Christie del Castillo-Hegyi, M.D., Co-Founder of the Fed is Best Foundation
In response to a letter written by 1000 Days director, Lucy Martinez-Sullivan and follow-up editorial from Kimberly Seals Allers, we wanted to take an opportunity to set the record straight.The mission of the Fed is Best Foundation is to protect infants from complications and injuries resulting from accidental starvation under currently promoted breastfeeding policies. In order to protect infant safety and ensure the patient and human rights of mothers and babies, we have built a non-profit organization committed to: (1) the study of exclusive breastfeeding complications that can result in brain injury and, in the most severe instances, death; and (2) raising public awareness to signs of infant hunger and the consequences that can result based on peer-reviewed research.
As part of our public health awareness commitment, the Fed is Best Foundation has developed and compiled extensive resources for parents and health professionals to promote safe breastfeeding and safe infant feeding policies based on evidence, including, the science of infant feeding, the caloric and fluid requirements of newborns and the caloric yield of exclusive breastfeeding. These core matters of infant feeding are shockingly absent from current breastfeeding curricula and protocols. Our Foundation is not against breastfeeding; it is for safe breastfeeding and close monitoring to prevent complications and injuries to infants reported in the medical literature, the media and by the thousands of mothers who have sent us their stories, which we receive each and every day.
In order to advance this mission, we have firmly stood against the dangerous policy of “giving infants no food or drink other than breast milk unless medically indicated,” a core recommendation of the World Health Organization’s (WHO) Baby-Friendly Hospital Initiative (BFHI), which guides management of exclusively breastfed newborns in hospitals. The peer-reviewed scientific literature has shown that by the time the “medical indication” for supplementation has been reached, a child is at increased risk of brain injury, if not, already brain-injured. This brain injury is irreversible and causes developmental delays and disability, which organizations like the Academy of Breastfeeding Medicine and the American Academy of Pediatrics acknowledge as true.
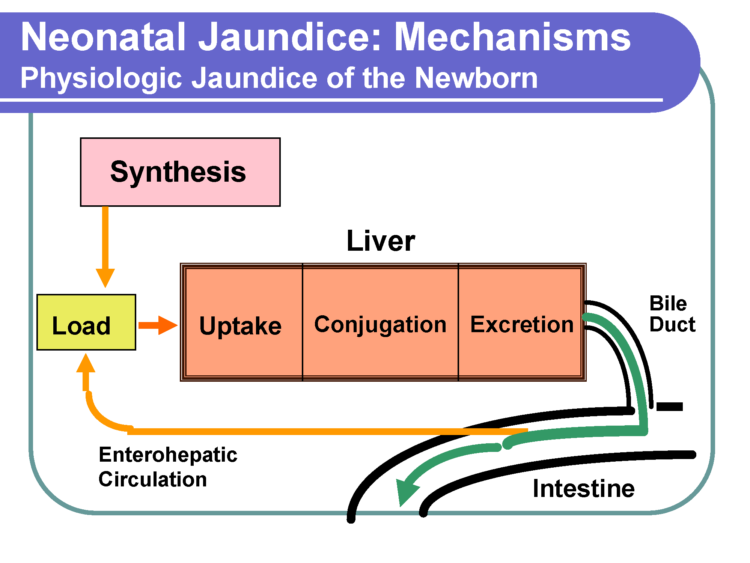
In addition, leading up to the point where there is brain injury and compromise to the infant’s life are days of constant crying and nursing in response to severe hunger and thirst caused by the fasting conditions imposed by the WHO BFHI, a phenomenon called “Second Night Syndrome.” Withholding supplemental milk from exclusively breastfed newborns who are nursing for hours and crying for additional milk is a common practice under the WHO’s Baby-Friendly protocol and it carries the risk of serious starvation-related complications, including jaundice, dehydration and hypoglycemia—established causes of brain injury. These complications are the medically-indicated reasons for supplementation, which require hospitalization to limit and prevent further brain injury, and they are nearly all preventable with ethically responsible monitoring, patient education and earlier supplementation. In addition to the risks of not supplementing, being fully fed is a basic human right that is not currently met by the standard of care.
In a recent editorial, our critics have accused the Foundation of being unwilling to engage with parties with opposing viewpoints, but that is simply untrue. Senior members of the Fed is Best Foundation along with a guest neonatologist from a BFHI-certified hospital, and guest pediatric endocrinologist, the lead author of the Pediatric Endocrine Society neonatal hypoglycemia guidelines, Dr. Paul Thornton, met with the top officials of the World Health Organization breastfeeding guidelines on September 22, 2017, Dr. Nigel Rollins, Dr. Laurence Grummer-Strawn and Dr. Wilson Were via teleconference. A full account of the meeting can be found here. We presented data on the high rates of complications in exclusively breastfed newborns from research conducted at BFHI hospitals and the expected prevalence of brain injury and long-term disability resulting from those complications.
The neonatologist in attendance reported on the experiences of neonatologists with the BFHI stating, “we are seeing these cases almost every day every where around the country. The focus [of the BFHI] is only on the number of women who are exclusively breastfeeding at discharge and not at all on safety.” During this meeting we uncovered that the WHO has never studied the complications associated with the WHO Ten Steps and has no program to monitor complications caused by the BFHI. As we have suspected, no attention has been paid to patient safety, which is the reason why our Foundation exists. Since there has never been any study of the safety of the BFHI or its medical indications for supplementation, there is no assurance that they protect babies from injury; in fact the evidence presented at the meeting on these complications reveal that they do not. Dr. Rollins informed us that every health professional trained in the Baby-Friendly protocol has been taught to look out for danger signs of an underfed breastfed baby at risk of brain injury which include, “convulsions, lethargy and inability to feed.” Unfortunately, the evidence presented showed that these are signs that brain injury is already present.
