By Christie del Castillo-Hegyi, M.D.
This week, the journal Academic Pediatrics, published a study conducted by the Newborn Weight Loss research group led by Drs. Valerie Flaherman and Ian Paul, which consisted of 143,889 healthy, term and near-term newborns born at the Baby-Friendly Northern California Kaiser Permanente hospital system from 2009-2013.[1] They included newborns who were discharged from their birth hospitalization without requirement of intensive care, which includes newborns who developed jaundice before discharge. They looked at the effects of mode of feeding, namely exclusive breastfeeding and exclusive formula feeding during the birth hospitalization on the rates of rehospitalization and number of outpatient follow-up visits. In addition, they looked at the effects of percent weight loss on the same outcomes.
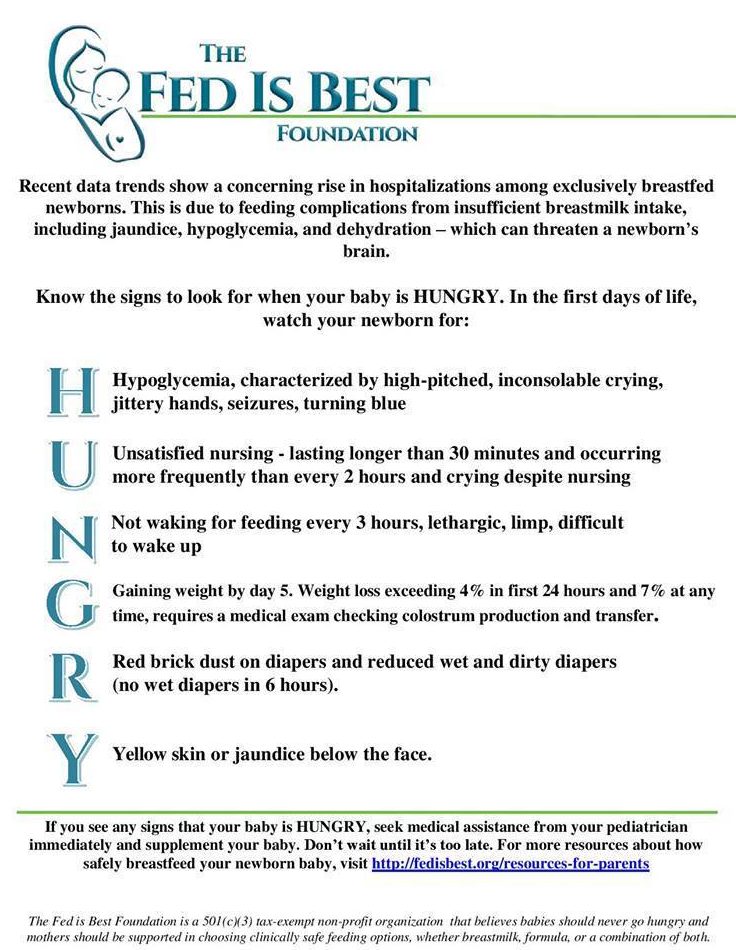
Overall, 6.2% (1 in 16) of the healthy term newborns studied were readmitted; 4% were vaginally delivered and 2.2% were Cesarean delivered. This represents 8921 newborns over the five year period, almost 5 babies per day. They showed that exclusively breastfed newborns had slightly more than double the risk of being rehospitalized, even when adjusted for gestational age, birth weight and maternal race/ethnicity. Exclusively breastfed newborns also had significantly more (32% more) outpatient visits in the first 30 days after birth compared to exclusively formula-fed newborns. The leading cause of readmission was for hyperbilirubinemia or jaundice and need for inpatient phototherapy. The purpose of phototherapy is to reduce blood bilirubin levels in order to prevent or limit brain injury, a complication of insufficient feeding and dehydration commonly found in exclusively breastfed newborns before the onset of copious milk production (lactogenesis II).

