by Christine K.
When the Fed Is Best Foundation launched two years ago, a few nurses sent us messages about their experiences working in a Baby-Friendly Hospital Initiative (BFHI) hospital. They shared common concerns about watching exclusively breastfed babies crying out in hunger from not enough colostrum while being refused supplementation just so that high exclusive breastfeeding rates were met. Two years later, we now receive messages from nurses, physicians, lactation consultants, and other health professionals, regularly. They express their concerns while asking for patient educational resources. They tell us their stories and they need support and direction on what to do about unethical and dangerous practices they are forced to take part in. We collected their stories and are beginning a blog series on health professionals who are now speaking out about the Baby-Friendly Health Initiative (BFHI) and the WHO Ten Steps of Breastfeeding.
Christine K. is a Neonatal Nurse Practitioner currently working in a BFHI Hospital with 25 years of experience. She has worked in both BFHI and non-BFHI hospitals and talks about her concerns about taking care of newborns in the Baby-Friendly setting.
Regarding Unsafe Skin-To-Skin Practices
In BFHI facilities, skin-to-skin is mandated. The protocol calls for skin-to-skin at birth, for the first hour, then ongoing until discharge. New mothers are constantly told that it is important for bonding, for breastfeeding, for milk production and for temperature regulation of the newborn. Baby baths are delayed for skin-to-skin time and nurses are required to document in detail the skin-to-skin start and end times. There is no education on safety regarding skin-to-skin time, only that it is to be done. I have been responsible for the resuscitation of babies who coded while doing skin-to-skin. One died, and the other baby is severely disabled. Mothers are not informed of the risks of constant and unsupervised skin-to-skin time. Mothers have complained to me that they felt forced to do skin-to-skin to warm up their cold or hypoglycemic infant because they are told skin-to-skin time will help their infant resolve these issues when in fact it doesn’t. There is also no assessment of the mother’s comfort level with constant skin-to-skin. It’s very discouraging to hear staff say things like, “That mother refused to do skin-to-skin,” like it was a crime or an act of child abuse. The judgment is harsh on mothers who fail to follow the protocol. I have noticed that partners are pushed to the side, especially in the first hour of life, not being able to hold their newborn, due to this strict policy. Their involvement has been discounted in the name of the exclusive breastfeeding protocol.
Breastfeeding Education and Support
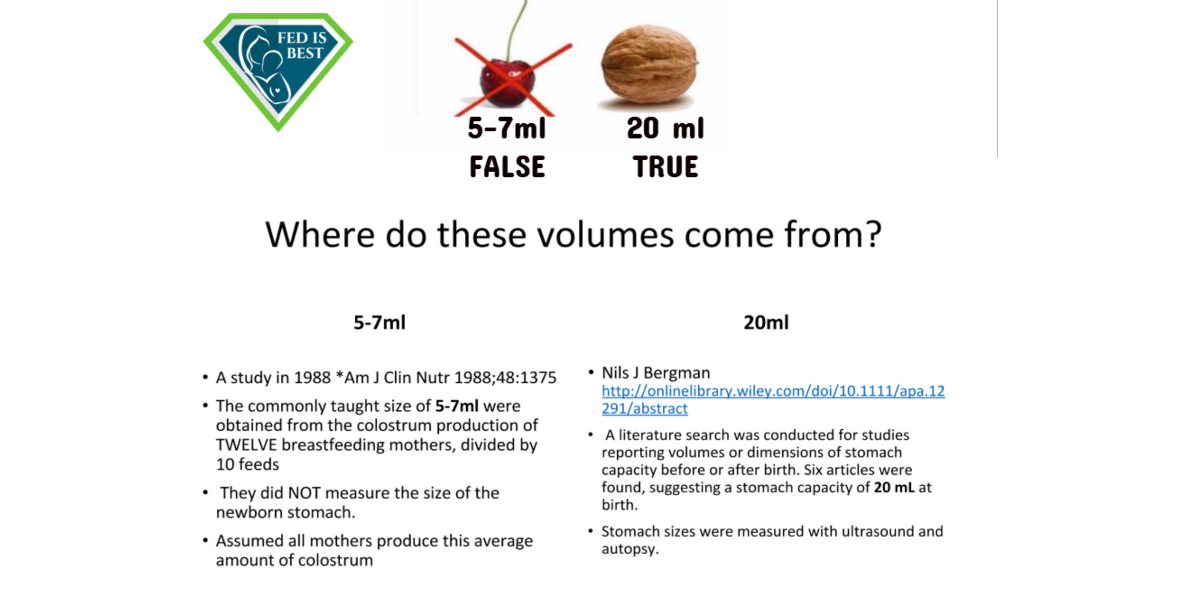
In the BFHI facility, breastfeeding is assumed on the admission of a laboring patient. If a mother says she wants to combo- or formula-feed then the nurse has memorized a BFHI script, given to them by the administration to change the mother’s mind. Education is provided to mothers on the ‘risks’ of formula-feeding and the benefits of breastfeeding. Cultural preferences are ignored; personal choices that don’t conform are demeaned; partner involvement is nearly eliminated. The lactation department, who are tasked with keeping the exclusive breastfeeding rates at > 80% at all times become aggressive to meet the thresholds. Lactation support teams are required to be anti-pacifier, anti-supplement, and anti-artificial nipple, without exception. They point out why these things are “harmful” and how they can destroy the breastfeeding relationship, even when they contradict current research and evidence-based medicine.
