private maternity hospital. S Afr Med J. 1988 Oct 15;74(8):396-9. PubMed PMID: 3187818.
- Islam MA, Nielsen CC. Maternal and child health services: evaluating mothers’ perceptions and participation. Public Health. 1993 Jul;107(4):243-9. PubMed PMID: 8356206.
- Ashraf RN, Jalil F, Khan SR, Zaman S, Karlberg J, Lindblad BS, Hanson LA. Early child health in Lahore, Pakistan: V. Feeding patterns. Acta Paediatr Suppl. 1993 Aug;82 Suppl 390:47-61. PubMed PMID: 8219467.
- WHO Global Data Bank on Infant and Young Child Feeding http://www.who.int/nutrition/databases/infantfeeding/countries/en/
- Akuse RM, Obinya EA. Why healthcare workers give prelacteal feeds. Eur J Clin Nutr. 2002 Aug;56(8):729-34. PubMed PMID: 12122548.
- Photograph of newborns receiving phototherapy from Firefly.
- Dassios, T., Greenough, A., Leontiadi, S., Hickey, A. & Kametas, N. Admissions for hypoglycaemia after 35 weeks of gestation: perinatal predictors of cost of stay. J. Matern. Fetal. Neonatal. Med. 1–19 (2017).
- Samayam P, Ranganathan PK, Kotari UD, Balasundaram R. Study of Asymptomatic
Hypoglycemia in Full Term Exclusively Breastfed Neonates in First 48 Hours of
Life. J Clin Diagn Res. 2015 Sep;9(9):SC07-10. - Kaiser JR, Bai S, Gibson N, Holland G, Lin TM, Swearingen CJ, Mehl JK,
ElHassan NO. Association Between Transient Newborn Hypoglycemia and Fourth-Grade Achievement Test Proficiency: A Population-Based Study. JAMA Pediatr. 2015
Oct;169(10):913-21. doi: 10.1001/jamapediatrics.2015.1631. - UN Declaration of Human Rights: http://www.un.org/en/universal-declaration-human-rights/.
- Wight, N., Marinelli, K. A. & Academy of Breastfeeding Medicine. ABM clinical protocol #1: guidelines for blood glucose monitoring and treatment of hypoglycemia in term and late-preterm neonates, revised 2014. Breastfeed Med 9, 173–179 (2014).1.
- Burns, C. M., Rutherford, M. A., Boardman, J. P. & Cowan, F. M. Patterns of cerebral injury and neurodevelopmental outcomes after symptomatic neonatal hypoglycemia. Pediatrics 122, 65–74 (2008).
- Bertini, G., Dani, C., Tronchin, M. & Rubaltelli, F. F. Is breastfeeding really favoring early neonatal jaundice? Pediatrics 107, E41 (2001).
- Thornton PS, Stanley CA, De Leon DD, Harris D, Haymond MW, Hussain K,
Levitsky LL, Murad MH, Rozance PJ, Simmons RA, Sperling MA, Weinstein DA, White
NH, Wolfsdorf JI; Pediatric Endocrine Society: Recommendations from the
Pediatric Endocrine Society for Evaluation and Management of Persistent
Hypoglycemia in Neonates, Infants, and Children. J Pediatr. 2015
Aug;167(2):238-45. doi: 10.1016/j.jpeds.2015.03.057.. - Salas, A. A. et al. Significant weight loss in breastfed term infants readmitted for hyperbilirubinemia. BMC Pediatr 9, 82 (2009).
- Uras N, Karadag A, Dogan G, Tonbul A, Tatli MM. Moderate hypernatremic dehydration in newborn infants: retrospective evaluation of 64 cases. J Matern Fetal Neonatal Med. 2007 Jun;20(6):449-52.
- Yang WC, Zhao LL, Li YC, Chen CH, Chang YJ, Fu YC, Wu HP. Bodyweight loss in predicting neonatal hyperbilirubinemia 72 hours after birth in term newborn infants. BMC Pediatr. 2013 Sep 21;13:145. doi: 10.1186/1471-2431-13-145.
- Neville, M. C. et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am. J. Clin. Nutr. 48, 1375–1386 (1988).