Astonishingly, 0.4% of vaginally-delivered and 6% of Cesarean-delivered newborns were discharged at > 10% weight loss (about 9209 newborns). The average number of outpatient visits were significantly greater for those with > 10% weight loss at discharge than they were for those with < 8% weight loss at discharge. For Cesarean-delivered newborns with > 10% weight loss at discharge, rehospitalization rates were significantly higher than for newborns with < 8% weight loss.
Of those who were weighed at 48-72 hours, 9.3% of vaginally-delivered and 14% of cesarean-delivered newborns developed > 10% weight loss. Almost 10% of vaginally-delivered newborns with > 10% weight loss were readmitted to the hospital compared to 4.7% of those with < 8% weight loss, a 2.2-fold increased risk. Cesarean-delivered newborns who lost > 10% in this time-frame were also at increased risk of rehospitalization and had more outpatient visits.
Overall, this study done on a very large cohort of healthy term and near-term newborns showed what has been widely observed by clinicians, including the American Academy of Pediatrics hyperbilirubinemia guidelines committee,[2] and what has been demonstrated repeatedly in the peer-reviewed literature, [3, 4] that exclusively breastfed newborns are at greater risk for phototherapy-requiring jaundice. This same research group, in a previous study, showed that exclusively formula-fed newborns rarely lost > 7-8% of their birth weight while 10% of vaginally-delivered and 25% of cesarean delivered exclusively breastfed newborns lost > 10%.[5, 6] Therefore, exclusively breastfed newborns are at higher risk of developing hyperbilirubinemia from excessive weight loss and insufficient feeding compared to exclusively formula-fed newborns. Consequently, exclusively breastfed newborns are also at increased risk for long-term consequences of bilirubin-induced brain injury, also known as Bilirubin-Induced Neurological Disorder (BIND).[7] The developmental disabilities related to high bilirubin can occur at bilirubin levels routinely found in infants requiring phototherapy (bilirubin level 13.7 – 26 mg/dL or 233-355 mmol/L in one study,[8] increasing in severity at levels above 19 mg/dL).[9] The developmental abnormalities of BIND can include deficits in attention, language, cognition, behavior as well as visual, auditory, motor and sensory development and can also increase the risk of seizure disorder.[7] In addition to the brain-insults caused by hyperbilirubinemia in underfed breastfed newborns are the co-occurring insults of hypotensive dehydration (low blood pressure causing reduced circulation to the brain), hypernatremia (high sodium from fluid deprivation) and hypoglycemia (low blood sugar), all of which individually are known causes of brain injury.[10, 11] Each of these complications add to the burden of brain injury that can have devastating effects on the newborn brain. A case series published in Hospital Pediatrics in 2015 showed the devastating levels of brain injury present in poorly fed breastfed newborns from hypoglycemia, showing brain injury present on MRI by day 3-5 of life affecting a third to almost the entire brain leading to varying lifelong disabilities.[12]
The findings of the Flaherman study provide robust evidence that keeping newborns from losing greater than 8% afforded the greatest protection from hospitalization for feeding complications and hyperbilirubinemia. The Fed is Best Foundation in fact recommends no greater than 7% weight loss, which is also the AAP’s current maximum weight loss recommendation, as published in the 2013 AAP breastfeeding guidelines.[13,14] The rationale for this recommended maximum weight loss is evidence that a child can develop hypernatremic dehydration by 7% weight loss, a known cause of brain injury and death.[15] Given the limited availability of breast milk/colostrum commonly found in the first days of life even with maximum breastfeeding management (more than 1 in 5 women will have delayed lactogenesis II),[16] immediate supplementation of breastfeeding is indicated to meet the full metabolic requirement of roughly 6 oz/kg/day with safe,[17] tested donor breast milk or formula when a newborn is approaching 7% or developing excessive jaundice before bilirubin levels rise above developmentally deleterious levels and before they need phototherapy. There is evidence that by the time a child meets criteria for phototherapy, they are at increased risk of already having markers of brain injury present in the blood.[18] In addition, providing parents informed consent of the increased risks of jaundice, dehydration, hypoglycemia, brain injury and hospitalization associated with exclusive breastfeeding before lactogenesis II, while validating the option of properly managed supplemented breastfeeding until full milk production with donor milk or formula, could potentially eliminate all jaundice hospitalizations and injuries caused by excessive weight loss.