Lactation department meetings are held to talk about strategies to change a mother’s mind in order to get her to breastfeed, even if it’s just for the twenty-four hours in the hospital. Then they can document higher breastfeeding rates to report to the state.
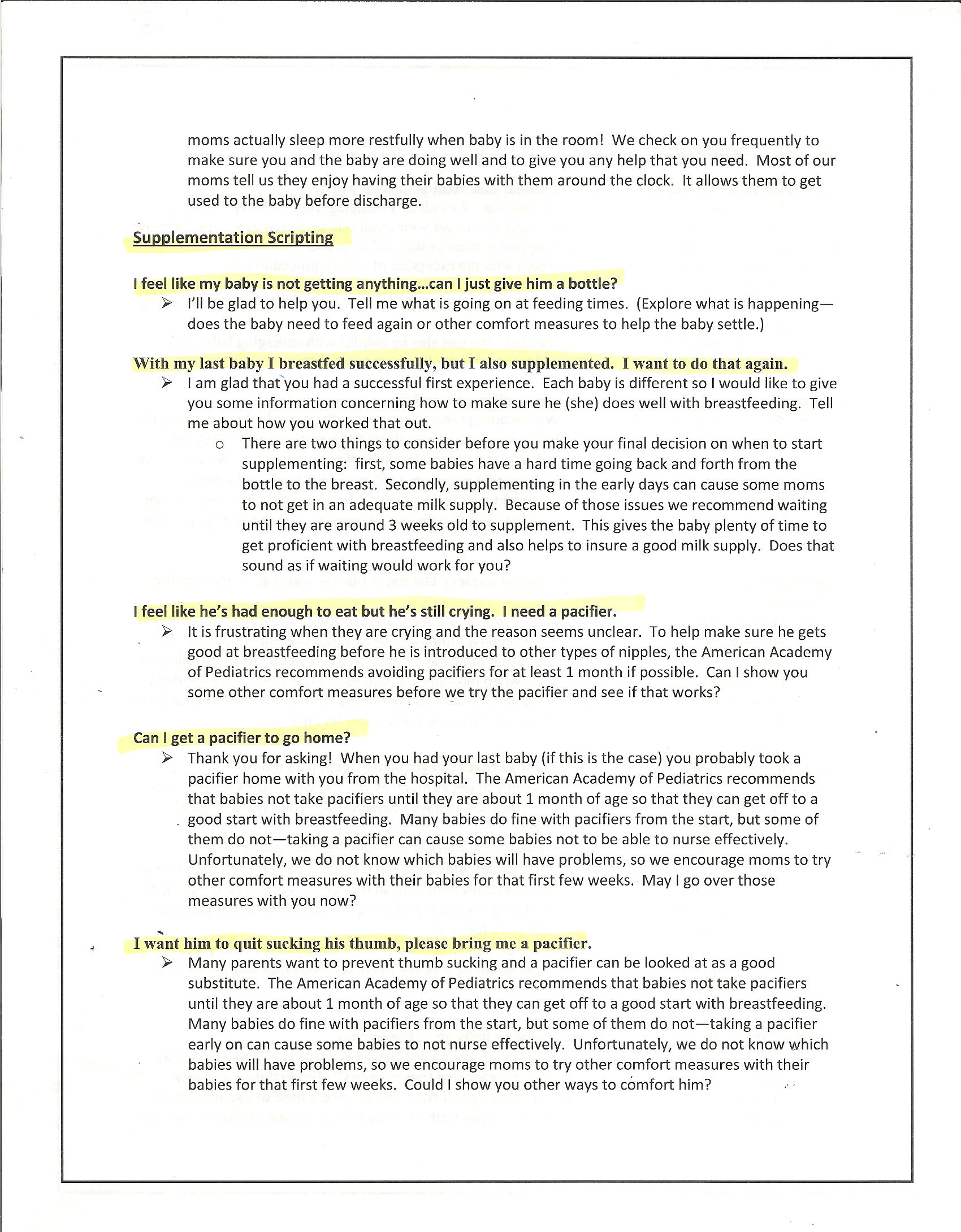
Text examples of how nurses are supposed to respond to mothers.