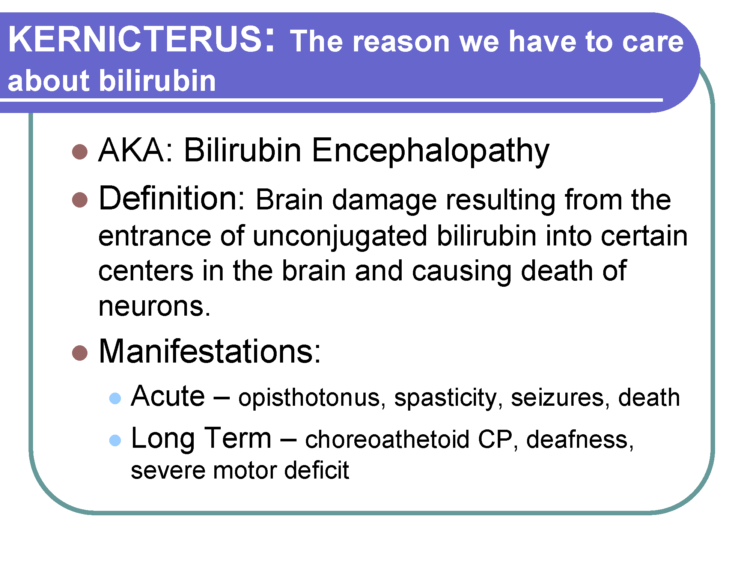
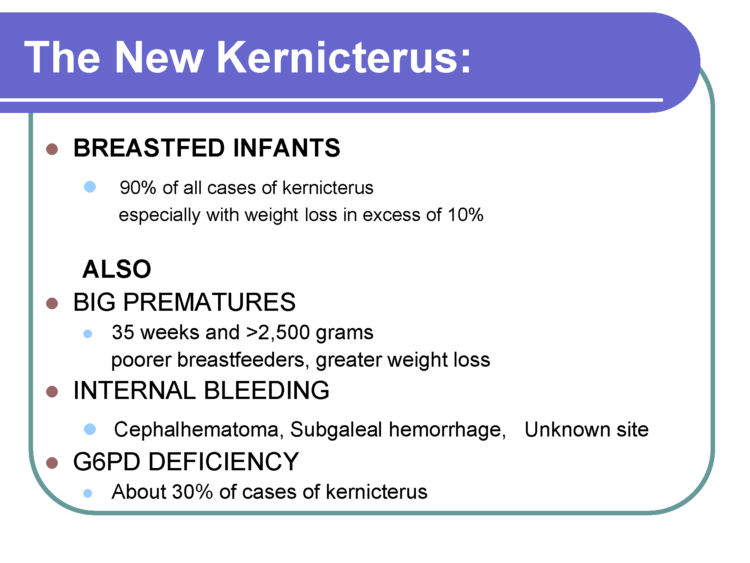
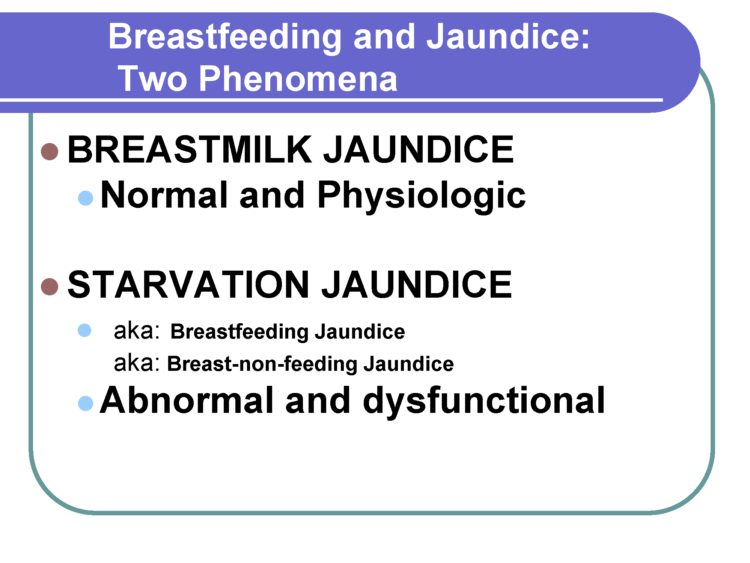
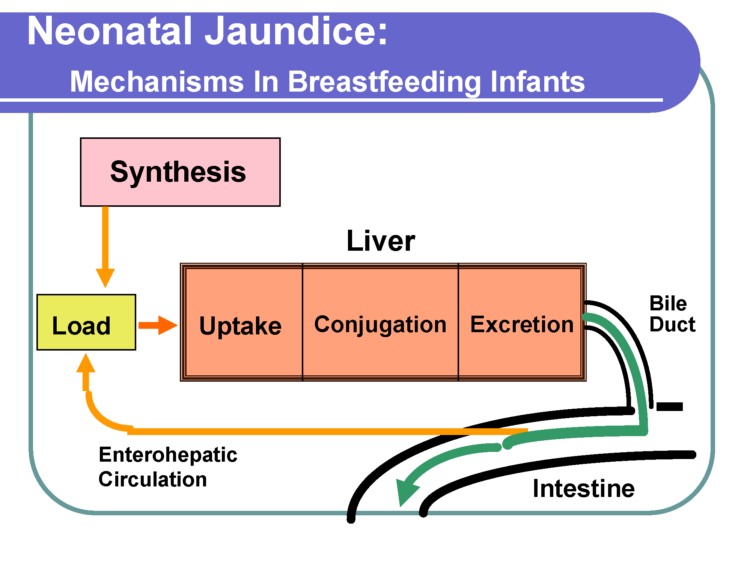
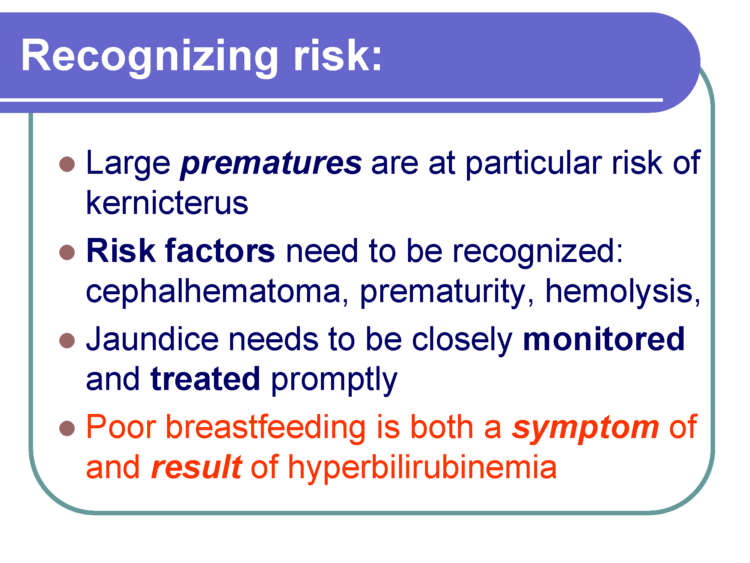
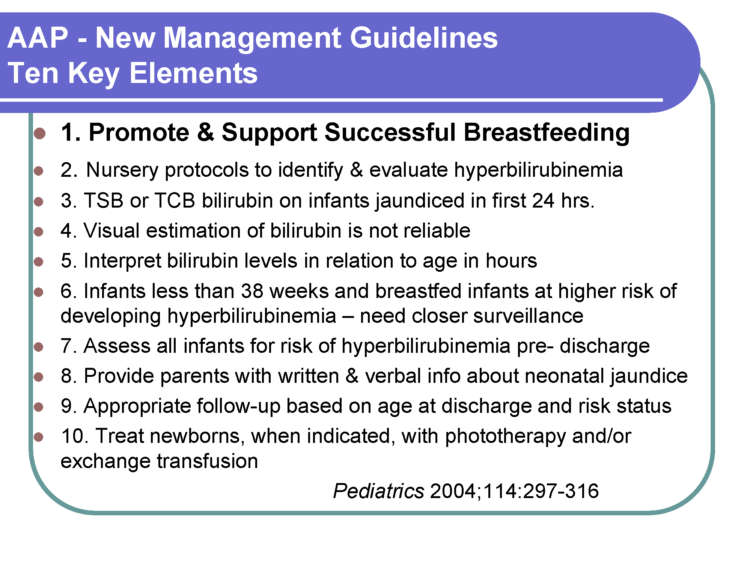
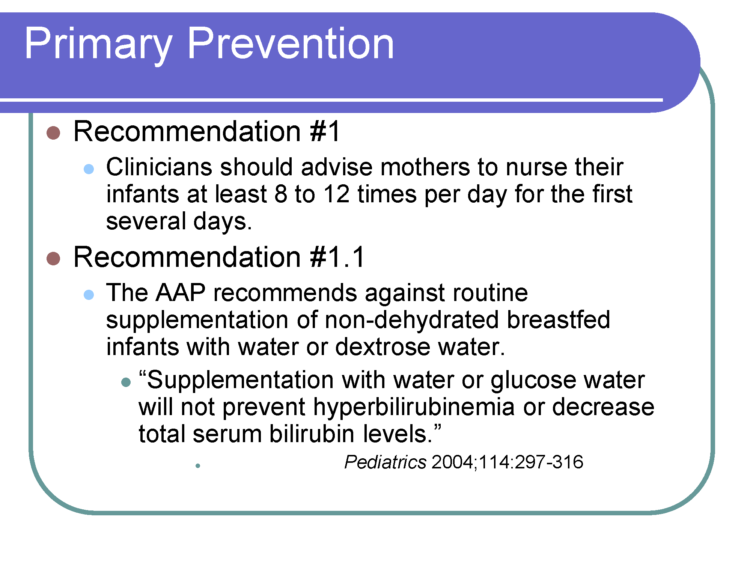
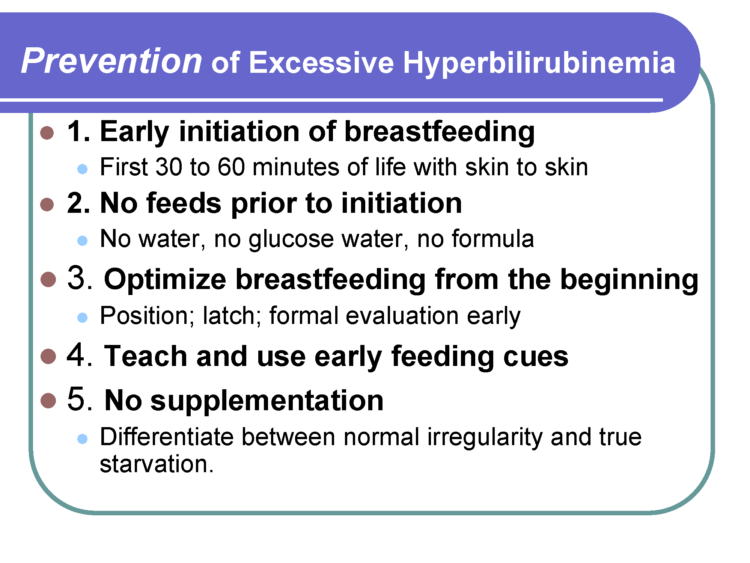
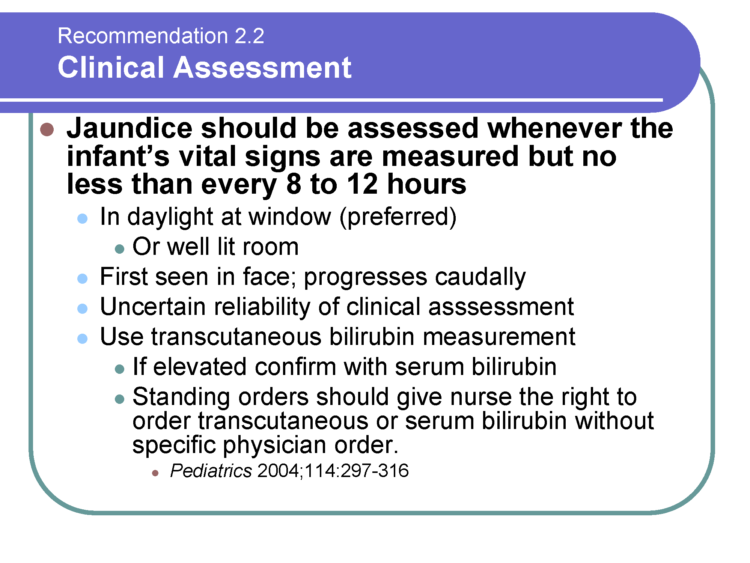
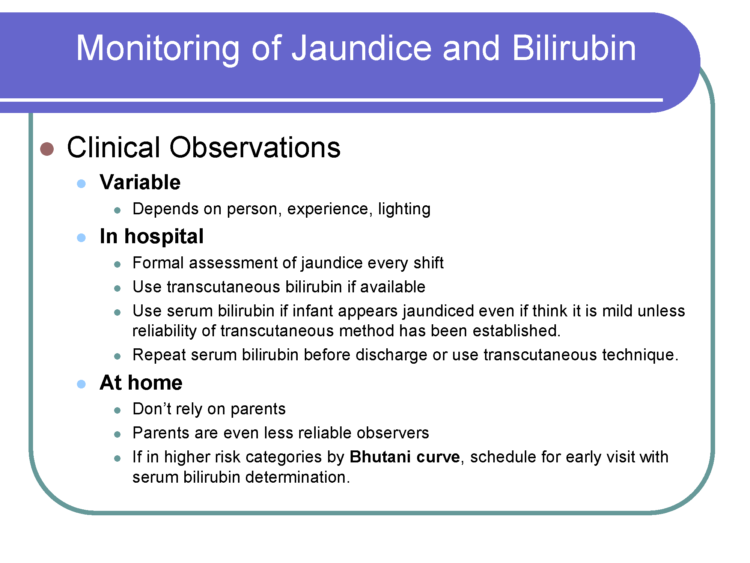
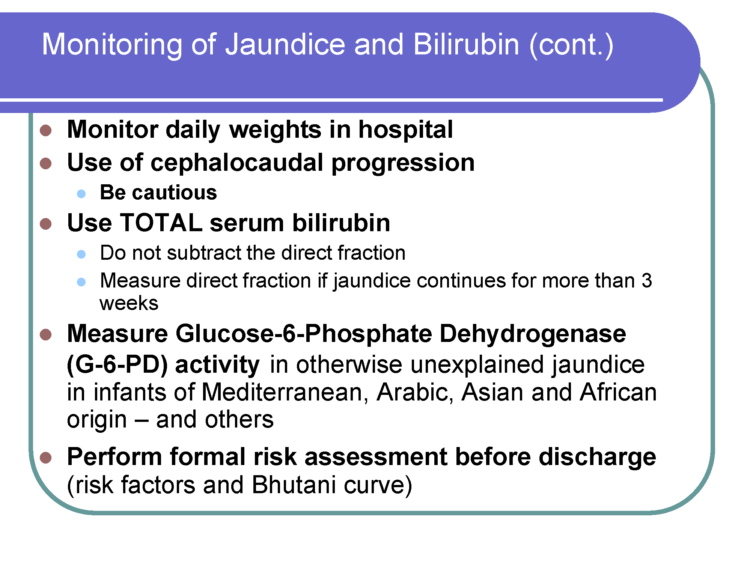
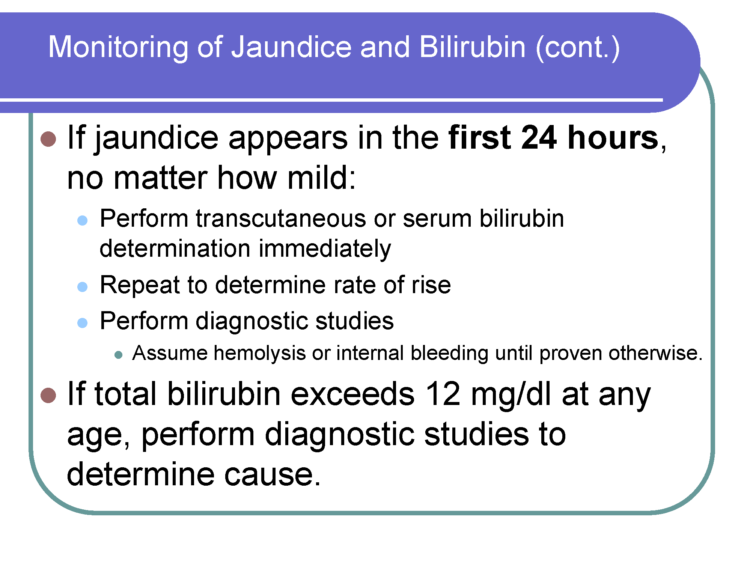
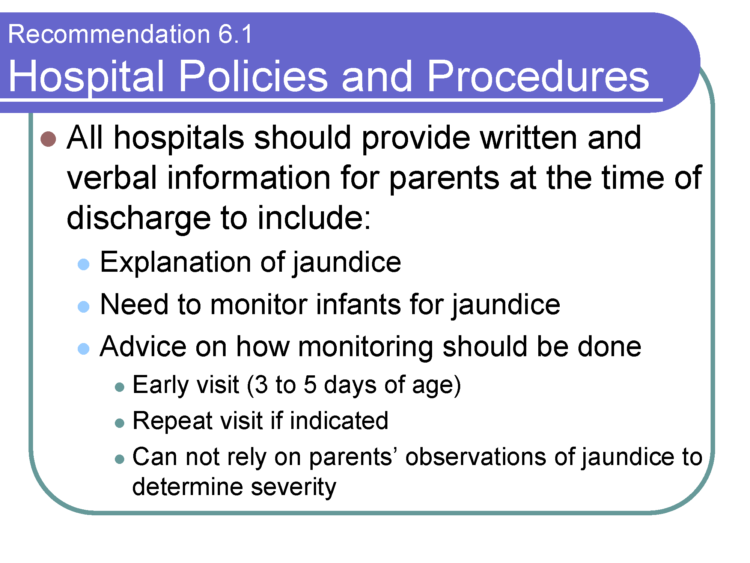
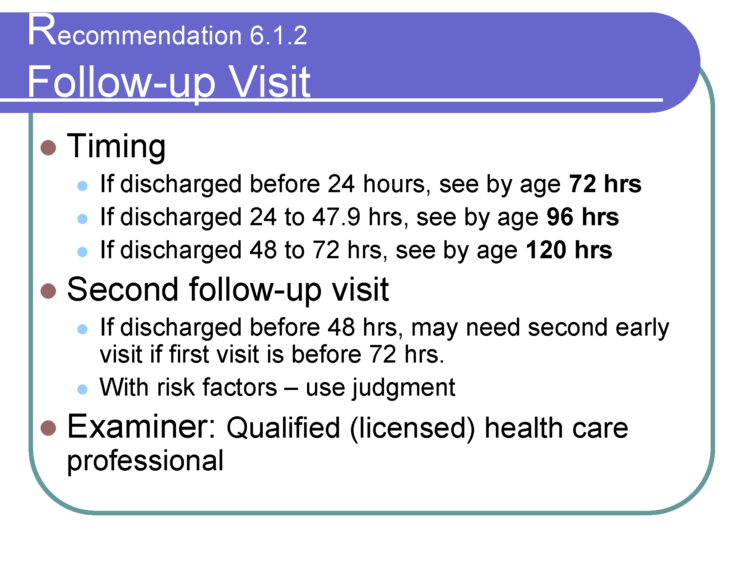
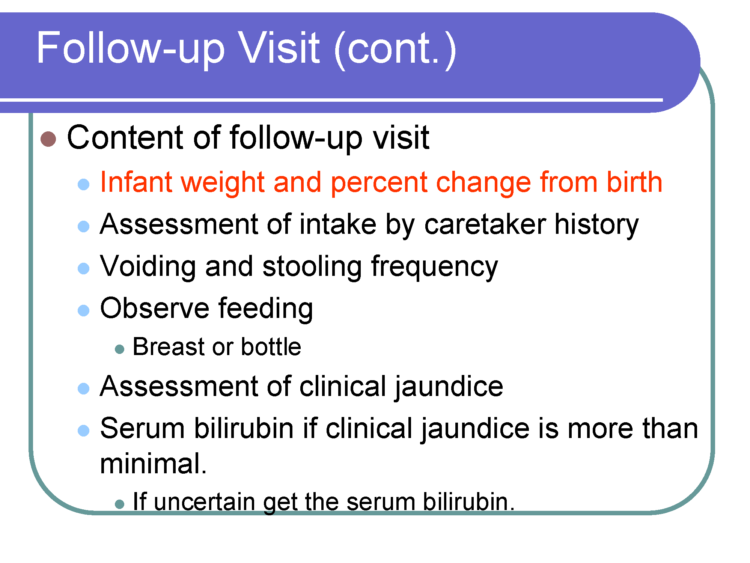
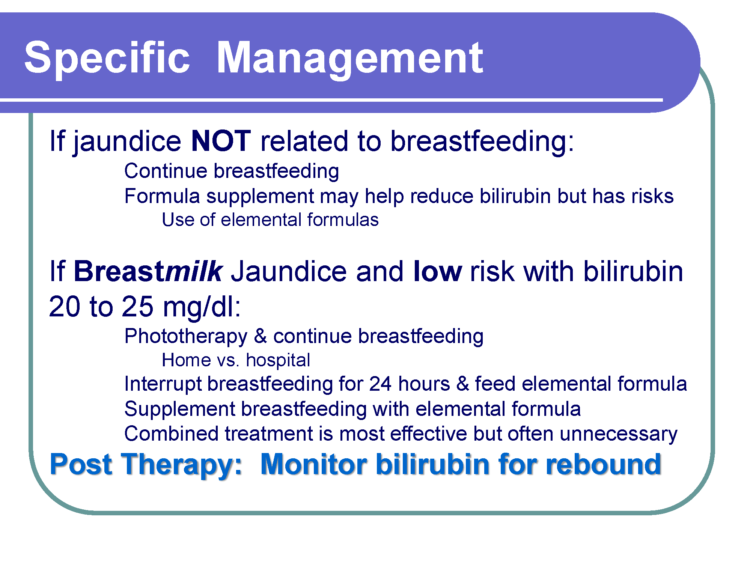
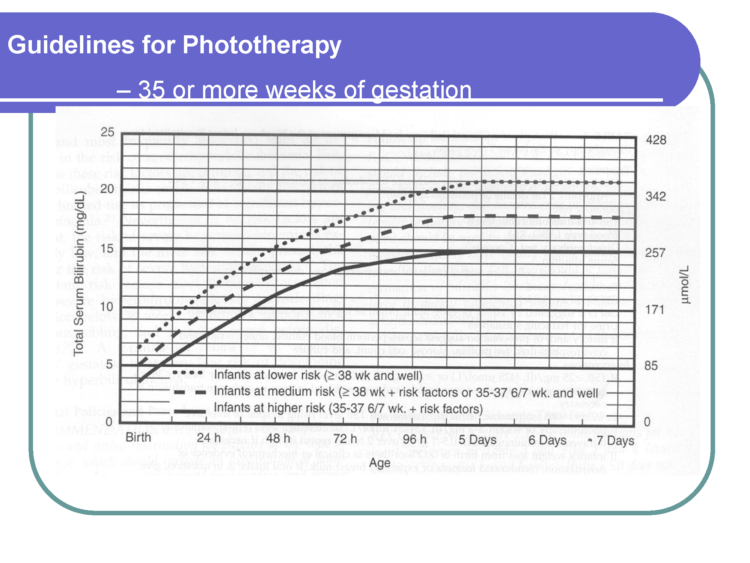
