Christie del Castillo-Hegyi, M.D. and Jody Segrave-Daly, RN, IBCLC
We at the Fed Is Best Foundation give mothers across the globe a platform to tell their stories about how their babies suffered needlessly because they were denied information and supplementation for their hungry babies while under the care of the Baby-Friendly Hospital Initiative/WHO Ten Steps to Successful Breastfeeding protocol. Our Foundation has grown rapidly and demands significantly more time than we currently have because we are a 100% volunteer organization. We are inundated with messages from mothers, health professionals and media on a daily basis. We try very hard to prioritize what we can do collectively, every single day. Our first priority is to respond to mothers in crisis who contact us needing assistance on how to safely feed their distressed breastfed baby because they were not educated on appropriate supplementation. Baby Friendly USA (BFUSA) found time to critique our interpretation of studies and written materials, so we were forced to take time away from mothers to update written materials and clarify our interpretations. Our goal is to be completely transparent and we have provided our detailed response below with corrections and clarifications given publicly available published data. If there have been errors in interpretation of published information, then we go back to the original published data to provide better data for the public, which we have done below. We believe we have a responsibility to inform parents, the public, medical insurance companies and BFHI hospitals about the risks of exclusive breastfeeding when insufficient. We believe parents deserve to know that the BFHI has an exclusive breastfeeding (EBF) threshold mandate to meet if the hospital wants to remain credentialed. The mandate results in tens of thousands of newborn admissions every year in the U.S. alone, which we chronicle on our page. For the safety of infants across the globe, we will continue to provide education on how to recognize serious complications of exclusive breastfeeding and how every parent can prevent them.
Starvation jaundice (hyperbilirubinemia) of the newborn is defined as abnormally high bilirubin in a newborn who loses >8-10% weight. It is caused by insufficient elimination of bilirubin due to insufficient caloric intake from exclusive breastfeeding in the first week of life. This well-established phenomenon has been discussed by neonatologist Dr. Lawrence Gartner, who is listed as a Director on the Baby-Friendly USA website, in a lecture given to lactation consultants (not just physicians and nurses as stated by BFUSA) at a 2013 California Breastfeeding Conference, previously posted on their website. This public lecture was provided to educate lactation consultants regarding dangerous levels of jaundice that can occur in previously healthy breastfed babies that result from inadequate intake of calories from exclusive breastfeeding. Under Fair Use laws, dissemination of educational material for non-profit educational purposes is protected and we were subsequently asked to post the full lecture by Dr. Gartner via email. The Academy of Breastfeeding Medicine jaundice protocol acknowledges that exclusively breastfed newborns are at higher risk of hyperbilirubinemia from insufficient milk intake (“suboptimal intake”) and excessive weight loss. The vast majority of newborn hyperbilirubinemia is caused by starvation jaundice. Their protocol also states that 98% of kernicterus, or the most severe form of brain injury from jaundice, occurs in breastfed newborns. Nearly all of starvation jaundice can be prevented with timely and adequate supplementation. Nearly all newborns with starvation jaundice show signs of poor feeding including excessive crying and frequent, unsatisfied nursing or lethargy before they develop levels of hyperbilirubinemia that result in impaired brain development. While BFUSA has not previously denied the increased risk of hyperbilirubinemia in breastfed newborns, they have not routinely disclosed them to parents or subscribing hospitals, which has the unfortunate effect of causing hospitalizations that would have been prevented by supplementing a crying underfed newborn. Unfortunately, many parents and health professionals are taught that the signs of poor feeding including crying and hours of unsatisfied nursing are normal, widely known as the “Second Night Syndrome.” These unfortunately are also the earliest signs of other complications like acute bilirubin encephalopathy, kernicterus, hypernatremic dehydration and hypoglycemia, all known causes of brain injury and permanent disability, which can occur if those signs are overlooked as normal and supplementation is avoided in order to meet the goal of exclusive breastfeeding.