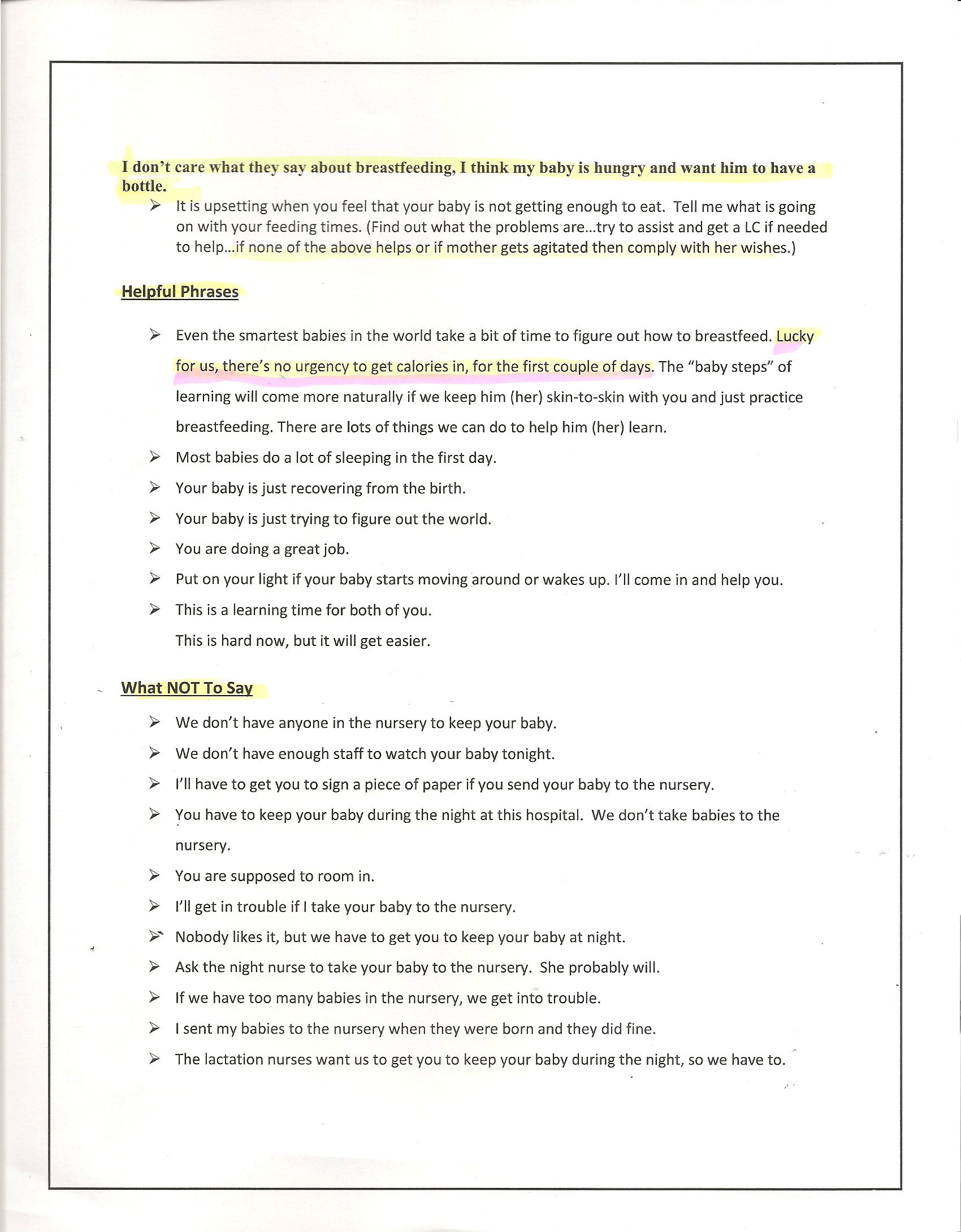
My experience has been that the lactation department is weak in current, evidence-based medicine and prefer to rely on outdated resources. They will grasp onto any mommy blog, opinion article, or poorly designed science article that is flat-out wrong, but very dangerous to mothers and newborns. A perfect example is the belly ball stomach size picture. This is a favorite mantra of lactation departments across the country. They use data based on a completely unscientific study from nearly 30 years ago, to support their claim on the infant stomach size. They continue to preach this information despite it being proven false through numerous studies and clinical data. Why? Because as long as they can say newborn stomach sizes are tiny they can continue to limit the intake of newborns who are displaying signs of ongoing hunger and maintain their 80 percent exclusive breastfeeding rates.
