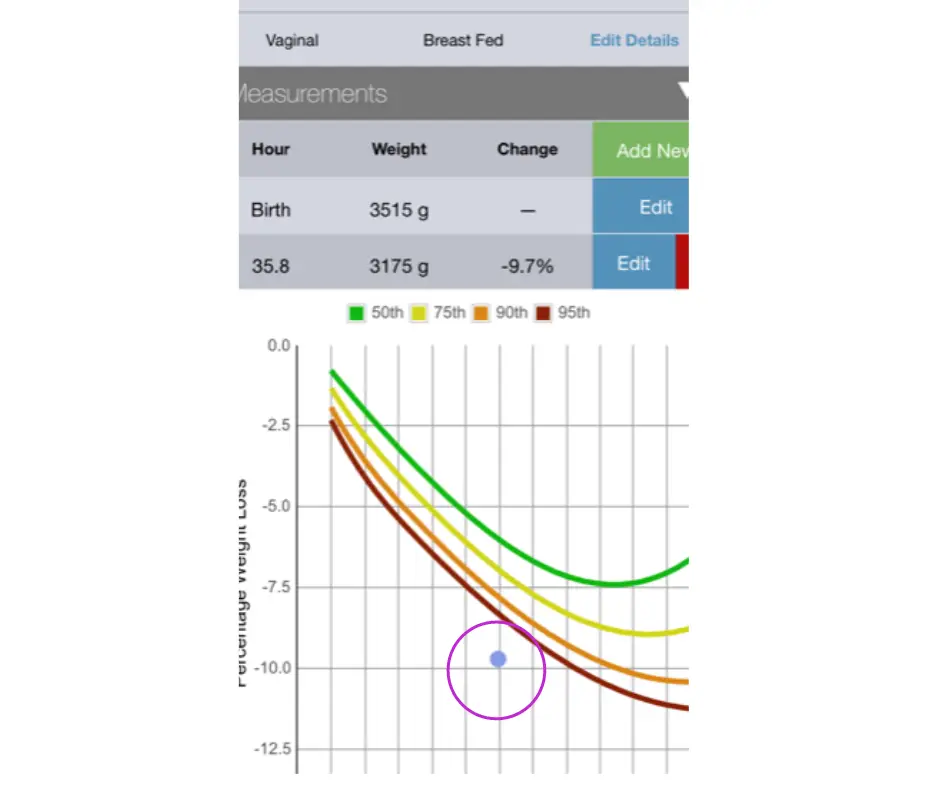
The Newborn Weight Loss Tool can provide an answer.
Parents are taught that it’s normal for babies to lose 7–10% of their body weight in the first few days after birth, but is this true? Well, that depends. According to the AAP, a baby who loses more than 7% of his body weight may be losing excessive weight and requires a comprehensive lactation evaluation to rule out delayed onset of copious milk production, primary lactation failure, and/or infant oral anomalies that prevent adequate colostrum/milk transfer.

From the American Academy of Pediatrics HealthyChildren.org website. Breastfed newborns should lose no more than 7 percent of birth weight in the first few days after birth before starting to gain weight again. (Accessed July 16, 2020)
Weight loss has typically been assessed using simple percentages, but now there is a much more precise and accurate way to track excessive weight loss in newborns and many hospitals, pediatricians, and lactation consultants are adopting this method for greater accuracy in making clinical recommendations. The Newborn Weight Tool, or NEWT, is an online tool, the first of its kind, to help pediatricians determine whether exclusively breastfed newborns have lost too much weight in the first days of life. The tool was developed at Penn State College of Medicine through research conducted jointly with University of California, San Francisco. It was developed using a research sample of hourly birth weights from more than 100,000 breastfed newborns. For a quick synopsis of this tool from the lead investigator and one of developers of the tool, Dr. Ian Paul, watch the video below.
Source: Penn State Health News
In this video, Dr. Ian Paul, professor of pediatrics and public health sciences at Penn State College of Medicine and pediatrician at Penn State Hershey Children’s Hospital, talks about how NEWT fills an important void. Determining whether an exclusively breastfed newborn is losing excessive weight is important because higher weight loss almost always reflects suboptimal milk intake. It is also associated with increased risk of medical complications such as low blood sugar, jaundice, and dehydration, which can result in the need for medical interventions and future health and developmental problems. This weight-loss tool shows that how quickly babies lose weight is just as important as how much they lose.