We have uncovered a lecture provided to lactation consultants at a prominent breastfeeding conference given by Baby-Friendly USA Chief Medical Consultant, Dr. Lawrence Gartner, who discussed the risk of brain injury from starvation-related jaundice, called kernicterus, 90% of which occurs to breastfed babies who lose excessive weight, according to his lecture. Yet despite this training, no information on the risk of preventable brain injury from starvation-related jaundice in breastfed newborns exists in patient-directed breastfeeding literature published by breastfeeding advocacy groups other than our own.
The full lecture by Dr. Gartner can be found here:
The directive given to breastfeeding mothers to “give no food or water other than breast milk” in combination with no education on the signs of infant starvation is leading to an epidemic of infant feeding complications, hospitalizations and injuries that is well-documented, a status quo that took the life of Landon Johnson five years ago. These complications occur because of the failure to truthfully inform parents of the common problem of insufficient breast milk, especially in the first days of life, and the serious and irreversible consequences of not delivering sufficient calories and fluid to an infant. Sadly, despite being provided evidence on the high rates of complications from Baby-Friendly practices, we were disappointed that the WHO had not identified informing the public of the dangers of infant starvation and the importance of supplementation to protect an infant’s brain and life as “a top priority.”
We are currently meeting with top officials of prominent health organizations and health insurers to advance the mission of the Fed is Best Foundation to protect families from unsafe practices found in breastfeeding management and to protect infants from injury caused by misinformation currently perpetuated in WHO-based breastfeeding education. We are changing the standards of breastfeeding management to protect the child’s health and brain first before protecting exclusive breastfeeding rates. Unfortunately, this leaves meeting with organizations whose standards of breastfeeding management and education have caused an epidemic of feeding complications in breastfed newborns, a lower priority.