It shocks me that mothers are not asked about their previous nursing experiences or risk factors for delayed milk production, breastfeeding difficulties or milk supply issues. I’ve had mothers break down in tears telling me how horrible their last experience, many developing postpartum anxiety, depression, and PTSD. But due to the pressure from family, friends, social media and now hospital staff, they’ve decided to try to breastfeed again. I’ve had mothers break down in tears when I tell them it’s okay to not breastfeed, that their choice is valid and that it doesn’t need to be validated by anyone, ever.
On Formula Feeding Education
Mothers who request formula for any reason are required mandatory education about the risks of formula feeding that are not accurate. Bottle nipples are often limited to “slow flow” to make the baby “work for his food, like breastfeeding.” I have seen nurses empty bottles, leaving only 5 or 10 ml, so that parents don’t “overfeed” their baby and ‘stretch out’ their stomachs, which supports the belly ball model ‘theory’.
Formula shaming comes in many forms. New mothers are told that formula makes babies spit-up, gives them gas, makes their stomach hurt and that their stools will smell worse than breast milk. These subtle and negative references to formula are degrading to mothers, some of whom have no choice in the way they feed their babies.
Discharge Education
Babies are commonly discharged at 24 hours and the highest risk time for breastfeeding complications are on days 2-4, sometimes before they even see a pediatrician. Mothers are not taught anything about supplementing if the mother’s milk doesn’t come in, which puts their babies at risk for rehospitalization. For babies who are formula-fed, parents are not told to increase the formula intake daily, or formula-feed on-demand until satisfied. Formula-fed babies are also at risk for underfeeding because parents are told the infant stomach size is a teaspoon.
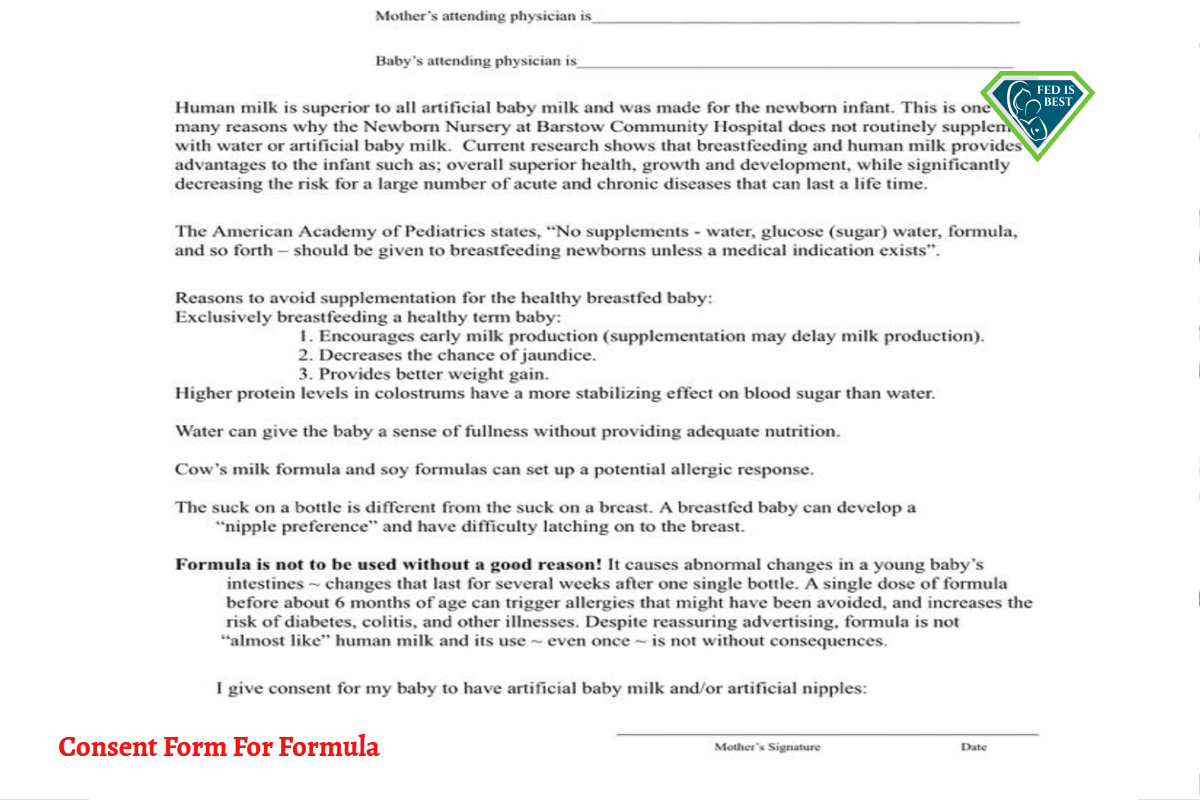
Some mothers must sign a consent form to supplement.
Maternal Exhaustion, Recovery from Surgery and Newborn Care
I think with the loss of nurseries, both non-BFHI and BFHI hospitals have placed newborn care onto parents from the moment the baby delivers. Babies are born, then to belly for skin-to-skin. Skin-to-skin happens in the operating room while they are still closing up the incision on the mother, then skin-to-skin for the 2 hr recovery time. Then they go straight to the room, where mothers are expected to care for their infant.