This study underlines that exclusive breastfeeding of newborns before full milk production is associated with clear risks that few to no parents are informed of. The study showed a staggering number of babies hospitalized for not getting fed enough milk. At a time where safe alternatives to breast milk is readily available to every single infant born in a hospital, threatening even one child’s future with jaundice, hypoglycemia or dehydration is unacceptable. Furthermore, many of these newborns are crying inconsolably, constantly nursing or developing signs of lethargy as indications of hunger and thirst leading up to the development of these complications. Unfortunately, the study authors included the following comment in their discussion:
“Such short-term adverse consequences of exclusive breastfeeding may be viewed as representing an acceptable tradeoff given the magnitude of the reported benefits.”
Whether this statement reflected their own perspective or a perspective adopted by other health professionals in general, from a parent’s perspective, no child is expendable. Even more so, no child is expendable for the sake of increasing exclusive breastfeeding rates at discharge, a clinically meaningless health metric that has the unacceptable side effect of increasing complications and hospitalizations to previously healthy newborns. Furthermore, every patient has the right to information that reduces their risk of even short-term adverse consequences and hospitalization, more so if the risks involve permanent disability and death.
The documented risks of early exclusive breastfeeding and their consequences to newborn brain development call into question where the benefits of breastfeeding are truly derived. Are they from breast milk and breastfeeding themselves? Or are they derived from the systematic harm caused to newborns who develop feeding complications from failed and insufficient lactation, which necessarily categorizes them as “formula-fed” once they are finally rescued from brain injury and death by formula? In a system that only protects babies whose mothers’ breast milk supply can protect them from starvation-related complications, the burden of the long-term negative effects of starvation are carried by the newborns who go on to be “formula-fed.” Such a system of infant feeding can create the advantage of being breastfed simply by making it disadvantageous to be born to a mother who has no milk.
The authors calculated that they would have had 1706 fewer readmissions had the readmission rates for exclusively breastfed newborns been similar to those of exclusively formula-fed newborns. Given an estimated $4548 per admission, that would have saved $7.8 million dollars for that one hospital system alone, according to the study authors. However, this is an underestimate of the true cost of excess phototherapy admissions related to exclusive breastfeeding as a previous study from this same hospital system showed that 71% of their phototherapy admissions were in fact in newborns who developed hyperbilirubinemia during the birth hospitalization, a population that was excluded from the Flaherman study.[19] Furthermore, the American Hospital Association in a recent review of national neonatal readmissions data showed the average total cost per readmission to be $14,247, jaundice being the leading cause of readmissions. If we include the population that required extended hospitalization for phototherapy, this would have resulted in 4177 more excess hospitalizations for a total of 5883 excess hospitalizations from exclusive breastfeeding costing the hospital system almost $83 million. Given that almost 4 million infants are born each year, preventing hospitalizations for hyperbilirubinemia in insufficiently fed exclusively breastfed newborns by providing education on the signs of insufficient feeding and preventing excessive weight loss with supplementation would save the U.S. healthcare system approximately $415 million dollars a year in preventable phototherapy admissions alone, not including admissions for hypoglycemia and dehydration. In addition, the medical and rehabilitative services of newborns disabled by brain injury caused by these complications costs society millions more per child over their lifetime.