California has a state mandate to require Baby-Friendly certification in all its hospitals by 2020, which require that 80% of eligible newborns be exclusively breastfed at discharge, the primary quality metric of the BFHI. Many California hospitals are working toward that designation and their exclusive breastfeeding rates at discharge are tracked by the California Department of Public Health. Among those hospitals were hospitals in the Kaiser Permanente system (although multiple Kaiser hospitals in Southern California appear to have recently relinquished their designation). Estimates of excessive jaundice in the Kaiser Permanente Northern California hospital system, which has among the highest exclusive breastfeeding rates at discharge, all except 2 reaching >80%, was published in JAMA Pediatrics in 2016, which showed that an astonishing 12% of newborns developed hyperbilirubinemia of >15 mg/dL. [Corrected 8/31/2018] Out of 104,428 newborns, that would have been 12,949 newborns (almost 12 babies a day) who developed significant hyperbilirubinemia. Among those newborns were 5.7% or 5952 newborns (5 babies a day) who required phototherapy. By comparison, a recently published article in the journal Neonatology showing the effects of supplementing breastfed newborns with oral glucose and formula to satisfaction yielded a neonatal hyperbilirubinemia rate of 1.3% and a phototherapy rate of 0.3%.
Another estimate of hyperbilirubinemia rates comes from a review published by leading jaundice investigator, Dr. Vinod Bhutani who estimates that severe jaundice rates (>17 mg/dL, >95th %ile) is 8 -10%, or 1 in 10 newborns. Severe jaundice is a known cause of more subtle brain injury and impairments in brain development called Bilirubin-Induced Neurological Disorder.
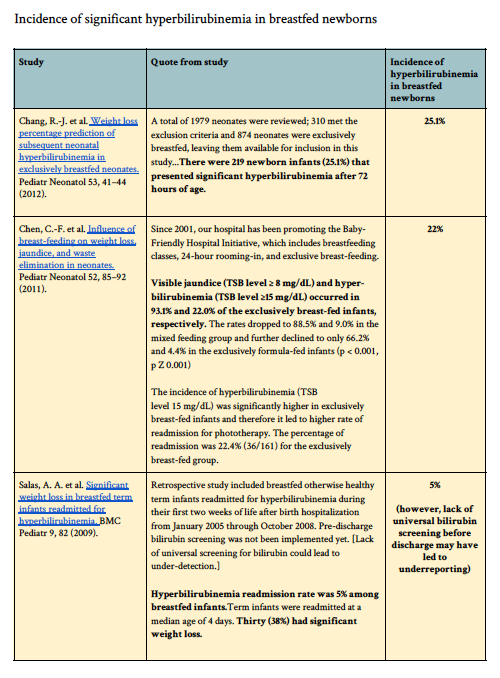
We have provided all the published data available through PubMed on rates of hyperbilirubinemia among breastfed newborns worldwide, which included hyperbilirubinemia rates as high as 35%.
In addition, among healthy, term exclusively breastfed newborns, 10% of vaginally-delivered newborns and 25% of cesarean-delivered newborns in this same hospital system lost >10% of their birth weight. In contrast, 7 out of 7075 formula-fed newborns lost >10% (0.1%) from another study at the same hospital system. [Corrected 8/31/2018]. This yields a minimum of a 100-fold increased rate of excessive weight loss in exclusively breastfed newborns. Given the serious complications associated with weight loss > 7% including hypernatremia and hyperbilirubinemia, this is an unacceptable complication rate among newborns experiencing the Baby-Friendly protocol.