No one gets a pass with baby care, even if a mother had a 3 day induction, has pregnancy-induced hypertension (PIH) and is on magnesium, 6 hours of pushing, crash c-section, third degree tear, 1000 ml blood loss, postpartum hemorrhage. It. Does. Not. Matter.
The partner or someone else has to stay to help care for the baby when mothers are recovering. When mothers need pain medication, they are told to not take too much because they are breastfeeding and it can cause them to be drowsy. But if the mother needs it, partners are coached to hold the baby to the mother’s breast while nursing or do hand expression while mothers are struggling to stay awake. If the mother is dangerously exhausted and asks to supplement her baby, the nurses are required to educate her once more about the dangers of supplementing their babies. She is told to be patient for her milk to come in no matter how much her baby is crying from hunger. They are told that colostrum is all they need no matter how much her baby is showing the opposite.
Common Clinical Situations
The most common encounters that I see with exclusively breastfed babies during their hospital stay are the complications of not receiving enough colostrum.
It is very common to hear frantically crying babies on the mother-baby units because they are hungry and are not satisfied from breastfeeding.
This happens every single shift I work.
Mothers are told their babies have ‘the second night syndrome‘ and that this is normal newborn behavior. At times, I will admit exclusively breastfed babies for hypoglycemia (low blood sugar) after failed supplemental feeding trials. These babies failed to get adequate calories and fluid at the breast. Often they should have been admitted much sooner, but the drive is to keep them with their mother and nursing. These babies have suffered hours of hypoglycemia, which causes brain injury every minute it is left untreated.
I also admit babies for phototherapy to treat excessive jaundice who have no risk factors beyond excessive weight loss and exclusive breastfeeding. Weight loss at 24 hours of 5-9 percent is common for at least 70 percent of our exclusively breastfed babies.
Ironically, those babies who require medical intervention and are allowed to feed on demand will demonstrate strong hunger signs and take supplemental feedings eagerly. And it’s far more than teaspoons of milk. Even if they need IV fluids, being more hydrated and having normal blood sugars helps the infant to breastfeed much better. We feed babies based on their weight, usually about 60-80 ml/kg/day (typically 15-30 ml) every 2-3 hours. When allowed to feed on demand, newborns will typically take the increased volumes eagerly and demonstrate feeding satisfaction and comfort.