This study demonstrates a well-known phenomenon of aggressive exclusive breastfeeding promotion. The phenomenon of newborn starvation-related jaundice from exclusive breastfeeding is not new or rare. It is in fact the leading cause of newborn rehospitalization and a leading cause of perinatal disability globally.[20,21]
Since the publication of the Baby-Friendly Hosital Initiative in 1991 promoting exclusive breastfeeding from birth, neonatal jaundice rates has increased, the majority caused by starvation-related jaundice from insufficient feeding in exclusively breastfed newborns. In countries like Ghana where health care resources and monitoring for breastfeeding complications like jaundice and dehydration are limited, babies who develop severe jaundice commonly develop permanent brain injury and cerebral palsy.
It is not just a failure of breastfeeding technique, breast milk supply, breastfeeding education or a rare failure in biology. It is the failure of the authors of the exclusive breastfeeding guidelines to gather the necessary data to ensure safety in their recommendations. It is their failure to study the following vital information necessary to provide safe infant nutrition:
- the true milk requirement of newborns to protect their brain and vital organs, (100-120 Cal/kg/day or 2.7 oz/lb/day or 6 oz/kg/day of mature breast milk or formula from the first day of life)[22]
- the true caloric yield of exclusive colostrum feeding (colostrum provides 54 Cal/dL which provides an average of 10-66% of a 3 kg newborn’s daily caloric requirement for the first 3 days of life)[23, 24]
- the true milk production of women to safely exclusively breastfeed from birth to 6 months of life without causing fasting conditions and starvation-related complications that can have permanent negative consequences to infant brain development, which has never been studied
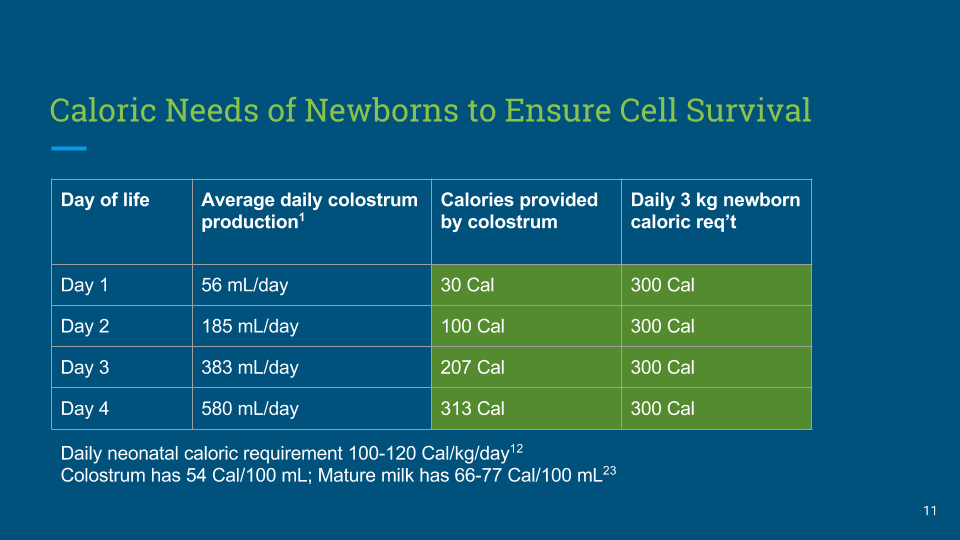
Figure 1. The Caloric Yield of Exclusive Colostrum Feeding
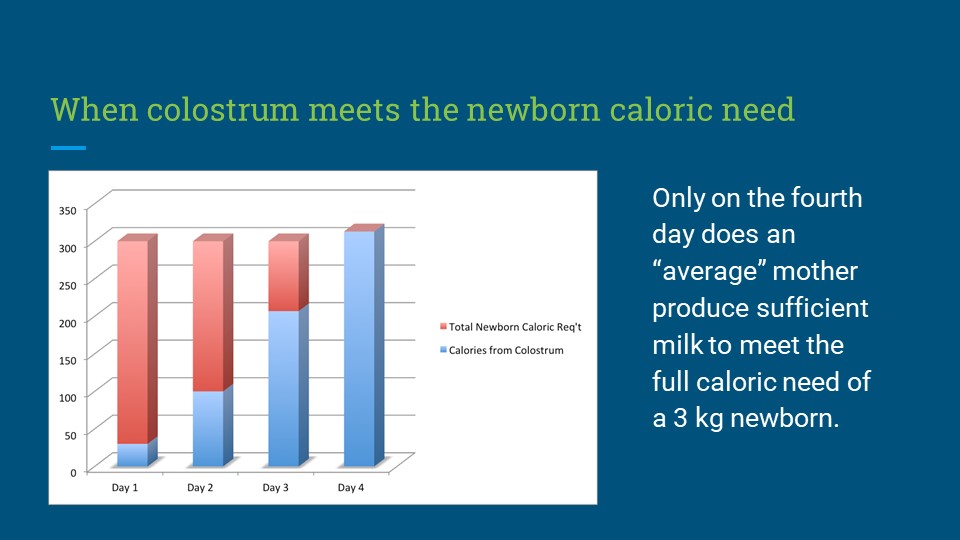
Figure 2. Graphical Representation of Caloric Yield of Exclusive Colostrum Feeding Relative to Newborn Caloric Requirement
Finally, the problem of infant starvation is a problem of refusing to question the authority that has created the rules of breastfeeding. Decades of scientific evidence has shown that the breastfeeding guidelines that are currently promoted by the WHO increase the risk of serious complications to newborns. Step 6 of the Ten Steps to Successful Breastfeeding, which is to “give no food or water other than breast milk,” has created an epidemic of neonatal feeding complications, hospitalizations, occult brain injuries and developmental disabilities in previously healthy newborns.