Sadly, because of our opposition to BFHI policies, we face significant opposition from organizations who think that exclusive breastfeeding should be promoted at all costs. That opposition ranges from attacks on social media to accusations that the Foundation is funded by formula companies, which is simply not true. We do not and have never accepted donations from infant feeding companies, both breast- and formula-feeding. We are funded entirely by the private donations of mothers whose children have been hospitalized and disabled by the WHO Ten Steps and the BFHI. They support the Foundation with their personal funds and volunteer to protect future babies from experiencing the same harm.
We have made tremendous progress as mothers globally are now aware that supplementation protects the brains and lives of babies who are underfed by exclusive breastfeeding. We have guided mothers in supplementing their babies in the first days of life to prevent excessive weight loss and hospitalization who have gone on to safely and exclusively breastfeed, in both the developed and developing world. We have also supported mothers to combination feed and exclusively formula feed, protecting their children from hunger while believing in and respecting her ability to produce milk, her intelligence and her choice. We have stood against violating the human rights of newborns by ensuring their access to sufficient calories and fluid to protect their brain and vital organs and to protect them from the torture of hunger and thirst. We have taught mothers the signs and the consequences of infant starvation that have been conspicuously left out of breastfeeding education resources published to date.
Unfortunately, our critics have failed to honestly inform mothers of the dangers of these protocols. Our Foundation’s top priority is patient safety and the human rights of infants. We have limited resources, are volunteer-run, and simply have not had the time or interest to engage with organizations who have refused to publicly acknowledge the harm caused by current breastfeeding policies while blaming mothers when their babies are harmed by complications. If those organization members are willing, we invite them to an open, video-recorded forum with Foundation members and mothers whose children have been harmed by the BFHI protocol so that they may answer for them why they were not honestly informed of these complications and why their children were allowed to be hospitalized when they were assured they would get enough. Until they are willing to openly inform mothers of these dangers and provide them with evidence-based education on when to supplement to protect their infant’s life and brain before emergencies occur, we will continue on our mission and educate the public without them.
Addendum/Response from Dr. Lawrence Gartner, BF USA Chief Medical Advisor and Board Member:
”To: Fed Is Best (FIB)
From: Lawrence M. Gartner, M.D.
Re: Lecture Slides
It has been brought to my attention that selected slides and a complete set of slides from one of my lectures has been posted on your website without my permission or prior knowledge. The accompanying comment by the website editors implies that starvation jaundice is responsible for 90% of all cases of kernicterus. Those at the lecture that accompanied these slides heard me make the point that inadequate caloric intake during the newborn period contributes to the risk of developing kernicterus, but is rarely the sole cause of excessive hyperbilirubinemia and kernicterus.
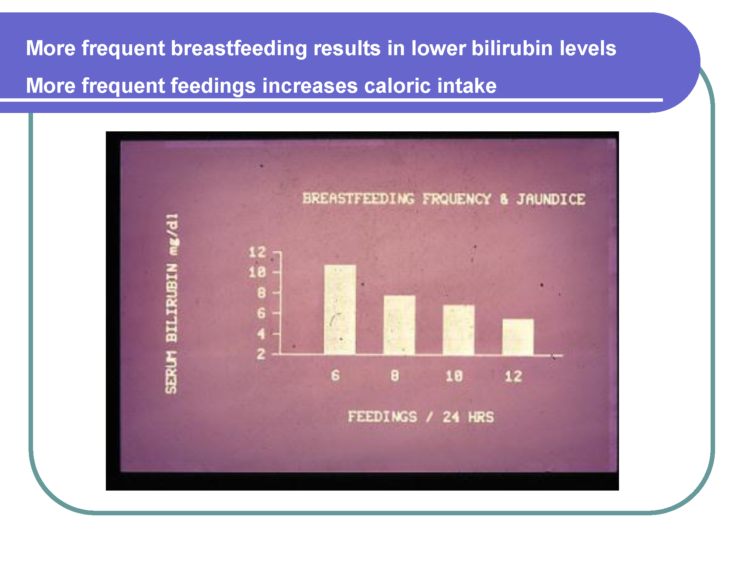
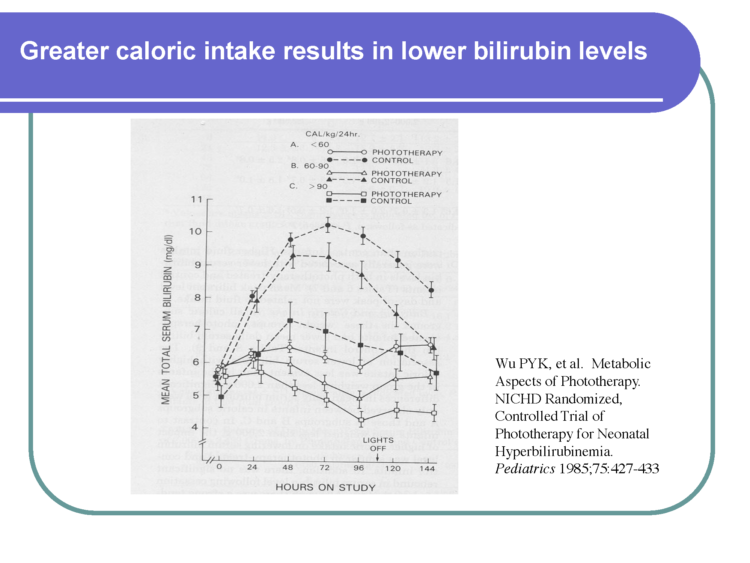
The slides list the major causes of excessive hyperbilirubinemia, which themselves cause poor feeding and further increase in serum bilirubin. The point I was making in this lecture was that physicians and nurses need to recognize and correct inadequate intake of calories in sick infants and those with excessively rising serum bilirubin levels that are approaching potentially toxic levels, whether formula feeding or breastfeeding. The lecture also provided the clear evidence from multiple studies that infants breastfed under the guidance provided by the WHO Baby Friendly Hospital Initiative do not have excessive jaundice and are not at risk of kernicterus unless they have a pathologic condition which either increases serum bilirubin levels or renders the infant unable to feed adequately. The final slides in this lecture provide guidance for both optimal breasting management according to Baby Friendly standards and for detection of pathologic conditions which may cause excessive jaundice. Supplementary feeding of sick breast or formula fed infants is always indicated if the child is clearly starving. But, supplementary feeding of formula for healthy breastfed infants is never indicated or needed because it will increase the likelihood that breastfeeding will subsequently be insufficient, which then may increase jaundice.