Conversely, there are mothers who are so entrenched in their belief that formula is toxic, that they will continue to deny any risks or dangers of starving their newborn and refuse to supplement even when it is medically required.
I’ve also had mothers admit to sneaking in formula to supplement their babies for fear of it being denied.
Here’s the reality of it all. The BFHI drives hospitals to ignore a mother and newborn infant’s basic human needs, ignore cultural preferences, and shame mothers if they can’t or chose to not breastfeed.
Underneath all of this, a driving force in medicine is the dreaded DRGs and hospital bed turnover. [A DRG, or diagnostic related grouping, is how Medicare and health insurance companies categorize hospitalization costs and determine how much to pay for a patient’s hospital stay.] Gone are the days of resting and recovering from your delivery. Hospitals are now driven by turn-over and keeping beds full. Vaginal deliveries are out in twenty-four hours, C-sections are out on day 2 because every admission is reimbursed the same amount and every additional day in the hospital reduces the hospital’s net reimbursement. Infant weight loss, latch effort, and feeding competence are not factored into this financial equation and can be dealt with outpatient in the primary care provider’s office. Jaundice can be rechecked on follow-up outpatient exams. Turnover is critical.
Do they worry about readmissions? Typically, no, as this doesn’t factor into the initial hospital stay payment system and I would be surprised if many hospitals even tracked the outcomes of their mother/newborn patient population. How many mothers don’t show up at the follow-up appointments? How many mothers and babies end up in the emergency room? How many extra doctor’s office visits were required to monitor breastfeeding complications in babies with risk factors that were present at the time of discharge?
Do they worry about a baby who may have developed hypoglycemia or jaundice severe enough to cause brain injury before they even see their pediatrician? No, because those fall under different billing codes and can be billed with better reimbursement as outpatients.
It’s a battle every day to safely feed our babies. A battle for the nurses. A battle with the lactation team who wants every single baby to breastfeed while in the hospital, regardless of their mother’s choice. A battle with the administration to look beyond exclusive breastfeeding statistics and see the harm caused by the BFHI policies. And yes, sometimes a battle with mothers who resist any intervention because “breast is best.”
Why do mother’s follow the hospital guidelines, ignore their gut instinct that their baby is hungry, and follow a hospital lactation plan that is contrary to what they planned for nine months of their pregnancy? Because they have been pushed and pressured into believing that if they don’t follow these guidelines they will have failed as a mother. And who wants to feel like a failure as a new mother?
For the most part, I feel many staff and providers are now trying to do their best to give excellent care, to keep mothers and babies safe, and to discharged families home in a safe manner, all the while flying under the administration’s radar.
How did we reach this point in a first-world society with advanced medicine?
We have a private and secure Face book group for licensed health professionals who are interested in learning more about our advocacy. Please contact us at contact@fedisbest.org
References:
What Happens When Mothers Are Told Being Fed Is The Bare Minimum?
Why is the American Academy of Pediatrics exaggerating the benefits of breastfeeding?
Breastfeeding Benefits: The Real, the Imagined, and the Exaggerated
https://www.sciencedaily.com/releases/2018/09/180925150440.htm
http://pediatrics.aappublications.org/content/138/3/e20161889
https://thescientificparent.org/recent-reports-of-skin-to-skin-benefits-fail-to-mention-key-infant-safety-risks/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3599160/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3599160/
http://pediatrics.aappublications.org/content/137/1/e20152238
My Baby Starved at Kaiser Permanente – I Was Told Her Stomach Size Was Only 5 mL
My Three Day Old Baby Went Limp And Turned Blue; She Was Starving And I Almost Lost Her
The Scientific Evidence on the Effects of Underfeeding on the Newborn Brain
http://fedisbest.org/resources-for-parents/second-night-syndrome-abnormal/
http://fedisbest.org/resources-for-parents/starvation-jaundice-risk-factors-prevention/
Markers of Brain Injury is Present in the Blood of Newborns Requiring Phototherapy for Jaundice
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
Letter to Doctors and Parents About the Dangers of Insufficient Exclusive Breastfeeding
If I Had Given Him Just One Bottle, He Would Still Be Alive.
HOW YOU CAN SUPPORT THE FED IS BEST FOUNDATION
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and every thing in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going. Thank you for your advocacy!



One thought on “Neonatal Nurse Practitioner Speaks Out About The Dangerous Practices Of The BFHI”