Last September, senior members of the Fed is Best Foundation met with top officials of the World Health Organization breastfeeding guidelines committee to discuss their concerns about the complications associated with the WHO Ten Steps to Successful Breastfeeding and the Baby-Friendly Hospital Initiative. There we discovered that the complications of the WHO Ten Steps and the BFHI have in fact never been rigorously studied or monitored by the WHO to ensure safety in the 29 years it has been promoted. In the meantime, the Ten Steps have hospitalized more babies for starvation-related complications than any public health policy that has ever been written and make up the leading causes of newborn rehospitalization worldwide.[21] Unfortunately, they gave no indication that they were going to inform parents of the serious risks of insufficient feeding from exclusive breastfeeding and the vital role of supplementation to prevent brain injury and long-term disability, an act that could save millions of babies from feeding complications, hospitalizations and injuries. Given the WHO’s unwillingness to address the harm caused by the Ten Steps and the BFHI, one must question whether the guidelines truly seek to provide the best outcomes for every newborn or whether the goals of the guidelines make it necessary to allow some babies to starve. Are exclusive breastfeeding rates at discharge more important than protecting the safety of every single child whose mother is recruited to exclusively breastfeed? Is it more important than telling parents truths about breastfeeding than can save their child from a lifetime of disability?
Putting children at risk of brain-injury and death by hiding the knowledge of those risks from patients constitutes criminal medical negligence. It is illegal to deny supplementation to a child who is showing all the clinical and laboratory markers of fasting and starvation known to be present in exclusively breastfed newborns, while blatantly exposing them to brain- and life-threatening complications that can permanently disable and even kill them. This practice of denying supplementation to exclusively breastfed newborns who are showing signs of hunger and dissatisfaction is in fact a violation of global human rights standards.[25] This is a standard of care of the BFHI that took the life of Landon Johnson almost 6 years ago.
The pressure to exclusively breastfeed when at least 15% of mothers are biologically incapable of doing so is resulting in crippling postpartum depression for mothers who struggle to breastfeed.[26,27] The psychological trauma inflicted on families who were misled to avoid supplementation resulting in accidental starvation and hospitalization of their newborns is profound. The suffering experienced by a child who survives these complications permanently disabled is immeasurable. The medical costs required to care for a previously-healthy injured child can impoverish a family.