Although my first thought for this letter was to request that you remove my lecture slides from your website, I am now inclined to give permission for the complete lecture slide set to remain on the site so those who want to learn from it may do so. However, you may not place selected slides on the website. I also require that comments on my slides accurately reflect what I have stated in the lecture, as I have indicated above.”
Lawrence M. Gartner, M.D.
Professor Emeritus, Pediatrics and OB/GYN
The University of Chicago
Member, Board of Directors, Baby Friendly USA
Response from Christie del Castillo-Hegyi, M.D., Co-Founder of the Fed is Best foundation
Dear Dr. Gartner,
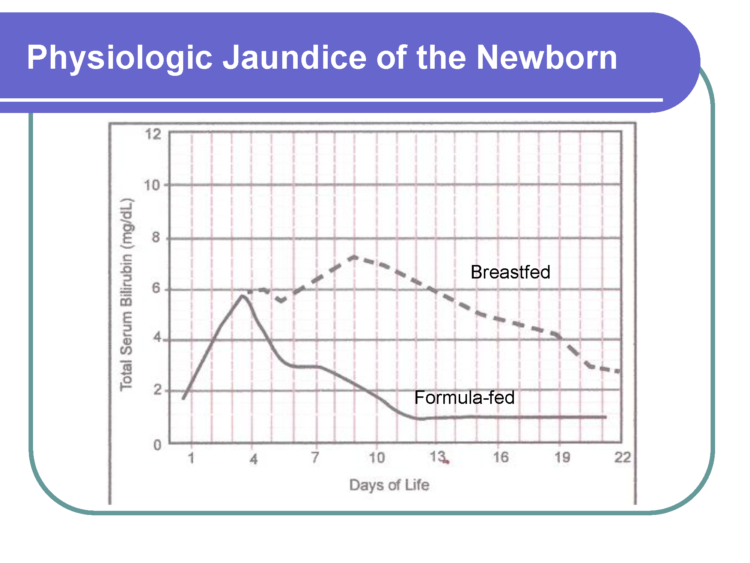
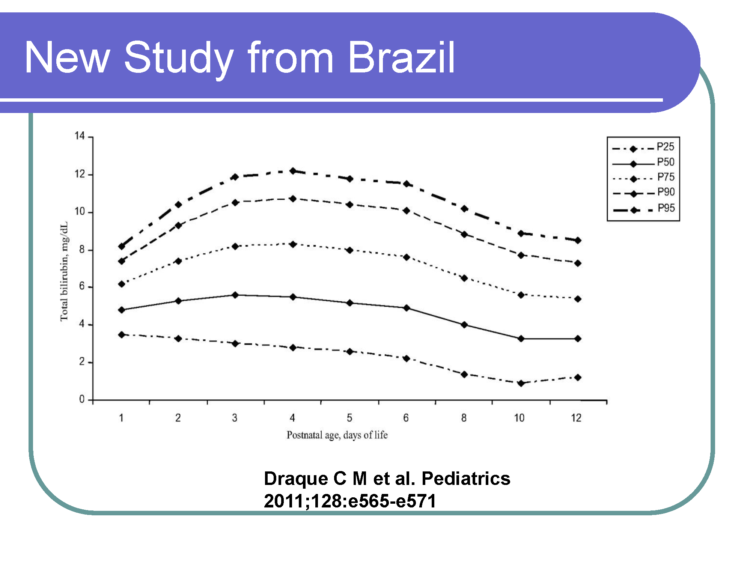
We are happy to include the comments in this letter as an addition to the blog but we disagree that the BFHI protocol protects babies from these outcomes as the literature shows that it does not. There is no evidence that healthy term breastfed babies are protected from these outcomes as recent BFHI data shows that 10-25% of healthy term babies lose > 10% and that 10-20% of them develop phototherapy-requiring levels of jaundice with more than 10% requiring phototherapy. Furthermore, any neonatologist can attest that the vast majority of babies admitted to the NICU for severe jaundice commonly accompanied by dehydration and hypoglycemia are exclusively breastfed newborns whose mothers have been told not to worry about insufficient breast milk despite their child showing obvious signs of distress and hunger, per the BFHI protocol.
The BFHI protocol, according to data on the actual caloric content of colostrum (54 Cal/dl), the published basal metabolic rate of newborns required to prevent starvation conditions (100-120 Cal/kg/day) and the average published volumes of a mother’s colostrum shows that the average mother provides a 3 kg newborn 10% then 33% then 66% of their caloric requirement the first 3 days of life. Therefore, the BFHI requires newborns to fast for 3 days, which makes it the primary cause of starvation and the primary cause of pathological jaundice in healthy newborns, even when a mother produces the expected amount of colostrum. Some babies are lucky to have mothers who produce copious milk earlier to rescue them from starvation; an unacceptable number do not. This caloric yield not only makes the BFHI protocol unsafe, it also makes it unethical, barbaric and illegal by global human rights standards. This is the reason why the majority of EBF newborns experience distress from severe hunger and thirst called, “The Second Night Syndrome.”
We appreciate your efforts to educate lactation consultants on the matter of insufficient breast milk and brain injury from jaundice but this material should be available to all parents because any cause of serious life- and brain-threatening conditions to a newborn related to infant feeding should be made available to every parent. I can provide a slideshow of the entire lecture on the website formatted so that any health professional or parent can easily look through the entire lecture.
Sincerely,
Christie del Castillo-Hegyi, M.D.