- Escobar, G. J. et al. Five-year neurodevelopmental outcome of neonatal dehydration. J. Pediatr. 151, 127–133, 133.e1 (2007).
- Uras, N., Karadag, A., Dogan, G., Tonbul, A. & Tatli, M. M. Moderate hypernatremic dehydration in newborn infants: retrospective evaluation of 64 cases. J. Matern. Fetal. Neonatal. Med. 20, 449–452 (2007).
- Koklu, E. et al. A review of 116 cases of breastfeeding-associated hypernatremia in rural area of central Turkey. J. Trop. Pediatr. 53, 347–350 (2007).
- Bhutani, V. K. & Johnson-Hamerman, L. The clinical syndrome of bilirubin-induced neurologic dysfunction. Semin Fetal Neonatal Med 20, 6–13 (2015).
- Wei CC, Chang CH, Lin CL, Chang SN, Li TC, Kao CH. Neonatal jaundice and
increased risk of attention-deficit hyperactivity disorder: a population-based
cohort study. J Child Psychol Psychiatry. 2015 Apr;56(4):460-7. doi:
10.1111/jcpp.12303. Epub 2014 Jul 24. PubMed PMID: 25056274. - Ricardo-Garcell J, Harmony T, Porras-Kattz E, Colmenero-Batallán MJ,
Barrera-Reséndiz JE, Fernández-Bouzas A, Cruz-Rivero E. Epileptic encephalopathy
in children with risk factors for brain damage. Epilepsy Res Treat.
2012;2012:747565. doi: 10.1155/2012/747565. Epub 2012 Jul 12. PubMed PMID:
22957240; PubMed Central PMCID: PMC3420497. - Andrade E, Araujo Júnior E, Rolo LC, Costa Fda S. Risk factors for cerebral
palsy in premature infants identified during the pre and perinatal periods: a
case-control study. Minerva Ginecol. 2016 Feb;68(1):29-36. Epub 2014 Nov 21.
PubMed PMID: 25415488. - Maimburg RD, Olsen J, Sun Y. Neonatal hyperbilirubinemia and the risk of
febrile seizures and childhood epilepsy. Epilepsy Res. 2016 Aug;124:67-72. doi:
10.1016/j.eplepsyres.2016.05.004. Epub 2016 May 19. PubMed PMID: 27259071. - Wusthoff CJ, Loe IM. Impact of bilirubin-induced neurologic dysfunction on
neurodevelopmental outcomes. Semin Fetal Neonatal Med. 2015 Feb;20(1):52-57. doi:10.1016/j.siny.2014.12.003. Epub 2015 Jan 10. Review. PubMed PMID: 25585889;
PubMed Central PMCID: PMC4651619. - Newborn weight loss tool – https://www.newbornweight.org/
- Sarici D, Gunes T, Yazici C, Akin MA, Korkmaz L, Memur S, Kurtoglu S, Ozturk
MA, Sarici SU. Investigation on malondialdehyde, S100B, and advanced oxidation
protein product levels in significant hyperbilirubinemia and the effect of
intensive phototherapy on these parameters. Pediatr Neonatol. 2015
Apr;56(2):95-100. doi: 10.1016/j.pedneo.2014.06.006. Epub 2014 Sep 26. PubMed
PMID: 25261050. - Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol #22: guidelines for management of jaundice in the breastfeeding infant equal to or greater than 35 weeks’ gestation. Breastfeed Med 5, 87–93 (2010).
- Okumus, N. et al. Tau and S100B proteins as biochemical markers of bilirubin-induced neurotoxicity in term neonates. Pediatr. Neurol. 39, 245–252 (2008).
- Hokkanen, L., Launes, J. & Michelsson, K. Adult neurobehavioral outcome of hyperbilirubinemia in full term neonates—a 30 year prospective follow-up study. PeerJ 2, e294 (2014).
- Akuse, R. M. & Obinya, E. A. Why healthcare workers give prelacteal feeds. Eur J Clin Nutr 56, 729–734 (2002).

5 thoughts on “Why the Academy of Breastfeeding Medicine Guidelines for “Medically Necessary” Supplementation Make the Baby-Friendly Hospital Initiative Unsafe”