It is time we recognize that exclusive breastfeeding for all mothers is an unrealistic goal regardless of who proclaims it as a public health priority as breasts do not in fact work that way. It is well-known that insufficient milk to safely exclusively breastfeed from birth to 6 months is common and the denial of this fact by the majority of breastfeeding education outlets and prominent breastfeeding advocacy organizations is having a devastating impact on our population. No research has ever been done to quantitatively prove that the vast majority of mothers have sufficient breast milk supply to safely follow the WHO’s recommendation of exclusive breastfeeding from birth to 6 months given known variations in breastmilk supply. Furthermore, teaching mothers to allow their babies to go hungry in order to achieve exclusive breastfeeding status can cause significant harm to a child’s developing brain if that child does not in fact receive sufficient calories for optimal brain development.
Breastfeeding can only be beneficial to a child if they are in fact being safely and fully fed from their first day of life onward, which is not guaranteed by current exclusive breastfeeding protocols. Any compromise of the delivery of calories and fluid to maintain the integrity of a child’s brain and vital organs can have irreversible consequences to a child’s health and future potential. Supplementing when a child is showing signs of persistent hunger due to insufficient breast milk is vital to the goal of protecting a child’s health and safety. Furthermore, providing mothers with options for supplementation including safe, tested donor milk and properly-prepared formula, respecting her right to full disclosure of the risks and benefits of every feeding option, and respecting her choice should be the standard of care. As it stands now, the standard of care makes healthy, term exclusively breastfed newborns the least safe patients in the hospital. This is an unacceptable evolution of infant feeding and it is up to every parent and health professional to change the standards so that every child is protected with safe and sufficient infant feeding.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and every thing in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
Thank you so much from the Founders of the Fed is Best Foundation!
References
[1] Valerie Flaherman, Eric W. Schaefer, Michael W. Kuzniewicz, Sherian Li, Eileen Walsh, Ian M. Paul, Health Care Utilization in the First Month after Birth and Its Relationship to Newborn Weight Loss and Method of Feeding, Academic Pediatrics (2017), https://doi.org/10.1016/j.acap.2017.11.005.
[2] American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 114, 297–316 (2004).
[3] Bertini G, Dani C, Tronchin M, Rubaltelli FF. Is breastfeeding really favoring
early neonatal jaundice? Pediatrics. 2001 Mar;107(3):E41.
[4] Seidman DS, Ergaz Z, Paz I, Laor A, Revel-Vilk S, Stevenson DK, Gale R.
Predicting the risk of jaundice in full-term healthy newborns: a prospective
population-based study. J Perinatol. 1999 Dec;19(8 Pt 1):564-7.
[5] Miller, J. R. et al. Early weight loss nomograms for formula fed newborns. Hosp Pediatr 5, 263–268 (2015).
[6] Flaherman, V. J. et al. Early Weight Loss Nomograms for Exclusively Breastfed Newborns. PEDIATRICS 135, e16–e23 (2015).
[7] Bhutani, V. K. & Johnson-Hamerman, L. The clinical syndrome of bilirubin-induced neurologic dysfunction. Semin Fetal Neonatal Med 20, 6–13 (2015).
[8] Soorani-Lunsing I, Woltil HA, Hadders-Algra M: Are moderate degrees
of hyperbilirubinemia in healthy term neonates really safe for the brain?
Pediatr Res 50:701-705, 2001
[9] Jangaard KA, Fell DB, Dodds L, et al: Outcomes in a population of
healthy term and near-term infants with serum bilirubin levels of or 325 micromol/L (or19 mg/dL) who were born in Nova Scotia, Canada, between 1994 and 2000. Pediatrics 1:119-124, 2008
[10] Korkmaz, A., Yiğit, S., Firat, M. & Oran, O. Cranial MRI in neonatal hypernatraemic dehydration. Pediatr Radiol 30, 323–325 (2000).