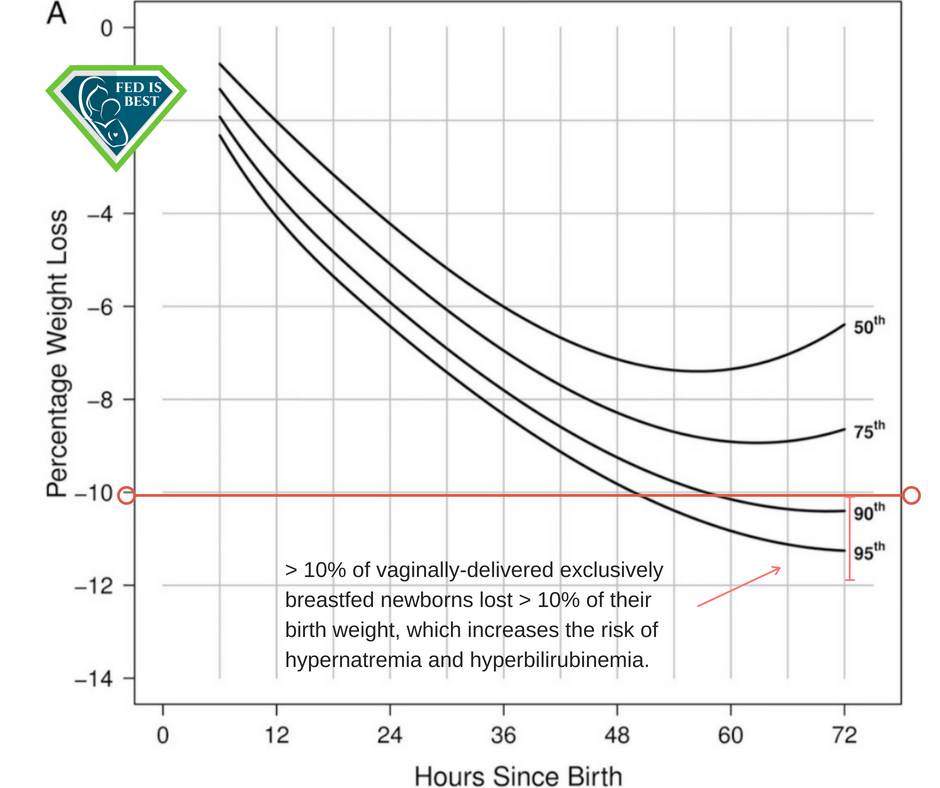
Flaherman et al, Early Weight Loss Nomogram of Exclusively Breastfed Newborns, Figure 2A, Pediatrics, Jan 2015.
Failing to disclose the increased risk of hyperbilirubinemia and dehydration from early exclusive breastfeeding and the risks of developmental disabilities from such complications is unsafe and irresponsible. If Baby-Friendly USA truly believes in providing mothers accurate information, they should start off with telling them the most vital information required to protect their child’s safety, health and future potential. Namely, that:
- Insufficient breast milk, particularly in the first days of life is common.
- Persistent crying and nursing are signs of hunger, thirst and insufficient feeding.
- Insufficient feeding of breast milk or formula can result in complications like dehydration, hyperbilirubinemia and hypoglycemia that require hospitalization and can result in brain injury, disability and death.
- Supplementation with safe, laboratory tested donor milk and/or formula to satisfaction can correct and prevent serious and irreversible outcomes.
We ask Baby-Friendly USA to act responsibly, prioritize patient safety and publicly acknowledge the known risks of insufficient feeding from exclusive breastfeeding to all its subscribing hospitals, health professionals and the public. Disclosing these risk, the signs and consequences of breastfeeding complications to parents is the only way to eliminate breastfeeding tragedies given that these complications commonly occur at home shortly after discharge. We ask BFUSA to refrain from encouraging subscribing hospitals to dismiss reports of patient harm as spurious complaints coming from the Fed is Best Foundation, which they have done on their website. Examining cases of patient harm are vital to ensuring patient safety. We also ask that you correct the posts on your website accurately reflecting that we have invited you to a video-recorded web conference to discuss breastfeeding complications, an invitation which you have not accepted. Finally, we ask that you acknowledge the errors you have made in interpretation of data including the weight loss data above, the rates of insufficient breast milk in the first days of life, the size of the newborn stomach, the nutritional content of colostrum, the metabolic and neurological consequences of feeding newborns less than their requirement for several days, the meaning of crying in such newborns, the effects of supplementation on breastfeeding rates from the Cochrane Review data, which was used in the 2017 WHO guidelines, and many, many more vital concepts of infant feeding required to ensure patient safety.
To BFUSA’s request: We stand corrected. The most current estimate of newborn jaundice among exclusively breastfed newborns is not 10-18%, it is 5-33%. [Corrected 8/31/2018]
Unfortunately, more current and more accurate data is not available as BFUSA does not publish its complication rates.
ABM Revised Jaundice Protocol:
https://abm.memberclicks.net/…/22-jaundice-protocol-english…
To read our full account of data on rates of hyperbilirubinemia (jaundice) and phototherapy admissions in a Baby-Friendly-Compliant Hospital System, Kaiser Permanente Northern California, please read the updated blog, “High Rates of Newborn Hospitalizations for Jaundice Requiring Phototherapy in a Baby-Friendly-Compliant Hospital System.”


One thought on “Response to Baby-Friendly USA Regarding Rates of Hyperbilirubinemia Among Exclusively Breastfed Newborns”