Follow-up Email from Dr. del castillo-Hegyi
Dear Dr. Gartner,
I have updated the blog post to offer a view of your presentation in slideshow format with full navigation. I have also included the comments you sent in your email in its entirety along with my response. I am happy to edit or remove it if you change your mind about adding it to the blog. The link to the blog is here: http://fedisbest.org/2017/11/fed-best-foundations-top-priority-saving-babies-lives/
While your presentation suggests that frequent feeding may reduce bilirubin on average, according to the studies, these statistics do not reflect a guarantee of that relationship for every mother and child in real life. Recommending “frequent feeding” and improvement of latch as solutions to insufficient breast milk intake only works if a mother has the volume of breast milk/colostrum to meet a child’s metabolic requirement and for an unacceptably high number of mothers, “frequent feeding” and latch correction will not be enough to prevent brain-threatening levels of hyperbilirubinemia, hypernatremic dehydration or hypoglycemia, all of which can occur by 7% weight loss. Frequent feeding is the most common sign of a starving newborn that ends up being lethargic, brain injured and encephalopathic from these complications.
Furthermore, the AAP recommends against supplementing with water and sugar water as these supplements do not contain fat or protein required to promote bilirubin excretion. But formula and donor milk supplementation DO reduce bilirubin as the literature adequately shows over and over again. The volume of milk a child receives is the main determinant of bilirubin excretion. So I do not agree that supplementation worsens starvation jaundice. That is absolutely incorrect. Supplementation with breast milk substitutes when mom’s own breast milk is not enough is in fact an important part of the treatment regimen of a hyperbilirubinemic newborn as enteric excretion is the primary mode of bilirubin elimination. Formula supplementation has also been shown to increase exclusive breastfeeding rates at 3 months in newborns who lose 5% between 24 and 48 hours. The Kaiser BFHI data shows that formula-fed and freely-supplemented newborns never lose greater than 10% and therefore by definition never experience starvation jaundice.
Ultimately, a high number of mothers will not have the milk to prevent newborn complications from happening and it is time that BFUSA recognize that breastfeeding tragedies that occur to babies experiencing the BFHI protocol have nothing to do with insufficient support or education. It results from insufficient milk which is determined by the biological properties of colostrum and the biological realities of breastfeeding mothers. The BFHI appears to have never done the math required to know whether or not the protocol is safe. The fault does not lie in the individual health providers or the mother. It lies in the unsupported belief that colostrum is enough to meet the minimum metabolic requirement for the vast majority of exclusively breastfed newborns, which the science shows it does not. EBF are known have higher circulating levels of ketones than EFF babies because they are in fact fasting. They are also at risk of hyperosmolar hypernatremic dehydration, from fluid deprivation, also caused by exclusive colostrum feeding. All the data points to the fact that colostrum (54 Cal/dL), which has fewer calories the mature milk (66-77 Cal/dL), does not actually provide a child their full metabolic requirement and therefore prolonged newborn crying and frequent feeding are signs of hunger and thirst, which at this time, are not medically-indicated reasons for supplementation. The BFHI requires a child to actually have metabolic markers consistent with starvation beyond the level that is known to cause brain injury. Allowing exclusively breastfed newborns who are crying from hunger and fasting to not be supplemented makes it necessarily unsafe and a human rights violations. If colostrum actually met the metabolic requirement of a newborn, they would in fact not cry, not experience jaundice, hypernatremia or hypoglycemia. And we all know these absolutely happen to EBF newborns routinely. Millions of babies have suffered brain- and life-threatening complications as a result of the BFHI, which we described in our meeting with the Directors of the WHO Breastfeeding Guidelines program contained here. We hope you will review the account of the meeting as well as the video presentation contained within that I prepared for the WHO.
Christie del Castillo-Hegyi, M.D.
The Fed is Best Foundation
christie@fedisbest.org
Mothers, interested family members and health professionals wishing to attend this video-recorded forum hosted by the Fed is Best Foundation to discuss starvation-related complications of the Baby-Friendly Hospital Initiative with lactation professionals and Foundation members, please email contact@fedisbest.org. Please send an email with your name and your affiliation. Once we have an estimate on the number of interested parties, we will make arrangements and send information on the date and time of the forum.






As a mother whose son suffered and was hospitalized by BFHI protocol, I truly can’t understand why this is such a hard concept for healthcare providers in these hospitals. I think of all the WHO’S Ten Steps, the most dancing is actually the one where they ask hospitals to only track exclusive breastfeeding rates. If that is truly the only number you care about, of course babies will be harmed in the process. It creates a culture of lying and bullying in those facilities at a time when mothers need clear, compassionate support to care for their new babies. If readmissions or NICU transfers counted more than the almighty EBF rate, this support would happen naturally. As it stands, you have the horror that passes for “care” today.
This is important information. Thank you. The trick is to give all mothers accurate and informed follow-up care, and to be sure that babies are transferring milk from the breast before they are discharged. Breastfeeding is not to blame for providers who lack the understanding and who see babies with 15% weight loss or not pooping enough every day, both early signs of big trouble. If these signs are picked up early enough (within 2 or 3 days after discharge from the hospital, and managed appropriately, babies will do well.
Unfortunately, babies can already have brain injury from hypogylycemia, jaundice and hypernatremia even before they leave the hospital or before they get seen even the day after discharge. All of those conditions can develop by 7% weight loss and an EBF newborn can develop that weight loss by 24 hours of life. Wet and dirty diapers do not accurately predict sufficient intake. Crying, however, is a sign that is often dismissed as a sign of newborn hunger and starvation.
And here is the give away: The lecture also provided the clear evidence from multiple studies that infants breastfed under the guidance provided by the WHO Baby Friendly Hospital Initiative do not have excessive jaundice and are not at risk of kernicterus unless they have a pathologic condition which either increases serum bilirubin levels or RENDERS THE INFANT UNABLE TO FEED ADEQUATELY.
First, what if it is the mother with the pathological condition that prevents her from producing enough colostrum/milk for the infant to feed adequately?
Second, how are the providers supposed to tell if the infant has such a pathological condition, other than the infant showing signs of hunger and distress?
I was told my son had a great latch, he nursed A LOT, we were going great according to the staff. Except by the 2nd day he was fussing 20 minutes after nursing and I felt nothing in my breasts. He was also destroying my nipples. I started supplementing before we left the hospital because something wasn’t right. Turns out he had a severe tongue tie and was not transferring milk efficiently from the breast. No one on the staff thought to check his tongue. If I hadn’t made the decision to supplement and accepted a constantly crying baby as normal, who knows what would have happened.
Dr. Gartner is simply playing semantics. An EBF infant who is being fed adequately does not display the behaviors Fed is Best says require supplementation. What does Dr. Gartner consider adequate feeding for an infant, and how can he tell?