[11] Burns, C. M., Rutherford, M. A., Boardman, J. P. & Cowan, F. M. Patterns of cerebral injury and neurodevelopmental outcomes after symptomatic neonatal hypoglycemia. Pediatrics 122, 65–74 (2008).
[12] Seske, L. M., Merhar, S. L. & Haberman, B. E. Late-Onset Hypoglycemia in Term Newborns With Poor Breastfeeding. Hosp Pediatr 5, 501–504 (2015).
[13] Fed is Best Feeding Plan: http://fedisbest.org/resources-for-parents/feeding-plan/
[14] AAP SECTION ON BREASTFEEDING. Breastfeeding and the Use of Human Milk. PEDIATRICS 129, e827–e841 (2012).
[15] Uras, N., Karadag, A., Dogan, G., Tonbul, A. & Tatli, M. M. Moderate hypernatremic dehydration in newborn infants: retrospective evaluation of 64 cases. J. Matern. Fetal. Neonatal. Med. 20, 449–452 (2007).
[16] Dewey, K. G., Nommsen-Rivers, L. A., Heinig, M. J. & Cohen, R. J. Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics 112, 607–619 (2003).
[17] Ben, X.-M. Nutritional management of newborn infants: Practical guidelines. World Journal of Gastroenterology 14, 6133 (2008).
[18] Sarici, D. et al. Investigation on malondialdehyde, S100B, and advanced oxidation protein product levels in significant hyperbilirubinemia and the effect of intensive phototherapy on these parameters. Pediatr Neonatol 56, 95–100 (2015).
[19] Kuzniewicz, M. W., Greene, D. N., Walsh, E. M., McCulloch, C. E. & Newman, T. B. Association Between Laboratory Calibration of a Serum Bilirubin Assay, Neonatal Bilirubin Levels, and Phototherapy Use. JAMA Pediatr 170, 557–561 (2016).
[20] Janet H. Muri, et al. From the American Hospital Association: Reducing Avoidable Obstetrical and Neonatal Readmissions http://www.aha.org/content/11/PerinatalReadmissionscall1.pdf
[21] Olusanya, B. O., Osibanjo, F. B., & Slusher, T. M. (2015). Risk Factors for Severe Neonatal Hyperbilirubinemia in Low and Middle-Income Countries: A Systematic Review and Meta-Analysis. PLoS ONE, 10(2), e0117229.
[22] Ben XM. Nutritional management of newborn infants: practical guidelines. World
J Gastroenterol. 2008 Oct 28;14(40):6133-9.
[23] Gidrewicz DA, Fenton TR. A systematic review and meta-analysis of the nutrient content of preterm and term breast milk. BMC Pediatr. 2014 Aug
30;14:216.
[24] Neville MC, Keller R, Seacat J, Lutes V, Neifert M, Casey C, Allen J, Archer
P. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am J Clin Nutr. 1988 Dec;48(6):1375-86.
[25] Neville MC, Keller R, Seacat J, Lutes V, Neifert M, Casey C, Allen J, Archer
P. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am J Clin Nutr. 1988 Dec;48(6):1375-86.
[26] Lee S, Kelleher SL. Biological underpinnings of breastfeeding challenges: the
role of genetics, diet, and environment on lactation physiology. Am J Physiol
Endocrinol Metab. 2016 Aug 1;311(2):E405-22. doi: 10.1152/ajpendo.00495.2015.
Epub 2016 Jun 28.
[27] Watkins S, Meltzer-Brody S, Zolnoun D, Stuebe A. Early breastfeeding
experiences and postpartum depression. Obstet Gynecol. 2011 Aug;118(2 Pt
1):214-21. doi: 10.1097/AOG.0b013e3182260a2d. PubMed PMID: 21734617.

2 thoughts on “Exclusively Breastfed Newborns Have Double the Risk of Being Rehospitalized”